Abstract
Methylphenidate (MPH) is an amphetamine-like stimulant commonly prescribed for attention deficit hyperactivity disorder. Despite its widespread use, the cellular/molecular effects of MPH remain elusive. Here, we report a novel direct role of MPH on the regulation of macromolecular flux through human brain endothelial cells (ECs). MPH significantly increased caveolae-mediated transcytosis of horseradish peroxidase through ECs without affecting paracellular permeability. Using FRET-based live cell imaging, together with pharmacological inhibitors and lentiviral-mediated shRNA knockdown, we demonstrate that MPH promoted ROS generation via activation of Rac1-dependent NADPH oxidase (NOX) and c-Src activation at the plasma membrane. c-Src in turn was shown to mediate the phosphorylation of caveolin-1 (Cav1) on Tyr14 leading to enhanced caveolae formation and transendothelial transport. Accordingly, the inhibition of Cav1 phosphorylation by overexpression of a phosphodefective Cav1Y14F mutant or knocking down Cav1 expression abrogated MPH-induced transcytosis. In addition, both vitamin C and inhibition of NOX blocked MPH-triggered vesicular transport. This study, therefore, identifies Rac1/NOX/c-Src-dependent signaling in MPH-induced increase in transendothelial permeability of brain endothelial cell monolayers via caveolae-mediated transcytosis.







Similar content being viewed by others
Abbreviations
- ADHD:
-
Attention deficit hyperactivity disorder
- BBB:
-
Blood–brain barrier
- Cav1:
-
Caveolin-1
- ECs:
-
Endothelial cells
- HRP:
-
Horseradish peroxidase
- HBMVECs:
-
Human brain microvascular endothelial cells
- MPH:
-
Methylphenidate
- M-β-C:
-
Methyl-β-cyclodextrin
- NOX:
-
Nicotinamide adenine dinucleotide phosphate (NADPH) oxidase
- ROS:
-
Reactive oxygen species
- TEER:
-
Transendothelial electrical resistance
- TJs:
-
Tight junctions
- VitC:
-
Vitamin C
References
Sharma A, Couture J (2014) A review of the pathophysiology, etiology, and treatment of attention-deficit hyperactivity disorder (ADHD). Ann Pharmacother 48(2):209–225. doi:10.1177/1060028013510699
Elder TE (2010) The importance of relative standards in ADHD diagnoses: evidence based on exact birth dates. J Health Econ 29(5):641–656. doi:10.1016/j.jhealeco.2010.06.003
Sahakian BJ, Bruhl AB, Cook J, Killikelly C, Savulich G, Piercy T, Hafizi S, Perez J, Fernandez-Egea E, Suckling J, Jones PB (2015) The impact of neuroscience on society: cognitive enhancement in neuropsychiatric disorders and in healthy people. Philos Trans R Soc Lond B Biol Sci 370(1677):20140214. doi:10.1098/rstb.2014.0214
Cardoso FL, Brites D, Brito MA (2010) Looking at the blood–brain barrier: molecular anatomy and possible investigation approaches. Brain Res Rev 64(2):328–363. doi:10.1016/j.brainresrev.2010.05.003
Cipolla MJ, Crete R, Vitullo L, Rix RD (2004) Transcellular transport as a mechanism of blood–brain barrier disruption during stroke. Front Biosci 9:777–785
Sverdlov M, Shajahan AN, Minshall RD (2007) Tyrosine phosphorylation-dependence of caveolae-mediated endocytosis. J Cell Mol Med 11(6):1239–1250. doi:10.1111/j.1582-4934.2007.00127.x
Chang CF, Chen SF, Lee TS, Lee HF, Chen SF, Shyue SK (2011) Caveolin-1 deletion reduces early brain injury after experimental intracerebral hemorrhage. Am J Pathol 178(4):1749–1761. doi:10.1016/j.ajpath.2010.12.023
Gaudreault SB, Dea D, Poirier J (2004) Increased caveolin-1 expression in Alzheimer’s disease brain. Neurobiol Aging 25(6):753–759. doi:10.1016/j.neurobiolaging.2003.07.004
Head BP, Patel HH (1838) Insel PA (2014) Interaction of membrane/lipid rafts with the cytoskeleton: impact on signaling and function: membrane/lipid rafts, mediators of cytoskeletal arrangement and cell signaling. Biochim Biophys Acta 2:532–545. doi:10.1016/j.bbamem.2013.07.018
Fernandez I, Ying Y, Albanesi J, Anderson RG (2002) Mechanism of caveolin filament assembly. Proc Natl Acad Sci USA 99(17):11193–11198. doi:10.1073/pnas.172196599
Zimnicka AM, Husain YS, Shajahan AN, Sverdlov M, Chaga O, Chen Z, Toth PT, Klomp J, Karginov AV, Tiruppathi C, Malik AB, Minshall RD (2016) Src-dependent phosphorylation of caveolin-1 Tyr14 promotes swelling and release of caveolae. Mol Biol Cell. doi:10.1091/mbc.E15-11-0756
Rosenberg GA (2012) Neurological diseases in relation to the blood–brain barrier. J Cereb Blood Flow Metab 32(7):1139–1151. doi:10.1038/jcbfm.2011.197
Marquand AF, O’Daly OG, De Simoni S, Alsop DC, Maguire RP, Williams SC, Zelaya FO, Mehta MA (2012) Dissociable effects of methylphenidate, atomoxetine and placebo on regional cerebral blood flow in healthy volunteers at rest: a multi-class pattern recognition approach. Neuroimage 60(2):1015–1024. doi:10.1016/j.neuroimage.2012.01.058
Bahcelioglu M, Gozil R, Take G, Elmas C, Oktem H, Kadioglu D, Calguner E, Erdogan D, Sargon MF, Yazici AC, Tas M, Bardakci Y, Senol S (2009) Dose-related immunohistochemical and ultrastructural changes after oral methylphenidate administration in cerebrum and cerebellum of the rat. World J Biol Psychiatry 10(4 Pt 2):531–543. doi:10.1080/15622970903176683
Bernas MJ, Cardoso FL, Daley SK, Weinand ME, Campos AR, Ferreira AJ, Hoying JB, Witte MH, Brites D, Persidsky Y, Ramirez SH, Brito MA (2010) Establishment of primary cultures of human brain microvascular endothelial cells to provide an in vitro cellular model of the blood–brain barrier. Nat Protoc 5(7):1265–1272. doi:10.1038/nprot.2010.76
Weksler BB, Subileau EA, Perriere N, Charneau P, Holloway K, Leveque M, Tricoire-Leignel H, Nicotra A, Bourdoulous S, Turowski P, Male DK, Roux F, Greenwood J, Romero IA, Couraud PO (2005) Blood–brain barrier-specific properties of a human adult brain endothelial cell line. FASEB J 19(13):1872–1874. doi:10.1096/fj.04-3458fje
Socodato R, Portugal CC, Canedo T, Domith I, Oliveira NA, Paes-de-Carvalho R, Relvas JB, Cossenza M (2015) c-Src deactivation by the polyphenol 3-O-caffeoylquinic acid abrogates reactive oxygen species-mediated glutamate release from microglia and neuronal excitotoxicity. Free Radic Biol Med 79:45–55. doi:10.1016/j.freeradbiomed.2014.11.019
Coelho-Santos V, Leitao RA, Cardoso FL, Palmela I, Rito M, Barbosa M, Brito MA, Fontes-Ribeiro CA, Silva AP (2015) The TNF-alpha/NF-kappaB signaling pathway has a key role in methamphetamine-induced blood-brain barrier dysfunction. J Cereb Blood Flow Metab 35(8):1260–1271. doi:10.1038/jcbfm.2015.59
Martins T, Burgoyne T, Kenny BA, Hudson N, Futter CE, Ambrosio AF, Silva AP, Greenwood J, Turowski P (2013) Methamphetamine-induced nitric oxide promotes vesicular transport in blood–brain barrier endothelial cells. Neuropharmacology 65:74–82. doi:10.1016/j.neuropharm.2012.08.021
Fernandes S, Salta S, Bravo J, Silva AP, Summavielle T (2016) Acetyl-l-carnitine prevents methamphetamine-induced structural damage on endothelial cells via ILK-related MMP-9 activity. Mol Neurobiol 53(1):408–422. doi:10.1007/s12035-014-8973-5
Gopal KV, Miller BR, Gross GW (2007) Acute and sub-chronic functional neurotoxicity of methylphenidate on neural networks in vitro. J Neural Transm 114(11):1365–1375. doi:10.1007/s00702-007-0759-8
Balcioglu A, Ren JQ, McCarthy D, Spencer TJ, Biederman J, Bhide PG (2009) Plasma and brain concentrations of oral therapeutic doses of methylphenidate and their impact on brain monoamine content in mice. Neuropharmacology 57(7–8):687–693. doi:10.1016/j.neuropharm.2009.07.025
Phan NT, Hanrieder J, Berglund EC, Ewing AG (2013) Capillary electrophoresis-mass spectrometry-based detection of drugs and neurotransmitters in Drosophila brain. Anal Chem 85(17):8448–8454. doi:10.1021/ac401920v
Huff JK, Davies MI (2002) Microdialysis monitoring of methylphenidate in blood and brain correlated with changes in dopamine and rat activity. J Pharm Biomed Anal 29(5):767–777
Matter K, Balda MS (2003) Functional analysis of tight junctions. Methods 30(3):228–234. doi:10.1016/S1046-2023(03)00029-X
Hasebe R, Suzuki T, Makino Y, Igarashi M, Yamanouchi S, Maeda A, Horiuchi M, Sawa H, Kimura T (2010) Transcellular transport of West Nile virus-like particles across human endothelial cells depends on residues 156 and 159 of envelope protein. BMC Microbiol 10:165. doi:10.1186/1471-2180-10-165
Stamatovic SM, Keep RF, Wang MM, Jankovic I, Andjelkovic AV (2009) Caveolae-mediated internalization of occludin and claudin-5 during CCL2-induced tight junction remodeling in brain endothelial cells. J Biol Chem 284(28):19053–19066. doi:10.1074/jbc.M109.000521
Sun Y, Hu G, Zhang X, Minshall RD (2009) Phosphorylation of caveolin-1 regulates oxidant-induced pulmonary vascular permeability via paracellular and transcellular pathways. Circ Res 105(7):676–685, 615 p following 685. doi:10.1161/CIRCRESAHA.109.201673
Maniatis NA, Kardara M, Hecimovich D, Letsiou E, Castellon M, Roussos C, Shinin V, Votta-Vellis EG, Schwartz DE, Minshall RD (2012) Role of caveolin-1 expression in the pathogenesis of pulmonary edema in ventilator-induced lung injury. Pulm Circ 2(4):452–460. doi:10.4103/2045-8932.105033
Vihanto MM, Vindis C, Djonov V, Cerretti DP, Huynh-Do U (2006) Caveolin-1 is required for signaling and membrane targeting of EphB1 receptor tyrosine kinase. J Cell Sci 119(Pt 11):2299–2309. doi:10.1242/jcs.02946
Park M, Hennig B, Toborek M (2012) Methamphetamine alters occludin expression via NADPH oxidase-induced oxidative insult and intact caveolae. J Cell Mol Med 16(2):362–375. doi:10.1111/j.1582-4934.2011.01320.x
Long M, Huang SH, Wu CH, Shackleford GM, Jong A (2012) Lipid raft/caveolae signaling is required for Cryptococcus neoformans invasion into human brain microvascular endothelial cells. J Biomed Sci 19:19. doi:10.1186/1423-0127-19-19
Lim JS, Shin M, Kim HJ, Kim KS, Choy HE, Cho KA (2014) Caveolin-1 mediates Salmonella invasion via the regulation of SopE-dependent Rac1 activation and actin reorganization. J Infect Dis 210(5):793–802. doi:10.1093/infdis/jiu152
Ouyang M, Sun J, Chien S, Wang Y (2008) Determination of hierarchical relationship of Src and Rac at subcellular locations with FRET biosensors. Proc Natl Acad Sci USA 105(38):14353–14358. doi:10.1073/pnas.0807537105
Gomes KM, Inacio CG, Valvassori SS, Reus GZ, Boeck CR, Dal-Pizzol F, Quevedo J (2009) Superoxide production after acute and chronic treatment with methylphenidate in young and adult rats. Neurosci Lett 465(1):95–98. doi:10.1016/j.neulet.2009.08.060
Martins MR, Reinke A, Petronilho FC, Gomes KM, Dal-Pizzol F (1078) Quevedo J (2006) Methylphenidate treatment induces oxidative stress in young rat brain. Brain Res 1:189–197. doi:10.1016/j.brainres.2006.01.004
Hu G, Vogel SM, Schwartz DE, Malik AB, Minshall RD (2008) Intercellular adhesion molecule-1-dependent neutrophil adhesion to endothelial cells induces caveolae-mediated pulmonary vascular hyperpermeability. Circ Res 102(12):e120–e131. doi:10.1161/CIRCRESAHA.107.167486
Frey RS, Ushio-Fukai M, Malik AB (2009) NADPH oxidase-dependent signaling in endothelial cells: role in physiology and pathophysiology. Antioxid Redox Signal 11(4):791–810. doi:10.1089/ARS.2008.2220
Stielow C, Catar RA, Muller G, Wingler K, Scheurer P, Schmidt HH, Morawietz H (2006) Novel Nox inhibitor of oxLDL-induced reactive oxygen species formation in human endothelial cells. Biochem Biophys Res Commun 344(1):200–205. doi:10.1016/j.bbrc.2006.03.114
Chen W, Pendyala S, Natarajan V, Garcia JG, Jacobson JR (2008) Endothelial cell barrier protection by simvastatin: GTPase regulation and NADPH oxidase inhibition. Am J Physiol Lung Cell Mol Physiol 295(4):L575–L583. doi:10.1152/ajplung.00428.2007
Giannoni E, Buricchi F, Raugei G, Ramponi G, Chiarugi P (2005) Intracellular reactive oxygen species activate Src tyrosine kinase during cell adhesion and anchorage-dependent cell growth. Mol Cell Biol 25(15):6391–6403. doi:10.1128/MCB.25.15.6391-6403.2005
Coyne CB, Kim KS, Bergelson JM (2007) Poliovirus entry into human brain microvascular cells requires receptor-induced activation of SHP-2. EMBO J 26(17):4016–4028. doi:10.1038/sj.emboj.7601831
Hopkins AM, Walsh SV, Verkade P, Boquet P, Nusrat A (2003) Constitutive activation of Rho proteins by CNF-1 influences tight junction structure and epithelial barrier function. J Cell Sci 116(Pt 4):725–742
Song L, Ge S, Pachter JS (2007) Caveolin-1 regulates expression of junction-associated proteins in brain microvascular endothelial cells. Blood 109(4):1515–1523. doi:10.1182/blood-2006-07-034009
Li Y, Liu LB, Ma T, Wang P, Xue YX (2015) Effect of caveolin-1 on the expression of tight junction-associated proteins in rat glioma-derived microvascular endothelial cells. Int J Clin Exp Pathol 8(10):13067–13074
Gomes KM, Petronilho FC, Mantovani M, Garbelotto T, Boeck CR, Dal-Pizzol F, Quevedo J (2008) Antioxidant enzyme activities following acute or chronic methylphenidate treatment in young rats. Neurochem Res 33(6):1024–1027. doi:10.1007/s11064-007-9544-1
Kahles T, Luedike P, Endres M, Galla HJ, Steinmetz H, Busse R, Neumann-Haefelin T, Brandes RP (2007) NADPH oxidase plays a central role in blood–brain barrier damage in experimental stroke. Stroke 38(11):3000–3006. doi:10.1161/STROKEAHA.107.489765
Han M, Pendem S, Teh SL, Sukumaran DK, Wu F, Wilson JX (2010) Ascorbate protects endothelial barrier function during septic insult: Role of protein phosphatase type 2A. Free Radic Biol Med 48(1):128–135. doi:10.1016/j.freeradbiomed.2009.10.034
Nimnual AS, Taylor LJ, Bar-Sagi D (2003) Redox-dependent downregulation of Rho by Rac. Nat Cell Biol 5(3):236–241. doi:10.1038/ncb938
Zaas DW, Duncan M, Rae Wright J, Abraham SN (2005) The role of lipid rafts in the pathogenesis of bacterial infections. Biochim Biophys Acta 1746(3):305–313. doi:10.1016/j.bbamcr.2005.10.003
Persidsky Y, Heilman D, Haorah J, Zelivyanskaya M, Persidsky R, Weber GA, Shimokawa H, Kaibuchi K, Ikezu T (2006) Rho-mediated regulation of tight junctions during monocyte migration across the blood–brain barrier in HIV-1 encephalitis (HIVE). Blood 107(12):4770–4780. doi:10.1182/blood-2005-11-4721
Wojciak-Stothard B, Potempa S, Eichholtz T, Ridley AJ (2001) Rho and Rac but not Cdc42 regulate endothelial cell permeability. J Cell Sci 114(Pt 7):1343–1355
Carbajal JM, Schaeffer RC Jr (1999) RhoA inactivation enhances endothelial barrier function. Am J Physiol 277(5 Pt 1):C955–C964
Birukova AA, Zebda N, Cokic I, Fu P, Wu T, Dubrovskyi O, Birukov KG (2011) p190RhoGAP mediates protective effects of oxidized phospholipids in the models of ventilator-induced lung injury. Exp Cell Res 317(6):859–872. doi:10.1016/j.yexcr.2010.11.011
Hu G, Place AT, Minshall RD (2008) Regulation of endothelial permeability by Src kinase signaling: vascular leakage versus transcellular transport of drugs and macromolecules. Chem Biol Interact 171(2):177–189. doi:10.1016/j.cbi.2007.08.006
Liang S, Pong K, Gonzales C, Chen Y, Ling HP, Mark RJ, Boschelli F, Boschelli DH, Ye F, Barrios Sosa AC, Mansour TS, Frost P, Wood A, Pangalos MN, Zaleska MM (2009) Neuroprotective profile of novel SRC kinase inhibitors in rodent models of cerebral ischemia. J Pharmacol Exp Ther 331(3):827–835. doi:10.1124/jpet.109.156562
Acknowledgments
This work was supported by Project PTDC/NEU-OSD/0312/2012 from Foundation for Science and Technology (FCT Portugal) co-financed by COMPETE and FEDER funds, and strategic projects PEST-C/SAU/UI3282/2013 and UID/NEU/04539/2013. Also, Ph.D. fellowships SFRH/BD/85556/2012 and SFRH/BD/84408/2012 and, postdoctoral fellowship SFRH/BPD/91833/2012 and SFRH/BPD/91962/2012 from FCT Portugal co-financed by QREN. TSummavielle was supported by program Investigador FCT, POPH and Fundo Social Europeu, and RDMinshall by NIH P01 HL60678. We thank Dr. Shu Chien (University of California, San Diego) for providing KRas Src YPet and KRas Src (RV) YPet FRET probes. We thank Dr. Michiyuki Matsuda (Kyoto University) for kindly sharing with us the Raichu-RhoA, Raichu-Rac1 and Raichu-cdc42 FRET probes, and Dr. Andrei Karginov (University of Illinois, Chicago) for providing the RapR-Src construct.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
18_2016_2301_MOESM1_ESM.tif
Supplementary Fig. 1 Effect of MPH on ECs viability. HBMVECs were exposed to increasing MPH concentrations (0.001-3 mM) for (a) 24 h or (b) 48 h to evaluate cell death. MPH increased the number of TUNEL-positive cells to concentration above 3 or 1 mM for 24 or 48 h of exposure, respectively. (c) hCMEC/D3 cells were incubated with MPH (100 µM) during 3, 24, and 48 h, and no cell death was observed at any time-point analyzed. The results are expressed as mean % of control ± S.E.M., n=11-24. *P<0.05, **P<0.01, ***P<0.001, significantly different when compared to the control using Dunnett’s Multiple comparison test (TIFF 5386 kb)
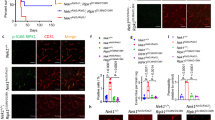
18_2016_2301_MOESM2_ESM.tif
Supplementary Fig. 2 Impact of MPH on Rac1, RhoA, and Cdc42 GTPases activity analyzed by a pull-down assay. hCMEC/D3 cells were exposed to MPH (100 µM) during 30 min (TIFF 1541 kb)
Rights and permissions
About this article
Cite this article
Coelho-Santos, V., Socodato, R., Portugal, C. et al. Methylphenidate-triggered ROS generation promotes caveolae-mediated transcytosis via Rac1 signaling and c-Src-dependent caveolin-1 phosphorylation in human brain endothelial cells. Cell. Mol. Life Sci. 73, 4701–4716 (2016). https://doi.org/10.1007/s00018-016-2301-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00018-016-2301-3