Abstract
Background
Because myocardial infarction in young adults is rare, there has been limited research on the condition in this patient group. Very few data are available regarding the long-term outcomes of patients under 40 years of age with non-ST-segment elevation myocardial infarction (NSTEMI) undergoing invasive treatments. The prognostic value of uric acid (UA) in young patients with NSTEMI who undergo percutaneous coronary intervention (PCI) has also not been studied. The purpose of this study was to evaluate the long-term clinical outcomes of this specific subset of young patients. In addition, we aimed to identify the role of serum UA in predicting the long-term prognosis of young patients with NSTEMI who have undergone PCI.
Methods
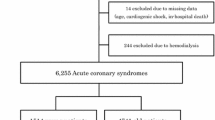
We performed a retrospective analysis of 213 young adult patients (≤40 years old) with NSTEMI who underwent PCI during their hospitalization at our tertiary referral center.
Results
The mean age of the 213 patients was 36.8 ± 3.3 years (range, 21–40 years). The median follow-up was 930 days. Our patients were predominantly male (88.3%) and the most frequent traditional cardiovascular risk factors were smoking and dyslipidemia. Baseline TIMI flow 0–1, estimated glomerular filtration rate (eGFR), and UA were found to be independently correlated with long-term major adverse cardiovascular events (MACEs) in multivariate Cox regression analysis.
Conclusion
In the present study, baseline TIMI flow 0–1, admission eGFR, and UA levels were correlated with MACEs during long-term follow-up in young patients with NSTEMI.
Zusammenfassung
Hintergrund
Da ein Herzinfarkt bei jungen Erwachsenen selten ist, gibt es Untersuchungen dazu in dieser Patientengruppe nur in begrenztem Umfang. Zu den Langzeitergebnissen von Patienten unter 40 Jahren mit Nicht-ST-Strecken-Hebungs-Infarkt (NSTEMI), bei denen eine invasive Therapie durchgeführt wurde, gibt es nur sehr wenige Daten. Der prognostische Wert der Harnsäurewerte bei jungen Patienten mit NSTEMI, bei denen eine perkutane Koronarintervention (PCI) erfolgt, ist bisher ebenfalls nicht untersucht worden. Ziel der vorliegenden Studie war es, die klinischen Langzeitergebnisse dieser speziellen Untergruppe junger Patienten zu untersuchen. Darüber hinaus war es Ziel der Autoren, die Bedeutung der Harnsäure im Serum für die Vorhersage der Langzeitprognose junger Patienten mit NSTEMI zu ermitteln, bei denen eine PCI durchgeführt wurde.
Methoden
Retrospektiv wurden die Daten von 213 jungen erwachsenen Patienten (≤40 Jahre) mit NSTEMI ausgewertet, bei denen während ihres stationären Aufenthalts in dem Tertiärversorgungszentrum der Autoren eine PCI erfolgte.
Ergebnisse
Das durchschnittliche Alter der 213 Patienten betrug 36,8 ± 3,3 Jahre (Spanne: 21–40 Jahre). Im Mittel dauerte die Nachbeobachtungsphase 930 Tage. Die hier untersuchten Patienten waren in der Mehrzahl Männer (88,3 %), und die häufigsten üblichen kardiovaskulären Risikofaktoren waren Rauchen und Fettstoffwechselstörungen. Ein TIMI-Fluss (Thrombolysis-in-myocardial-Infarction-Klassifikation) zu Studienbeginn von 0–1, die geschätzte glomeruläre Filtrationsrate (eGFR) und die Harnsäurewerte stellten sich in der multivariaten Cox-Regressionsanalyse auf lange Sicht als unabhängig mit schweren ungünstigen kardiovaskulären Ereignissen (MACE) korreliert heraus.
Schlussfolgerung
Ein TIMI-Fluss von 0–1, die eGFR bei stationärer Aufnahme und die Harnsäurewerte waren in der vorliegenden Studie mit MACE während der Langzeitnachbeobachtung bei jungen Patienten mit NSTEMI korreliert.


Similar content being viewed by others
References
Zimmerman FH, Cameron A, Fisher LD, Ng G (1995) Myocardial infarction in young adults: angiographic characterization, risk factors and prognosis (Coronary Artery Surgery Study Registry). J Am Coll Cardiol 26:654–661
Schoenenberger AW, Radovanovic D, Stauffer JC et al (2011) Acute coronary syndromes in young patients: Presentation, treatment and outcome. International Journal of Cardiology 148:300–304
Canga Y, Osmonov D, Karataş MB et al (2011) Cannabis: a rare trigger of premature myocardial infarction. Anadolu Kardiyol Dergisi 11:271–275
Qureshi AI, Suri MF, Guterman LR, Hopkins LN (2001) Cocaine use and the likelihood of nonfatal myocardial infarction and stroke: data from the third national health and nutrition examination survey. Circulation 103:502–506
Trkulja V, Car S (2012) On-admission serum uric acid predicts outcomes after acute myocardial infarction: systematic review and meta-analysis of prognostic studies. Croat Med J 53(2):162–172
Zand S, Shafiee A, Boroumand M, Jalali A, Nozari Y (2013) Serum uric acid is not an independent risk factor for premature coronary artery disease. Cardiorenal Med 3(4):246–253
Roffi M, Patrono C, Collet JP et al (2015) ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Rev Esp Cardiol (engl Ed) 68(2015):1125
Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150(9):604–612
Sianos G, Papafaklis MI, Serruys PW (2010) Angiographic thrombus burden classification in patients with ST-segment elevation myocardial infarction treated with percutaneous coronary intervention. J Invasive Cardiol 22(10 suppl B):6B–14B
Kirma C, Izgi A, Dundar C, Tanalp AC, Oduncu V, Aung SM et al (2008) Clinical and prodedural predictors of no-reflow phenomenon after primary percutaneous coronary interventions: experience at a single center. Circ J 72:716–721
Cheitlin MD, Armstrong WF, Aurigemma GP et al (2003) ACC/AHA/ASE 2003 guideline update for the clinical application of echocardiography-summary article: a report of the American college of cardiology/American heart association task force on practice guidelines (ACC/AHA/ASE committee to update the 1997 guidelines for the clinical application of echocardiography). J Am Coll Cardiol 42(5):954–970
de Soeiro AM, Fernandes FL, Soeiro MC et al (2015) Clinical characteristics and long-term progression of young patients with acute coronary syndrome in Brazil. Einstein (São Paulo) 13(3):370–375
Matsis K, Holley A, Al-Sinan A et al (2017) Differing clinical characteristics between young and older patients presenting with myocardial infarction. Heart Lung Circ 26(6):566–571
Pelletier R, Choi J, Winters N et al (2016) Sex differences in clinical outcomes after premature acute coronary syndrome. Can J Cardiol 32(12):1447–1453
Sabbag A, Matetzky S, Porter A et al (2017) Sex differences in the management and 5‑year outcome of young patients (〈55 years) with acute coronary syndromes. Am J Med 130(11):1324.e15–1324.e22
Ma Q, Wang J, Jin J et al (2017) Clinical characteristics and prognosis of acute coronary syndrome in young women and men: a systematic review and meta-analysis of prospective studies. Int J Cardiol 228:837–843
Andronescu AM, Delcea C, Enache V, Stamate CS, Dorobantu M (2014) Mean platelet volume variability in young patients with non-ST elevation acute myocardial infarction. J Med Life 7(Spec No. 3):107–113
Özlü MF, Öztürk S, Ayhan SS et al (2013) Predictive value of mean platelet volume in young patients with non-ST-segment elevation acute coronary syndromes: a retrospective observational study. Anadolu Kardiyol Derg 13(1):57–61
Tini G, Proietti G, Casenghi M et al (2017) Long-term outcome of acute coronary syndromes in young patients. High Blood Press Cardiovasc Prev 24(1):77–84
Trzeciak P, Gierlotka M, Poloński L, Gasior M (2017) Treatment and outcomes of patients under 40 years of age with acute myocardial infarction in Poland in 2009–2013: an analysis from the PL-ACS registry. Pol Arch Intern Med 127(10):666–673
Ren L, Ye H, Wang P, Cui Y, Cao S, Lv S (2014) Comparison of long-term mortality of acute ST-segment elevation myocardial infarction and non-ST-segment elevation acute coronary syndrome patients after percutaneous coronary intervention. Int J Clin Exp Med 7(12):5588–5592
Maroszyńska-Dmoch EM, Wożakowska-Kapłon B (2016) Clinical and angiographic characteristics of coronary artery disease in young adults: a single centre study. Kardiol Pol 74(4):314–321
Andrade PB, Rinaldi FS, Bienert IGC et al (2015) Clinical and angiographic profile of young patients undergoing primary percutaneous coronary intervention. Rev Bras Cardiol Invasiva 23(2):91–95
Landmesser U, Spiekermann S, Dikalov S et al (2002) Vascular oxidative stress and endothelial dysfunction in patients with chronic heart failure: role of xanthine-oxidase and extracellular superoxide dismutase. Circulation 106:3073–3078
Khosla UM, Zharikov S, Finch JL, Nakagawa T, Roncal C, Mu W, Krotova K, Block ER, Prabhakar S, Johnson RJ (2005) Hyperuricemia induces endothelial dysfunction. Kidney Int 67:1739–1742
Baldwin W, McRae S, Marek G et al (2011) Hyperuricemia as a mediator of the proinflammatory endocrine imbalance in the adipose tissue in a murine model of the metabolic syndrome. Diabetes 60:1258–1269
De Scheerder IK, van de Kraay AM, Lamers JM et al (1991) Myocardial malondialdehyde and uric acid release after short-lasting coronary occlusions during coronary angioplasty: potential mechanisms for free radical generation. Am J Cardiol 68:392–395
Alderman M, Aiyer KJ (2004) Uric acid: role in cardiovascular disease and effects of losartan. Curr Med Res Opin 20:369–379
Perlstein TS, Gumieniak O, Williams GH et al (2006) Uric acid and the development of hypertension: the normative aging study. Hypertension 48(6):1031–1036
Kodama S, Saito K, Yachi Y et al (2009) Association between serum uric acid and development of type 2 diabetes. Diabetes Care 32(9):1737–1742
Johnson RJ, Nakagawa T, Sanchez-Lozada LG et al (2013) Sugar, uric acid, and the etiology of diabetes and obesity. Diabetes 62:3307–3315
Soltani Z, Rasheed K, Kapusta DR, Reisin E (2013) Potential role of uric acid in metabolic syndrome, hypertension, kidney injury, and cardiovascular diseases: is it time for reappraisal? Curr Hypertens Rep 15(3):175–181
Bickel C, Rupprecht HJ, Blankenberg S et al (2002) Serum uric acid as an independent predictor of mortality in patients with angiographically proven coronary artery disease. Am J Cardiol 89(1):12–17
Anker SD, Doehner W, Rauchhaus M, Sharma R et al (2003) Uric acid and survival in chronic heart failure: validation and application in metabolic, functional, and hemodynamic staging. Circulation 107(15):1991–1997
Tscharre M, Herman R, Rohla M et al (2018) Uric acid is associated with long-term adverse cardiovascular outcomes in patients with acute coronary syndrome undergoing percutaneous coronary intervention. Atherosclerosis 270:173–179
Ndrepepa G, Braun S, Haase HU et al (2012) Prognostic value of uric acid in patients with acute coronary syndromes. Am J Cardiol 109(9):1260–1265
Timóteo AT, Lousinha A, Labandeiro J et al (2013) Serum uric acid: a forgotten prognostic marker in acute coronary syndromes? Eur Heart J Acute Cardiovasc Care 2(1):44–52
Culleton BF, Larson MG, Kannel WB, Levy D (1999) Serum uric acid and risk for cardiovascular disease and death: the Framingham Heart Study. Ann Intern Med 131(1):7–13
Lopez-Pineda A, Cordero A, Carratala-Munuera C et al (2018) Association analysis between hyperuricemia and long term mortality after acute coronary syndrome in three subgroups of patients. Data in Brief 17(5):885–889 (Feb)
Kojima S, Sakamoto T, Ishihara M et al (2005) Japanese Acute Coronary Syndrome Study (JACSS) Investigators. Prognostic usefulness of serum uric acid after acute myocardial infarction (the Japanese Acute Coronary Syndrome Study). Am J Cardiol 96:489–495
Funding
This research received no specific grant from any funding agency or from commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Y. Çanga, A. Emre, M.B. Karataş, A.N. Çalık, N.S. Yelgeç, D. İnan, G. Yüksel, and S. Terzi declare that they have no competing interests.
For this article no studies with human participants or animals were performed by any of the authors. All studies performed were in accordance with the ethical standards indicated in each case.
Rights and permissions
About this article
Cite this article
Çanga, Y., Emre, A., Karataş, M.B. et al. Prognostic value of serum uric acid levels in patients with non-STEMI undergoing percutaneous coronary intervention. Herz 45, 389–396 (2020). https://doi.org/10.1007/s00059-019-04849-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-019-04849-3