Abstract
Background
Utero-vaginal brachytherapy (BT) is an irreplaceable care component for the curative treatment of locally advanced cervix cancer (LACC). Magnetic Resonance Imaging (MRI)-image guided adaptive BT (IGABT) using the GYN-GEC-ESTRO EMBRACE guidelines is the international care standard. Usually following chemo–radiation therapy (CRT), IGABT has high proven utility in LACC but requires significant health system resources. Timely access was disrupted by the COVID-19 pandemic which challenged us to re-design our established IGABT care pathway.
Methods
From April 2020 consecutive patients with LACC were enrolled after CRT in a single arm exploratory non-inferiority study of a modified IGABT (mIGABT) protocol. This delivered an iso-effective IGABT dose (39.3 Gy: EQD2: α/β10Gy concept) over a 24-h period during a single overnight hospitalisation.
Results
Fourteen LACC patients received mIGABT from April 2020 to March 2022. Median age was 62.5 years (37–82 years). LACC histology was primary squamous (9/14) or adeno-carcinoma (5/14). International Federation of Gynaecology and Obstetrics (FIGO) 2018 stages ranged from IB1/2 (N = 3), IIA1/IIB (5), IIIB (2), IIIC1/2 (4) with mean ± standard deviation (SD) gross tumour volume-at-diagnosis (GTV_D) of 37.7 cc ± 71.6 cc. All patients achieved complete metabolic, clinical, and cytologic cancer response with CRT and IGABT. High-risk HPV was cleared by 6-months. Complete MRI-defined cancer response before mIGABT (GTV_Fx1) was seen in 77% of cases (10/13). Only two women developed metastatic disease and one died at 12-months; 13 patients were alive without cancer at mean 20.3 ± 7.2 months follow-up. Actuarial 2-year overall survival was 93%. Compared with our pre-COVID IGABT program, overall mIGABT cost-saving in this cohort was USD 22,866. Prescribed dose covered at least 90% (D90) of the entire cervix and any residual cancer at time of BT (HRCTV_D90: high-risk clinical target volume) with 3-fractions of 8.5 Gy delivered over 24-h (22.8 ± 1.7 h). Total treatment time including CRT was 38 days. The mIGABT schedule was well tolerated and the entire cohort met EMBRACE recommended (EQD2: α/β10Gy) combined HRCTV_D90 coverage of 87.5 ± 3.7 Gy. Similarly, organ-at-risk (OAR) median: interquartile range D2cc constraints (EQD2: α/β3Gy) were EMBRACE compliant: bladder (65.9 Gy: 58.4–72.5 Gy), rectum (59.1 Gy: 55.7–61.8 Gy), and sigmoid colon (54.6 Gy: 50.3–58.9 Gy). ICRU recto-vaginal point dose was significantly higher (75.7 Gy) in our only case of severe (G4) pelvic toxicity.
Conclusions
This study demonstrated the utility of mIGABT and VMAT CRT in a small cohort with LACC. Loco-regional control was achieved in all cases with minimal emergent toxicity. Single insertion mIGABT was logistically efficient, cost-saving, and patient-centric during the COVID-19 pandemic.
Similar content being viewed by others
Background
In 2020 the United Nations International Agency for Research on Cancer ranked invasive cervix cancer 4th after female breast, lung, and colorectal cancer in both annual incidence and mortality with approximately 60% of those diagnosed worldwide (342,000/604,127 women) dying of the disease [1]. Standardised cervix cancer mortality rates were 2.5 times higher in low and middle income countries (LMIC) [2]. Reducing poverty and developing sustainable Public Health initiatives that prioritise primary prevention using high-risk Human Papillomavirus (hr-HPV) vaccination [3, 4], and secondary surveillance strategies, are exigent to improving global outcomes as most patients present with locally advanced (inoperable) cervix cancer (LACC) [1,2,3,4,5].
LACC demands reliable access to integrated external beam chemo–radiation therapy (CRT) and utero-vaginal brachytherapy (UVBT) for cure [4,5,6,7,8,9,10,11,12,13,14,15]. UVBT is deemed an “irreplaceable” or critical component of care [16, 17], but UVBT is often non-existent, difficult to access, or without fidelity in many LMIC [2, 4, 6]. Underuse of UVBT is a major determinant for poorer cervix cancer treatment outcomes in all economic settings [2, 4, 18].
In March 2020, the novel Coronavirus disease 2019 (COVID-19) pandemic acutely disrupted cancer services in high income countries such as Australia. Access delays to UVBT imposed by the pandemic temporally mimicked some of the global realities of LACC in our practice [19,20,21,22,23,24,25].
In 2008, the Gynaecological Groupe Européen de Curiethérapie—European Society for Radiotherapy and Oncology (GYN GEC-ESTRO) began the prospective International study of image guided intensity modulated External beam radiotherapy and Magnetic Resonance Imaging (MRI) based adaptive Brachytherapy in locally Advanced Cervical cancer (EMBRACE-I) study. EMBRACE-I proposed multi-fraction 4-dimensional MRI-image guided adaptive brachytherapy (IGABT) after CRT [26] according to institutional tradition. This MRI volume-based prescription, recording, and reporting method has become the consensus international brachytherapy care standard in LACC [27].
Our EMBRACE-I IGABT protocol however, was logistically complex and resource intensive. From inception in 2010, our EMBRACE programme [28] was hospital-based and included 2 overnight admissions separated by 7 days modelled on Vienna dose-fractionation [29]. Each in-patient event involved operating room (OR) access and general anesthesia (GA) for ultrasound-guided utero-vaginal applicator insertion and specialised patient-applicator immobilisation. Subsequent transfers throughout the hospital for daily MRI was a precursor to applicator reconstruction, anatomic contouring, dose optimisation and treatment. Contingencies at any level of this repeated process were nominal.
The COVID-19 pandemic imposed sudden access barriers to protect critical Public Hospital infrastructure and key health personnel. Intra-hospital and Inter-departmental patient transfer restrictions to radiology and radiation oncology facilities further disrupted our EMBRACE care pathway.
Faced with these challenges, we developed a pragmatic radio-biological modification of our institutional EMBRACE protocol. Modelled from a compendium of published COVID-19 fractionation options [30,31,32] and a small prospective series [33], a putative bio-equivalent accelerated single insertion 3-fraction modified IGABT (mIGABT) EMBRACE programme was trialled on 14 women with LACC. We report our 2-year progression-free survival (PFS), total cost-saving, and toxicity outcomes.
Methods
This was a single-arm pre-defined exploratory non-inferiority study conducted on 14 consecutive women. All were referred from April 2020 to end-March 2022 with new biopsy-proven HPV-associated LACC. Age < 18 years, cervical neuroendocrine cancer, visceral metastatic disease, and any absolute contraindication to MRI were the only exclusions. COVID-19 post-nasal and throat swabs were polymerase chain reaction (PCR) negative before hospital admission for brachytherapy.
All patients were examined under anaesthesia (EUA) by a radiation oncologist (MJS) and certified gynaecologic oncologist. Speculum findings and the 3-D clinical (palpable) impression of the gross tumour volume (GTV) were recorded. Mandatory radiologic staging included whole body 18Fluoro-deoxyglucose (FDG) Positron Emission Tomography/Computer Tomography (PET/CT) and pelvic 3 T-MRI. Total gross primary tumour volume at diagnosis (GTV_D) and at time of IGABT fraction 1 and 2 (GTV_Fx1 and GTV_Fx2) were derived from T2-weighted 3 T-MRI sequences [14].
The decision to recommend definitive CRT/IGABT was determined by our institutional GYN multi-disciplinary team which convened weekly. The design and rationale of our COVID modified EMBRACE IGABT high dose-rate (HDR) protocol, and the analysis of (de-identified) patient databases was pre-approved by the Northern Sydney Local Health District HREC [LNR/2021/ETH01361].
Demographic characteristics, cancer histologic subtype, and International Federation of Gynaecology and Obstetrics (FIGO) 2018 stage [34] GTV_D, and duration of follow-up of our cohort are summarized in Table 1.
CRT
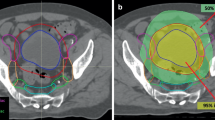
Concurrent 40 mg/m2 intravenous cisplatin (CDDP) was prescribed weekly for maximum 5 cycles. External beam radiation therapy (EBRT) was delivered by dynamic single isocentre volumetric-modulated arc therapy (VMAT) on either Varian TrueBeam® or Halcyon® linear accelerators (Varian Medical Systems: Palo Alto, CA). Daily cone-beam computer tomography (CBCT) provided image guidance. The primary central pelvic planning target volume (PTV_P) included cervix and corpus uteri, parametria, and additional vaginal margin on any gross disease identified on staging MRI. Iodated hydroxyethyl cellulose vaginal contrast (Iopromide 5 cc and K–Y gel® 30 cc agitated in 60 cc catheter tip syringe) was routinely used to delineate the vagina from fornix to introitus during simulation (seen fully in Fig. 1 sagittal view). Figure 1 presents the typical EBRT dose wash in axial and sagittal planes. PTV_P and subclinical iliac/para-aortic lymph node disease (PTV_N) was dosed to 45-50 Gy with simultaneous integrated boost to FDG or MRI-defined gross tumour volume nodal metastases (GTV_N; 55-60 Gy) in 25 daily fractions (1.8–2.4 Gy/day). PTVs were expanded by 0.7 cm from primary and nodal clinical target volumes (CTV_P and CTV_N), respectively [7]. Strict bladder (empty) and rectal filling guidelines with daily CBCT verification mitigated uncertainties of internal CTV_P motion. The one patient with FIGO Stage IIIC2 SCC and para-aortic nodal (PAN) metastases had extended field VMAT to the level of the renal vessels. All target volumes and organ-at-risk (OAR) structures were curated according to American Association of Physicists in Medicine nomenclature Task Group 263 [35].
CRT was quality monitored within a collaborative Public–Private Hospital network. All mIGABT was performed within a single Public institution by the same care team.
Utero-vaginal mIGABT
Day-of-admission utero-vaginal applicator insertion was performed under GA. Specific COVID-19 GA procedures were protocoled to minimise nasopharyngeal aerosolisation, viral dissemination, and unnecessary contacts within the OR [19, 20, 25]. The operating table was pre-prepared with a single use Haines® Air-Assisted Transfer Mat (Haines Medical Australia, manufacturers of the Haines® Air-Assisted Transfer Mat) and reusable vacuum cushion (BlueBAG™; Elekta Solutions AB, Stockholm, Sweden) (Fig. 2A). Applicators were inserted under ultrasound guidance by the radiation oncologist (MJS). Cranio-caudal migration or rotation was prevented by meticulous vaginal (vas gauze) packing and vulvar suturing. Op-site® surgical body wrap secured the patient to the BlueBAG™ (Fig. 2B) which when evacuated formed a rigid cradle from breast-line to upper-thighs. Free draining in-dwelling urinary and rectal catheters were mandatory.
This set-up had been previously validated by us in over 150 LACC patients (> 600 IGABT fractions) since 2010. Significant applicator displacement or pelvic shift during multiple patient transfers was minimal [28]. Immobilisation was well tolerated overnight. Patient-controlled opioid analgesia was routine. A total of six transfer cycles from bed to MRI (pre-Fractions 1 and 2), and CT (pre-Fraction 3) couch top were required to complete mIGABT.
MRI/CT compatible applicators were of 2 types: Vienna Ring Set 26–34 mm (Elekta AB: Part No. 189.569) with fixed angle (60°) intrauterine 20-60 mm tandems (Tandem + Ring (T + R); 12/14 women: 86%), or Vaginal Applicator set (Elekta AB: Part No. 101001): 20-80 mm angled tandems (10–45°) and segmented (20-35 mm) cylinder set (Tandem + Cylinder (T + C); 2/14: 14%). No patient required a hybrid interstitial technique.
A dedicated brachytherapy planning system (Oncentra v4.6.0; Elekta AB) was used to contour, reconstruct, optimise, and evaluate dose target coverage. A standard loading pattern similar to a Manchester “Point A” plan was used as the starting point before manual conservative optimisation to ensure 3D-volume-based planning metrics were met. At least 90% of the ICRU 89 high-risk CTV (HRCTV) received 100% of the prescription dose (HRCTV_D90 concept) (Fig. 3). Pre-specified ICRU 89 OAR D2cc constraints (rectum, bladder, and sigmoid colon) were respected. OAR D0.1 cc and D1.0 cc exposures were also recorded. Emergent ICRU rectal, bladder, and vaginal late toxicity dose points, and vaginal reference length (VRL) were also identified [32, 36]. Vaginal toxicity points were located 0.5 cm deep to the mucosa in the anterior and lateral fornices, and for T + R patients (12/14), relative (± 2 cm) to the postero-inferior border of symphysis pubis (PIBS). The VRL was defined longitudinally from the PIBS point to the centre of the Vienna ring (vaginal sources).
MRI/MRI and MRI/CT image match
Fraction 1 HRCTV_D90 and OAR volumes were defined on the day of applicator insertion on T2-MRI sequences (Ingenia 3.0 T CX: Philips Medical Systems, Eindhoven, Netherlands), and imported into Velocity® (v4.1, Varian Medical Systems: Palo Alto, CA). Velocity® allowed rigid applicator registration and assessment of dosimetric uncertainties due to applicator displacement after Fraction 1. Oil-filled markers were placed within the applicators pre-imaging to aide localisation (Fig. 3). Relative inter-fractional applicator shift on Fraction 2 and Fraction 3 was primarily assessed by tandem tip/flange position (all cases), and ring (12/14) or cylinder dome (2/14) tilt, yaw, and migration. Secondary match structures included posterior bladder (empty) wall, rectal wall/tube, and symphysis pubis. Overall 3-D stability (± 1–2 mm) was confirmed using the Velocity® platform before Fractions 2 and 3. Based on internal departmental analysis and Schindel et al. [37], a tolerance of ≥ 3 mm was applied to the matching structures before brachytherapy re-plan was required.
mIGABT accelerated hyper-fractionation
Modified IGABT was delivered with HDR 192Ir (microSelectron® v3.1.4, Elekta AB). The EMBRACE/ICRU 89 IGABT protocol delivered a biologically-equivalent tumour dose (Linear-Quadratic [LQ] model: EQD2 α/β10Gy) of 39.7 Gy (4 IGABT fractions of 7 Gy in 2 insertions to the HRCTV_D90 over 8 days). We hypothesised a bio-effective mIGABT scheme to be 39.3 Gy (25.5 Gy in 3 fractions of 8.5 Gy in 1 day) as derived from the formula:
EQD2 mIGABT = Total modified dose (d x number fractions) x (α/β + d) (α/β + 2)−1 Gy, where d = modified dose (Gy)/fraction, and α/β for acute tumour effect = 10 Gy. EQD2 exposures for OAR late (injury) effects were derived at α/β = 3 Gy.[12].
Repair half-time within the LQ model was assumed to be 1.5 h. Our protocoled minimal overnight fractionation interval (Fx1 and Fx2: 17.9 ± 1.3 h), and day 2 gap (i.e. between Fx2 and Fx3: 5.3 ± 0.8 h), was probably sufficient to disregard any significant repair of sub-lethal injury.
The LQ EQD2 concept enabled direct summation of MRI-image-based dose-volume histogram mIGABT and CRT parameters (total HR-CTV_D90 coverage; EQD2 α/β10Gy). Similarly, total OAR exposures for probability of late toxicity (EQD2 α/β3Gy) were also calculated.
Toxicity
All acute and emergent (> 90 day) late toxicity data was collected by physician and patient-reported assessments according to the Common Terminology Criteria for Adverse Events (CTCAE) v4.03 [38]. Anatomically, five at-risk CTCAE system organ classes (SOC) were identified namely, 1. Blood and lymphatic system, 2. Gastrointestinal, 3. Renal and urinary, 4. Reproductive system, and 5. Musculoskeletal/connective tissue (insufficiency fractures). Specific SOC-related blood tests (full blood count and renal function) were administered during quarterly follow-up together with bi-manual pelvic examination, cervical liquid-based cytology and HPV “co-test” (Cobas® 4800, Branchburg NJ: Roche Molecular Systems, Inc; 2018). Re-staging FDG-PET imaging was done at 3 months, 12 months, and 24 months post UVBT. Diagnostic MRI, FDG-PET, and directed re-biopsies were repeated at any time if clinically indicated.
Cost analysis
In addition to reporting toxicity outcomes, a cost analysis was conducted to compare the cost of delivering mIGABT versus IGABT. This analysis was conducted with a health service perspective using a bottom-up approach. Labour costs were calculated based on NSW Health Awards [39,40,41,42] and the time that it took per task. In-hospital costs were based on departmental figures. All costs are reported in 2021 Australian dollars (AUD/0.72USD).
Statistical analysis
Descriptive and frequency statistics were used to delineate mean ± SD, and median with interquartile range (IQR) for non-normal data. Scatter plots depicted relationships between dose, volume, OAR point and linear vaginal parameters.
Results
Table 1 presents patient demographics for the 14 patients included in the study. Median age of our cohort was 62.5 years (37–82 years). Nine women (64%) had primary squamous cell cancer (SCC) and 5 (36%) had endocervical adenocarcinoma (AC). Four patients (29%) had lymph node metastases; pelvis only (Stage IIIC1; 3 cases), and 1 case (Stage IIIC2) with involvement of both pelvic and para-aortic nodal stations. The five AC cases were further classified as either Silva Pattern A (1/5) or unfavourable Pattern C (4/5) [43]. Mean follow-up was 20.3 ± 7.2 months. No patient had acquired COVID-19 infection when PCR tested on day of admission for mIGABT.
All patients completed both radiation components (EBRT and mIGABT). Mean EBRT PTV dose was 46.3 ± 2.7 Gy.
Patient 11 with favourable AC (Silva Pattern A) and minimal residual GTV_D (below) had mIGABT upfront as COVID-19 restrictions delayed her CRT. This patient also discontinued cisplatin (CDDP) chemotherapy after 3 cycles due to fatigue; 5 planned cycles of weekly CDDP were otherwise completed by the other 13 patients.
Total time to complete treatment (CRT + mIGABT) was exactly 38 days. Mean overall mIGABT treatment time was 22.8 ± 1.71 h.
Volumetric response
Mean cervix gross tumour volume-at-diagnosis (GTV_D) was 37.7 ± 71.6 cc. Excluding Patient 2 with very bulky central disease (266.2 cc), the mean GTV_D of our cohort was 20.2 ± 29.5 cc. Diagnostic loop excision of transformation zone was performed on both Stage IB1 patients (Patient 10 and Patient 11). This resulted in minimal residual disease before treatment (GTV_D: 0.2 cc and 2.1 cc respectively).
Respective median (IQR) HRCTV were Fraction 1: 18.6 cc (16.4–21.7), Fraction 2: 17.9 cc (16.0–21.8), and Fraction 3: 17.8 cc (14.4–22.2). Mean ± SD mIGABT HRCTV_D90 [EQD2: α/β10Gy] coverage was 37.5 ± 3.5 Gy. Combined total mean ± SD and median (IQR) HRCTV_D90 coverage was 87.5 ± 3.7 Gy and 89.4 Gy (87.2–89.6), respectively.
Complete MRI-defined cancer response before mIGABT (GTV_Fx1) was seen in 77% of cases (10/13). Measurable disease at fraction 2 was detected in 4 cases (GTV_Fx2): Patient 2 (21 cc), 4 (0.34 cc), 5 (4.4 cc), and 8 (1.3 cc). Minimal inter-fractional HRCTV adaption was required.
Velocity® matching
Dosimetric re-plans were necessary in only 3 patients (2/14: Fraction 2; and 1/14: Fraction 3). Contributors to this low frequency included geometric stability of patient-applicator setup, no or small residual GTV at time of mIGABT (13/14; 93%), and minimal perturbations in OAR volumes over 24 h. The Velocity® platform allowed rigid registration of pelvic simulator CT acquired in the brachytherapy facility and obviated the Fraction 3 MRI simulation and the associated in-patient bed transport to radiology.
Local control
All patients achieved complete clinical, metabolic (FDG-PET), and cervical “co-test” response at 3 months. High-risk human papilloma virus (hr-HPV) was cleared in every case either at this point (11/14: 79%) or at 6 months follow-up (3/14; 21%). Although Patient 1 and Patient 5 progressed systemically, no significant local symptoms were recorded (patient reported SOC: renal and urinary, and reproductive system), or was detected on re-imaging after salvage chemotherapy (Patient 1). This implied durable LACC control within the pelvis. Two-year actuarial PFS was 86% (12/14) and overall survival 93% (13/14).
Metastases
Systemic metastatic disease occurred in 2 cases (Patient 1 and Patient 5). Both had unfavourable Stage IIIB SCC with significant vaginal disease. Time-to-metastatic event was 10 and 12 months respectively. Patient 5 developed peritoneal metastases and died of sepsis at 12 months post-mIGABT without further cancer-directed care. Patient 1 was diagnosed with a solitary (biopsy-proven) lung metastasis on routine re-staging FDG-PET at 12 months. Salvage cisplatin/paclitaxel doublet chemotherapy with bevacizumab [44] resulted in complete metabolic (FDG) response which is maintained at 24 months.
Cost analysis
In this context, the cost of delivering IGABT (28 Gy/4 fractions) is 6,024.98 AUD and 3,756.49 AUD to deliver mIGABT (25.5 Gy/3 fractions). Adopting our mIGABT approach resulted in Public Health cost savings of 2,268.49 AUD (1,633.31 USD) per treated patient (Table 2). To date, we have treated 14 patients with our mIGABT protocol and it has saved our institution 31,758.84 AUD (22,866.38 USD). In a large public teaching hospital such as ours, we treat approximately 15 cases of cervix cancer a year. If mIGABT is delivered standardly to this patient cohort then the total projected amount saved per year will be 34,027.35 AUD (24,949.65 USD).
Toxicity
Both components of care (CRT + mIGABT) were well tolerated. Acute cysto-proctitis during CRT was usually minor (≤ G2) and self-limiting in 13/14 (93%). Excluding Patient 2 (extended-field; pelvis + PAN), median pelvis-only PTV V43Gy was 1360 cc (1322–1418.5 cc).
Severe (≥ G3) acute toxicity was documented in Patient 2 only. As previously stated, this case had massive GTV_D (266.2 cc) and was also the only patient who required extended-field VMAT due to gross para-aortic lymph node metastases (Stage IIIC2). Final PTV V43Gy (2407.3 cc) and V55Gy (1117.5 cc) were both significant [7]. Haemorrhagic proctitis was associated with therapeutic anti-coagulation for significant pelvic venous thrombosis and pulmonary embolism at diagnosis. Rectal bleeding settled with transition to fractionated heparin and glucocorticoid suppositories. Patient 2 was also the only case who developed severe late toxicities across all 5 SOC groups, viz., 1. Blood and lymphatic system: anaemia requiring transfusion, 2. Gastro-intestinal tract: recurrent/persistent low volume haematochezia and diarrhoea, 3. Renal and urinary system: haematuria/bilateral ureteric stenosis (unilateral stent), 4. Reproductive: significant vaginal stenosis/vaginismus and dyspareunia, and 5. Musculo-skeletal system: asymptomatic pelvic (sacro-iliac) insufficiency fracture was noted on routine FDG-PET at 12 months. Pelvic examination, cervical co-test, and re-staging FDG-PET at 24 months, however confirmed healed fracture and cervix cancer-free status. Unfortunately, a wide vesico-vaginal fistula developed at 26 months following a stretch vaginoplasty and necessitated an anterior exenteration (G4 late toxicity). No histologic evidence of residual cervix cancer was present within resected tissue.
OAR exposures at completion of treatment were well within ICRU 89 guidelines. Respective total median D2cc. [EQD2α/β3Gy] for bladder, rectum, and sigmoid colon was 65.9 Gy (58.4–72.5), 59.1 Gy (55.7–61.8), and 54.6 Gy (50.3–58.9). Median dose at ICRU dose points for bladder 62.9 Gy (52.3–79.6) and recto-vaginal (RV) septum was 66.2 Gy (53.6–80.7). By comparison, absolute ICRU RV dose in Patient 1 and Patient 2 was 87.8 Gy and 75.7 Gy respectively, after T + C brachytherapy. Table 3 depicts combined HRCTV metrics for individual patients with ICRU Point-A doses for comparison. Most V200 (mean 27 ± 9 cc.) was restricted to the applicator system even in Patient 1 (23 cc.) and Patient 2 (16.5 cc.). Mean (SD) TRAK (total reference air-kerma rate at 1 m) was also acceptable/low at 0.0034 Gy (0.0016) and well within the 0.02 Gy associated with significant late bowel morbidity by Bockel et al. [45].
In LACC the vagina is both an OAR and potential target volume. Vaginal ICRU points reflected brachytherapy dose gradients at the level of vaginal sources 5 mm deep to the surface of the vaginal ring (12/14 cases) or cylinder dome (2/14; T + C cases). The exposures are representative at the mid-circumference within the 4 quadrants of the vaginal fornix. The T + C set did not allow differential (anisotropic) dosing and were excluded. Respective IGABT median (IQR) right, left, anterior, and posterior vaginal point exposures (12/14; T + R patients) were: 6.2 Gy (5.6–6.9), 5.8 Gy (4.9–7.1), 4.1 Gy (3.4–4.9), and 5.0 Gy (3.6–6.4). Total absolute doses were 52.5 Gy, 52.1 Gy, 50.4 Gy, and 51.3 Gy, respectively.
Table 4 displays combined dose OAR D2cc exposures for bladder, and rectum versus mIGABT bladder, recto-vaginal (RV), and vaginal ICRU dose point measurements. Figure 4 relates the vaginal OAR data to median total doses administered at PIBS points (PIBS ‘0’ ± 2 cm) versus VRL. By definition VRL could only be derived in the 12 women with T + R applicators; mean ± SD and median (IQR) VRL was 55.4 mm ± 10.7, and 55.2 mm (48.3–60.0) respectively. Predictive modelling for emergent late radiation toxicity is suggested in the Discussion.
Discussion
Over a 15-year period a landmark series of Gynaecological (GYN) GEC-ESTRO Working Group Recommendations (I–IV) described a coherent methodology of utero-vaginal MRI-IGABT prescription, recording, and reporting in LACC [11,12,13,14]. These publications (2005–2012) introduced the concepts of GTV and high-risk clinical target volume (HRCTV), and OARs in the familiar epistemology of 3D-EBRT. Similar to EBRT, brachytherapy dose became tractable as bio-equivalent daily fractions of 2-Gray based on differential tissue repair kinetics (Linear Quadratic EQD2Gy model) [12]. Personalised target and OAR dose-volume parameters had replaced the historical anatomic and prescription reference points of the traditional 2D-cervix brachytherapy traditions (or “Schools”).
Based on these principles, and through prior IGABT clinical practice [46, 47], the GYN GEC-ESTRO international EMBRACE-I study (2008–2015; 1416 patients) produced “unprecedented” actuarial 5-year rates of cervix cancer control (92%; 1233/1341 analysed). Rates of serious (≥ G3) OAR late toxicity were low (cumulative 14.6%; 3–6% per organ system). Remarkably, compared with mono-institutional IGABT cohorts [44, 47], the 5-year overall survival improved even in advanced Stage IIIB/IVA patients (74% to 79%). Historical 5-year disease-specific survival rates of only 35% [48] were expected in Stage IIIB women often due to suboptimal local and regional nodal control. Sustained eradication of central pelvic and nodal metastatic disease in EMBRACE-I however, were both excellent (87%) at 5-years. The significant predictive impact of pelvic and nodal control on overall survival in patients with LACC were confirmed in a recent nomogram from the GYN GEC-ESTRO group [47].
EMBRACE-I established the combined (EBRT/IGABT) minimal HRCTV_D90 target dose of 85 Gy [EQD2: α/β10Gy] as a hard goal for controlling the central pelvis. A range of safe OAR D2cc exposures (EQD2: α/β3Gy) were also reported. These have since been refined as primary planning aims in the current EMBRACE-II study [15]. Specifically, bladder D2cc (< 80 Gy), rectum D2cc (< 65 Gy), and sigmoid/bowel D2cc (< 70 Gy) were recommended constraints in addition to maximal ICRU recto-vaginal (RV) dose point exposure of less than 65 Gy. The latter correlates with vaginal shortening and stenosis [32, 36]. The principles and parameters of EMBRACE-I were validated by ICRU Report 89 [27]. ICRU 89 (2016) remains an enduring global capstone in the healthcare of women with LACC.
Despite these gains, optimal treatment of LACC is technically complex and health resource consumptive. In LMICs with the highest prevalence of cervix cancer, sophisticated oncologic care is simply unavailable or difficult to access [2, 4, 6]. Furthermore, over 90% of MRI scanners exist in high-income-countries. Democratising LACC treatment would require major LACC treatment re-design at several levels beginning perhaps with point-of-care enhanced low static field (LF) MRI units [49]. LF-MRI (0.25–1.0T) does not require expensive cryogenics, and has modest energy consumption, installation, and maintenance costs. Compact open-system LF-MRI configurations are ideal for MRI “fluoroscopy” and real-time (metal) applicator tracking for volume-based IGABT in remote areas. With appropriate industry and academic partnerships, a sustainable locally managed single insertion IGABT programme could be feasibly implemented in some LMIC settings [2, 4, 6].
Although major healthcare disparities are rare in Australia [50], the 2020 COVID-19 pandemic introduced uncertainties in patient care and sudden access delay to Public Health infrastructure. This challenged us to modify our original Vienna 4-fraction EMBRACE protocol [26, 29]. Re-design to an iso-effective single insertion IGABT protocol immediately halved our operating room requirements and in-patient transfers for MRI scans. The economic cost of our mIGABT schedule was shown with net savings of 2,268.49AUD (1,634USD) per treated patient (Table 2). There were no acute (≤ 3 months) re-hospitalisations.
This non-inferiority study of 14 women with LACC demonstrated the real-world “fungibility” of the radio-biological backbone of EMBRACE-I. Our IGABT fraction sizes of 8.5 Gy via a single utero-vaginal insertion delivered a mean (SD) combined HRCTV_D90 of 87.5 ± 3.7 Gy (EQD2Gy) in 3 fractions accelerated over 24 h. This schedule with pre-emptive or sequential CRT was generally well tolerated. All indices of HRCTV_D90 coverage, OAR, and most individual organ system ICRU dose point exposures were within published efficacy and chronic safety recommendations. Overall treatment time was significantly less than 50 days (38 days). Actuarial overall metabolic (FDG-PET) progression-free survival was 93%. All patients achieved central pelvis control with early eradication of malignant cytology (3-months) and hr-HPV (by 6-months) on PCR co-testing. Lymph node failure or persistent nodal metastatic disease did not occur. Our EBRT induction platform of dynamic VMAT and simultaneous accelerated integrated boost (55-60 Gy) to GTV_N with full chemotherapy intensity in 93% of patients (13/14) is assumed to have contributed to this success [7, 8, 32]. Registration of the pre-treatment MRI/FDG-PET to the pelvic CT-simulation series aided localisation of GTV_N. Rules for CTV_P and CTV_N contouring and OAR delineation were consistently applied since first adopting EMBRACE-I standards in 2010.
Our experience paralleled that of Mahantshetty et al. [33]. Their Phase I/II SIMBRACE trial utilised a single insertion 3-fraction MRI-IGABT regimen with HRCTV_D90 coverage of 9 Gy (Day 1) and 2 fractions of 7 Gy separated by 6-h on Day 2. Inter-fractional CT imaging determined the requirement for dosimetric re-plan. SIMBRACE had mean overall treatment time 9 days longer at 47 ± 6 days and their EBRT platform doses was higher (50 Gy) ± weekly CDDP chemotherapy. Two-year pelvic control was 90.1% in FIGO IIB-IVA patients with a comparable low rate (5.3%) of G3 rectal toxicity in the 38 women treated on protocol.
Although a post-COVID-19 change in our pattern of brachytherapy practice awaits longer follow-up, limitation to our method was suggested by significant late toxicity signals in one patient (Patient 2) with advanced central pelvic cancer (GTV_D: 266.2 cc). Extensive residual upper and middle third vaginal disease after CRT (HRCTV: 68 cc.) required a less optimal T + C IGABT technique which did not permit differential loading at the cervix level. The final combined ICRU RV point dose was almost 137% higher than the cohort median (75.7 Gy vs. 55.3 Gy) despite a low cancer residuum within the cervix (24 cc). ICRU Point A dosing was also highest (Table 3): 83.4 Gy (remainder cohort mean: 61.8 ± 5.3 Gy) although TRAK was relatively low (0.008 Gy). TRAK (≥ 0.02 Gy), residual HRCTV (> 25 cc.), and prior “active smoking” have been identified as risk factors for emergent bowel toxicity in a large multivariate analysis by Bockel et al. [45]. Although a prior tobacco smoker (10–20 pack-years), her EBRT was well within EMBRACE dose-volume D95 guidelines for extended-field radiation therapy (< 3500 cc): PTV V43Gy (2407.3 cc). Neo-adjuvant cyto-reductive chemotherapy [44] and hybrid (intracavity/interstitial) IGABT [46] were considered but the malignancy-associated coagulopathy with heavy vaginal bleeding, extensive deep venous pelvic thromboses, and significant pulmonary embolism were unique factors complicating this patient’s presentation.
Conclusions
This small study has demonstrated the utility of single insertion 3-fractional utero-vaginal MRI- IGABT and CRT in a cohort of 14 women with LACC. Loco-regional control was achieved in all cases. Single insertion IGABT was logistically efficient, overall cost-saving, and patient-centric during the COVID-19 pandemic. Severe pelvic toxicity in one patient (Patient 2) who is cancer-free at 30-months post-anterior exenteration, implicated both large residual HRCTV, history of cigarette smoking, and mIGABT applicator type to risk of organ-system injury.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- 3 T:
-
3 Tesla
- AAPM:
-
American Association of Physicists in Medicine
- BT:
-
Brachytherapy
- CBCT:
-
Cone beam computer tomography
- CCR:
-
Combined composite response
- CDDP:
-
Cisplatin
- COVID-19:
-
Coronavirus disease 2019
- CRT:
-
Chemo–radiation therapy
- CTCAE:
-
Common Terminology Criteria for Adverse Events
- CT:
-
Computer tomography
- CTV:
-
Clinical target volume
- CTV_N:
-
Clinical target volume nodal
- CTV_P:
-
Clinical target volume primary
- EBRT:
-
External beam radiation therapy
- EMBRACE:
-
Image guided intensity modulated External beam radiotherapy and MRI based adaptive BRAchytherapy in locally advanced CErvical cancer
- EQD2:
-
Equivalent total doses in 2 Gy fractions
- EUA:
-
Examined under anaesthesia
- FDG:
-
Fluorodeoxyglucose
- FIGO:
-
International Federation of Gynecology and Obstetrics
- GA:
-
General anaesthetic
- GTV:
-
Gross tumour volume
- GTV_D:
-
Gross tumour volume-at-diagnosis
- GTV_N:
-
Gross tumour volume nodal
- GYN GEC-ESTRO:
-
Gynaecological Groupe Européen de Curiethérapie -European Society for Radiotherapy and Oncology
- HDRB:
-
High dose-rate brachytherapy
- HIC:
-
High income countries
- hr-HPV:
-
High risk human papillomavirus
- IARC:
-
International Agency for Research on Cancer
- ICRU:
-
International Commission on Radiation Units and Measurements
- IGABT:
-
MRI-guided adaptive utero-vaginal brachytherapy
- LACC:
-
Locally advanced cervix cancer
- LMIC:
-
Low and middle income countries
- LQ:
-
Linear quadratic
- mIGABT:
-
Modified MRI-guided adaptive brachytherapy
- MRI:
-
Magnetic resonance imaging
- OAR:
-
Organ-at-risk
- OR:
-
Operating room
- PAN:
-
Para-aortic nodal
- PCR:
-
Polymerase chain reaction
- PET:
-
Positron emission tomography
- PFS:
-
Progression free survival
- PIBS:
-
Postero-inferior border of the symphysis pubis
- PTV:
-
Planning target volume
- PTV_N:
-
Planning target volume lymph node
- PTV_P:
-
Pelvic planning target volume
- RV:
-
Recto-vaginal
- SD:
-
Standard deviation
- SOC:
-
System organ classes
- T + C:
-
Tandem + Cylinder
- T + R:
-
Tandem + Ring
- UVBT:
-
Utero-vaginal brachytherapy
- VMAT:
-
Volumetric modulated arc therapy
- VRL:
-
Vaginal reference length
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
Grover S, Longo J, Einck J, Puri P, Brown D, Chino J, Mahantshetty U, Yashar C, Erickson B. The unique issues with brachytherapy in low-and middle-income countries. Semin Radiat Oncol. 2017;27(2):136–42.
Spencer JC, Brewer NT, Coyne-Beasley T, Trogdon JG, Weinberger M, Wheeler SB. Reducing poverty-related disparities in cervical cancer: the role of HPV vaccination poverty-related cervical cancer disparities. Cancer Epidemiol Biomark Prev. 2021;30(10):1895–903.
Abdel-Wahab M, Grover S, Zubizarreta EH, Rubio JAP. Addressing the burden of cervical cancer through IAEA global brachytherapy initiatives. Brachytherapy. 2020;19(6):850–6.
World Health Organization. WHO framework for strengthening and scaling-up of services for the management of invasive cervical cancer 2020.
International Atomic Energy Agency. Modern techniques in brachytherapy for cancer with special reference to the developing countries. IAEA; 2022.
Berger T, Seppenwoolde Y, Pötter R, Assenholt MS, Lindegaard JC, Nout RA, de Leeuw A, Jürgenliemk-Schulz I, Tan LT, Georg D. Importance of technique, target selection, contouring, dose prescription, and dose-planning in external beam radiation therapy for cervical cancer: evolution of practice from EMBRACE-I to II. Int J Radiat Oncol* Biol* Phys. 2019;104(4):885–94.
Chino J, Annunziata CM, Beriwal S, Bradfield L, Erickson BA, Fields EC, Fitch K, Harkenrider MM, Holschneider CH, Kamrava M. Radiation therapy for cervical cancer: executive summary of an ASTRO clinical practice guideline. Pract Radiat Oncol. 2020;10(4):220–34.
Cannon J, Bownes P, Mason J, Cooper R. UK audit of target volume and organ at risk delineation and dose optimisation for cervix radiotherapy treatments. Br J Radiol. 2020;93(1110):20190897.
Holschneider CH, Petereit DG, Chu C, Hsu I-C, Ioffe YJ, Klopp AH, Pothuri B, Chen L-M, Yashar C. Brachytherapy: a critical component of primary radiation therapy for cervical cancer: from the Society of Gynecologic Oncology (SGO) and the American Brachytherapy Society (ABS). Brachytherapy. 2019;18(2):123–32.
Haie-Meder C, Pötter R, Van Limbergen E, Briot E, De Brabandere M, Dimopoulos J, Dumas I, Hellebust TP, Kirisits C, Lang S. Recommendations from gynaecological (GYN) GEC-ESTRO Working Group☆(I): concepts and terms in 3D image based 3D treatment planning in cervix cancer brachytherapy with emphasis on MRI assessment of GTV and CTV. Radiother Oncol. 2005;74(3):235–45.
Pötter R, Haie-Meder C, Van Limbergen E, Barillot I, De Brabandere M, Dimopoulos J, Dumas I, Erickson B, Lang S, Nulens A. Recommendations from gynaecological (GYN) GEC ESTRO working group (II): concepts and terms in 3D image-based treatment planning in cervix cancer brachytherapy—3D dose volume parameters and aspects of 3D image-based anatomy, radiation physics, radiobiology. Radiother Oncol. 2006;78(1):67–77.
Hellebust TP, Kirisits C, Berger D, Pérez-Calatayud J, De Brabandere M, De Leeuw A, Dumas I, Hudej R, Lowe G, Wills R. Recommendations from gynaecological (GYN) GEC-ESTRO Working Group: considerations and pitfalls in commissioning and applicator reconstruction in 3D image-based treatment planning of cervix cancer brachytherapy. Radiother Oncol. 2010;96(2):153–60.
Dimopoulos JC, Petrow P, Tanderup K, Petric P, Berger D, Kirisits C, Pedersen EM, Van Limbergen E, Haie-Meder C, Pötter R. Recommendations from gynaecological (GYN) GEC-ESTRO working group (IV): Basic principles and parameters for MR imaging within the frame of image based adaptive cervix cancer brachytherapy. Radiother Oncol. 2012;103(1):113–22.
Pötter R, Tanderup K, Kirisits C, de Leeuw A, Kirchheiner K, Nout R, Tan LT, Haie-Meder C, Mahantshetty U, Segedin B. The EMBRACE II study: the outcome and prospect of two decades of evolution within the GEC-ESTRO GYN working group and the EMBRACE studies. Clin Transl Radiat Oncol. 2018;9:48–60.
Hanna T, Shafiq J, Delaney G, Barton M. The population benefit of radiotherapy for cervical cancer: local control and survival estimates for optimally utilized radiotherapy and chemoradiation. Radiother Oncol. 2015;114(3):389–94.
World Health organization. Technical specifications of radiotherapy equipment for cancer treatment. Geneva: WHO. 2021. Available from: https://www.who.int/publications/i/item/9789240019980.
Schad MD, Patel AK, Glaser SM, Balasubramani GK, Showalter TN, Beriwal S, Vargo JA. Declining brachytherapy utilization for cervical cancer patients-have we reversed the trend? Gynecol Oncol. 2020;156(3):583–90.
Weinkove R, McQuilten ZK, Adler J, Agar MR, Blyth E, Cheng AC, Conyers R, Haeusler GM, Hardie C, Jackson C. Managing haematology and oncology patients during the COVID-19 pandemic: interim consensus guidance. Med J Aust. 2020;212(10):481–9.
Prakash L, Dhar SA, Mushtaq M. COVID-19 in the operating room: a review of evolving safety protocols. Patient Saf Surg. 2020;14(1):1–8.
Kumar D, Dey T. Recapitulating intracavitary brachytherapy in cervical cancer patients during the COVID-19 pandemic: a viewpoint. Future Oncol. 2020;16(28):2143–6.
Agency for Clinical Innovation. Key principles for management of surgery during COVID-19 pandemic: advice for NSW health services. 2020. Available from: https://www.health.nsw.gov.au/Performance/Documents/covid-surgery-principles.pdf.
Williams VM, Kahn JM, Harkenrider MM, Chino J, Chen J, Fang LC, Dunn EF, Fields E, Mayadev JS, Rengan R. COVID-19 impact on timing of brachytherapy treatment and strategies for risk mitigation. Brachytherapy. 2020;19(4):401–11.
Mohindra P, Beriwal S, Kamrava M. Proposed brachytherapy recommendations (practical implementation, indications, and dose fractionation) during COVID-19 pandemic. Brachytherapy. 2020;19(4):390–400.
Miriyala R, Mahantshetty U. Brachytherapy in cervical cancer radiotherapy during COVID-19 pandemic crisis: problems and prospects. J Contemp Brachyther. 2020;12(3):290–3.
Pötter R, Tanderup K, Schmid MP, Jürgenliemk-Schulz I, Haie-Meder C, Fokdal LU, Sturdza AE, Hoskin P, Mahantshetty U, Segedin B. MRI-guided adaptive brachytherapy in locally advanced cervical cancer (EMBRACE-I): a multicentre prospective cohort study. Lancet Oncol. 2021;22(4):538–47.
International Commission on Radiation Units and Measurements. ICRU 89: prescribing, recording, and reporting brachytherapy for cancer of the cervix. J ICRU. 2013;13(1–2):1–258.
Stevens MJ, Martland J. 3T MR image-guided cervix brachytherapy with novel immobilization-initial experience. Brachytherapy. 2014;13:S64.
Potter R, Georg P, Dimopoulos JCA, Grimm M, Berger D, Nesvacil N, Georg D, Schmid MP, Reinthaller A, Sturdza A, Kirisitis C. Clinical outcome of protocol-based image (MRI) guided adaptive brachytherapy combined with 3D conformal radiotherapy with or without chemotherapy in patients with locally advanced cervical cancer. Radiother Oncol. 2011;100:116–23.
Albuquerque K, Hrycushko BA, Harkenrider MM, Mayadev J, Klopp A, Beriwal S, Petereit DG, Scanderbeg DJ, Yashar C. Compendium of fractionation choices for gynecologic HDR brachytherapy—an American Brachytherapy Society Task Group Report. Brachytherapy. 2019;18(4):429–36.
Goswami J, Manir KS, Mondal M, Mallik S, Das S, Sen A, Pal B, Das S, Palit S, Sarkar P. Clinical audit of dose-escalated radical radiotherapy for advanced cervical carcinoma using a pragmatic protocol (3 fractions of 8 Gy HDR brachytherapy). Gynecol Oncol Rep. 2021;37: 100822.
Sturdza AE, Knoth J. Image-guided brachytherapy in cervical cancer including fractionation. Int J Gynecol Cancer. 2022;32(3).
Mahantshetty U, Gurram L, Bushra S, Ghadi Y, Aravindakshan D, Paul J, Hande V, Pilar A, Chopra S, Ghosh J. Single application multifractionated image guided adaptive high-dose-rate brachytherapy for cervical cancer: dosimetric and clinical outcomes. Int J Radiat Oncol* Biol* Phys. 2021;111(3):826–34.
Bhatla N, Berek JS, Cuello Fredes M, Denny LA, Seija G, Karunaratne K, Kehoe ST, Konishi I, Olawaiye AB, Prat J, Sankaranarayanan R, Brierley J, Mutch D, Querleu D, Cibula D, Quinn M, Botha H, Sigurd L, Rice L, Ryu H-S, Ngan H, Mäenpää J, Andrijono A, Purwoto G, Maheshwari A, Bafna UD, Plante M, Natarajan J. Revised FIGO staging for carcinoma of the cervix uteri. Int J Gynaecol Obstet. 2019;145(1):129–35.
Mayo CS, Moran JM, Bosch W, Xiao Y, McNutt T, Popple R, Michalski J, Feng M, Marks LB, Fuller CD. American Association of Physicists in Medicine Task Group 263: standardizing nomenclatures in radiation oncology. Int J Radiat Oncol Biol Phys. 2018;100(4):1057–66.
Kirchheiner K, Nout RA, Lindegaard JC, Haie-Meder C, Mahantshetty U, Segedin B, Jürgenliemk-Schulz IM, Hoskin PJ, Rai B, Dörr W. Dose–effect relationship and risk factors for vaginal stenosis after definitive radio (chemo) therapy with image-guided brachytherapy for locally advanced cervical cancer in the EMBRACE study. Radiother Oncol. 2016;118(1):160–6.
Schindel J, Zhang W, Bhatia SK, Sun W, Kim Y. Dosimetric impacts of applicator displacements and applicator reconstruction-uncertainties on 3D image-guided brachytherapy for cervical cancer. J Contemp Brachyther. 2013;5(4):250–7.
US Department of Health and Human Services. Common Terminology criteria for adverse events (CTCAE). Version 5.0 2017. Available from: https://ctep.cancer.gov/protocoldevelopment/electronic_applications/docs/ctcae_v5_quick_reference_8.5x11.pdf.
NSW Health. Health Employees Medical Radiation Scientists (State) Award 2021: NSW Health; 2021. Available from: https://www.health.nsw.gov.au/careers/conditions/Awards/hsu-he-medical-radiation-scientist.pdf.
NSW Health. Health professional and mecical salaries (State) Award 2021: NSW Health; 2021. Available from: https://www.health.nsw.gov.au/careers/conditions/Awards/he-profmed-salaries.pdf.
NSW Health. Public Health System Nurses and Midwives (State) Award 2021: NSW Health; 2021. Available from: https://www.nswnma.asn.au/wp-content/uploads/2021/08/Public-Health-System-Nurses-and-Midwives-State-Award-2021.pdf.
NSW Health. Staff Specialists (State) Award 2021: NSW Health; 2021. Available from: https://www.health.nsw.gov.au/careers/conditions/Awards/staff-specialists-award.pdf.
Alvarado-Cabrero I, Parra-Herran C, Stolnicu S, Roma A, Oliva E, Malpica A. The Silva pattern-based classification for HPV-associated invasive endocervical adenocarcinoma and the distinction between in situ and invasive adenocarcinoma: relevant issues and recommendations from the International Society of Gynecological Pathologists. Int J Gynecol Pathol. 2021;40(2 Suppl 1):S48.
Tewari KS, Sill MW, Penson RT, Huang H, Ramondetta LM, Landrum LM, Oaknin A, Reid TJ, Leitao MM, Michael HE. Bevacizumab for advanced cervical cancer: final overall survival and adverse event analysis of a randomised, controlled, open-label, phase 3 trial (Gynecologic Oncology Group 240). Lancet. 2017;390(10103):1654–63.
Bockel S, Escande A, Dumas I, Manea E, Morice P, Gouy S, Deutch E, Haie-Meder C, Chargari C. Total reference air kerma is associated with late bowel morbidity in locally advanced cervical cancer patients treated with image-guided adaptive brachytherapy. J Clin Med. 2020;8:125–36.
Sturdza A, Pötter R, Fokdal LU, Haie-Meder C, Tan LT, Mazeron R, Petric P, Šegedin B, Jurgenliemk-Schulz IM, Nomden C. Image guided brachytherapy in locally advanced cervical cancer: Improved pelvic control and survival in RetroEMBRACE, a multicenter cohort study. Radiother Oncol. 2016;120(3):428–33.
Sturdza AE, Pötter R, Kossmeier M, Kirchheiner K, Mahantshetty U, Haie-Meder C, Lindegaard JC, Jurgenliemk-Schulz I, Tan LT, Hoskin P. Nomogram predicting overall survival in patients with locally advanced cervical cancer treated with radiochemotherapy including image-guided brachytherapy: a retro-EMBRACE study. Int J Radiat Oncol Biol Phys. 2021;111(1):168–77.
Montana GS, Fowler WC, Varia MA, Walton LA, Mack Y, Shemanski L. Carcinoma of the cervix, stage III. Results Radiat Ther Cancer. 1986;57(1):148–54.
Hori M, Hagiwara A, Goto M, Wada A, Aoki S. Low-field magnetic resonance imaging: its history and renaissance. Invest Radiol. 2021;56(11):669.
Anderson K, Diaz A, Parikh DR, Garvey G. Accessibility of cancer treatment services for Indigenous Australians in the Northern Territory: perspectives of patients and care providers. BMC Health Serv Res. 2021;21(1):1–13.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
MJS, FK, RB, JM study conceptualization. MJS, FK, JY, LB, JA data curation. MS, RB, FK, JM, JA, JY formal analysis. MJS, FK, LB investigations. MJS, FK, JM, RB study methodology. Original draft of manuscript MJS. Review and editing of manuscript MJS, FK, JM, RB, LB, JA, JY. All authors read and approved the final manscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was pre-approved by the Northern Sydney Local Health District (NSLHD) and included patients who had consented to the use of their oncologic and general medical data stored by the Northern Sydney Cancer Centre for clinical follow-up and research purposes. HREC reference: 2021/ETH01361.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Stevens, M.J., Ko, F., Martland, J. et al. Safety and efficacy of single insertion accelerated MR-image guided brachytherapy following chemo–radiation in locally advanced cervix cancer: modifying our EMBRACE during the COVID pandemic. Radiat Oncol 18, 54 (2023). https://doi.org/10.1186/s13014-023-02240-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13014-023-02240-5