Abstract
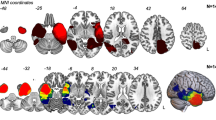
The state of the art in contemporary glioma surgery is the irremediable fight between anatomic, supramarginal and functional tumor resections. All our efforts are focused on increasing the ‘progression-free survival’ but not at any cost, as the neurological function preservation is nowadays considered as a must. Low grade glioma patients are now considered as long survivors, who should be able to continue with their normal lives after surgical treatments for a long time. Therefore, achieving supramarginal resections, by predicting, detecting and respecting the eloquent areas of the human brain represents the gold-standard on glioma surgery. In this sense, preserving the visual function is of extreme importance, especially in those patients whose daily routine requires a normal visual field. Visual pathways represent a complex anatomy not easily recognizable into the surgical field due to its depth and different directions followed into the periventricular areas. We present our protocol and results after implementing a novel method to detect the optic radiations based on preoperative MRI images and an original intraoperative campimetry implemented to the subcortical stimulation device. The use of this method has allowed us to maximize our resections, as well as to decide the safest surgical trajectory in certain cases.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
González-Darder JM, González-López P. Management of Brain Tumors in eloquent areas. In: Abujamra AL, editor. Diagnostic techniques and surgical management of brain tumors. InTech; 2011. https://doi.org/10.5772/21796.
Ferracci FX, Duffau H. Improving surgical outcome for gliomas with intraoperative mapping. Expert Rev Neurother. 2018;18(4):333–41. https://doi.org/10.1080/14737175.2018.1451329. Epub 2018 Mar 20
Duffau H. Preserving quality of life is not incompatible with increasing overall survival in diffuse low-grade glioma patients. Acta Neurochir. 2015;157:165–7.
Soffietti R, Baumert BG, Bello L, Von Deimling A, Duffau H, Frénay M, Grisold W, Grant R, Graus F, Hoang-Xuan K, Klein M, Melin B, Rees J, Siegal T, Smits A, Stupp R, Wick W. Guidelines on management of low-grade gliomas: report of an EFNS-EANO task force. Eur J Neurol. 2010 Sep;17(9):1124–33. https://doi.org/10.1111/j.1468-1331.2010.03151.x.
Duffau H, Mandonnet E. The “onco-functional balance” in surgery for diffuse low-grade glioma: integrating the extent of resection with quality of life. Acta Neurochir. 2013;155(6):951–7. https://doi.org/10.1007/s00701-013-1653-9. Epub 2013 Feb 28
Duffau H. Surgery for diffuse low-grade gliomas (DLGG) functional Ouctomes. In: Duffau H, editor. Diffuse low-grade gliomas in adults. Springer; 2013. p. 497–533.
Gogos AJ, Young JS, Morshed RA, Hervey-Jumper SL, Berger MS. Awake glioma surgery: technical evolution and nuances. J Neuro-Oncol. 2020;147(3):515–24. https://doi.org/10.1007/s11060-020-03482-z. Epub 2020 Apr 8
Bartholow R. Experimental investigations into the functions of the human brain. Am J Med Sci. 1874;7:305–13.
Penfeld W, Boldrey E. Somatic motor and sensory representation in the cerebral cortex of man as studied by electrical stimulation. Brain. 1937;60(4):389–443. https://doi.org/10.1093/brain/60.4.38919.
Whitaker HA, Ojemann GA. Graded localisation of naming from electrical stimulation mapping of left cerebral cortex. Nature. 1977;270(5632):50–1. https://doi.org/10.1038/270050a0.
Berger MS, Kincaid J, Ojemann GA, Lettich E. Brain mapping techniques to maximize resection, safety, and seizure control in children with brain tumors. Neurosurgery. 1989;25(5):786–92. https://doi.org/10.1097/00006123-198911000-00015.
Sincoff EH, Tan Y, Abdulrauf SI. White matter fiber dissection of the optic radiations of the temporal lobe and implications for surgical approaches to the temporal horn. J Neurosurg. 2004;101(5):739–46. https://doi.org/10.3171/jns.2004.101.5.0739.
Peltier J, Travers N, Destrieux C, Velut S. Optic radiations: a microsurgical anatomical study. J Neurosurg. 2006;105(2):294–300. https://doi.org/10.3171/jns.2006.105.2.294.
Shah A, Goel A, Jhawar SS, Patil A, Rangnekar R, Goel A. Neural circuitry: architecture and function - a Fiber dissection study. World Neursurg. 2019;125:eg20–e638.
Shah A, Jhawar SS, Goel A. Letter to the editor: optic radiations and anterior commissure. J Neurosurg. 2015;123(3):824–6.
Peuskens D, van Loon J, Van Calenbergh F, van den Bergh R, Goffin J, Plets C. Anatomy of the anterior temporal lobe and the frontotemporal region demonstrated by fiber dissection. Neurosurgery. 2004;55(5):1174–84. https://doi.org/10.1227/01.neu.0000140843.62311.24.
Mahaney KB, Abdulrauf SI. Anatomic relationship of the optic radiations to the atrium of the lateral ventricle: description of a novel entry point to the trigone. Neurosurgery. 2008;63(4 Suppl 2):195–202; discussion 202–3. https://doi.org/10.1227/01.NEU.0000313121.58694.4A.
Fernández-Miranda JC, Rhoton AL Jr, Alvarez-Linera J, Kakizawa Y, Choi C, de Oliveira EP. Three-dimensional microsurgical and tractographic anatomy of the white matter of the human brain. Neurosurgery. 2008;62(6 Suppl 3):989–1026; discussion 1026-8. https://doi.org/10.1227/01.neu.0000333767.05328.49.
Türe U, Yaşargil MG, Friedman AH, Al-Mefty O. Fiber dissection technique: lateral aspect of the brain. Neurosurgery. 2000;47(2):417–26; discussion 426–7. https://doi.org/10.1097/00006123-200008000-00028.
Yasargil MG, Türe U, Yasargil DC. Impact of temporal lobe surgery. J Neurosurg. 2004;101(5):725–38. https://doi.org/10.3171/jns.2004.101.5.0725.
Maldonado IL, Destrieux C, Ribas EC, de Abreu S, Brito Guimarães B, Cruz PP, Duffau H. Composition and organization of the sagittal stratum in the human brain: a fiber dissection study. J Neurosurg. 2021;8:1–9. https://doi.org/10.3171/2020.7.JNS192846. Epub ahead of print
Kiviranta P. Mapping the visual field: an empirical study on the user experience benefits of gaze-based interaction in visual field testing. [MDP in human-technology interaction, University of Tampere] 2017. http://urn.fi/URN:NBN:fi:uta-201710092561
Wolfson R, Soni N, Shah AH, Hosein K, Sastry A, Bregy A, Komotar RJ. The role of awake craniotomy in reducing intraoperative visual field deficits during tumor surgery. Asian. J Neurosurg. 2015;10(3):139–44. https://doi.org/10.4103/1793-5482.161189.
Bartos R, Jech R, Vymazal J, Petrovický P, Vachata P, Hejcl A, et al. Validity of primary motor area localization with fMRI versus electric cortical stimulation: a comparative study. Acta Neurochir. 2009;151:1071–80.
Petrovich N, Holodny AI, Tabar V, Correa DD, Hirsch J, Gutin PH, et al. Discordance between functional magnetic resonance imaging during silent speech tasks and intraoperative speech arrest. J Neurosurg. 2005;103:267–74.
Kuchcinski G, Mellerio C, Pallud J, Dezamis E, Turc G, Rigaux-Viodé O, et al. Three-tesla functional MR language mapping: comparison with direct cortical stimulation in gliomas. Neurology. 2015;84:560–8.
Duffau H. Awake mapping and tumor surgery. In: Duffau H, editor. Brain mapping. Springer; 2011. https://doi.org/10.1007/978-3-7091-0723-2_24.
Kollias SS. Functional magnetic resonance imaging of the human visual system. In: Baert AL, Sartor K, Müller-Forell WS, editors. Imaging of orbital and visual pathway pathology. Medical radiology (diagnostic imaging). Berlin, Heidelberg: Springer; 2006. https://doi.org/10.1007/3-540-27989-X_4.
Dumoulin S. Functional MRI of the visual system. In: Uludag K, Ugurbil K, Berliner L, editors. fMRI: from nuclear spins to brain functions. Biological magnetic resonance, vol 30. Boston, MA: Springer; 2015. https://doi.org/10.1007/978-1-4899-7591-1_15.
Hana A, Husch A, Gunness VR, Berthold C, Hana A, Dooms G, Boecher Schwarz H, Hertel F. DTI of the visual pathway–white matter tracts and cerebral lesions. J Vis Exp. 2014;90:51946. https://doi.org/10.3791/51946.
Feigl GC, Hiergeist W, Fellner C, Schebesch KM, Doenitz C, Finkenzeller T, et al. Magnetic resonance imaging diffusion tensor tractography: evaluation of anatomic accuracy of different fiber tracking software packages. World Neurosurg. 2014;81:144–50.
Gras-Combe G, Moritz-Gasser S, Herbet G, Duffau H. Intraoperative subcortical electrical mapping of optic radiations in awake surgery for glioma involving visual pathways. J Neurosurg. 2012;117(3):466–73. https://doi.org/10.3171/2012.6.JNS111981. Epub 2012 Jul 13
Pujol S, Wells W, Pierpaoli C, Brun C, Gee J, Cheng G, et al. The DTI challenge: toward standardized evaluation of diffusion tensor imaging tractography for neurosurgery. J Neuroimaging. 2015;25:875–82.
Kinoshita M, Yamada K, Hashimoto N, Kato A, Izumoto S, Baba T, et al. Fiber-tracking does not accurately estimate size of fiber bundle in pathological condition: initial neurosurgical experience using neuronavigation and subcortical white matter stimulation. NeuroImage. 2005;25:424–9.
Leclercq D, Duffau H, Delmaire C, Capelle L, Gatignol P, Ducros M, Chiras J, Lehéricy S. Comparison of diffusion tensor imaging tractography of language tracts and intraoperative subcortical stimulations. J Neurosurg. 2010;112:503–11.
Duffau H. The dangers of magnetic resonance imaging diffusion tensor tractography in brain surgery. World Neurosurg. 2014;81:56–8.
Creel DJ. Visually evoked potentials. Handb Clin Neurol. 2019;160:501–22. https://doi.org/10.1016/B978-0-444-64032-1.00034-5.
Visually CD, Potentials E. In: Kolb H, Fernandez E, Nelson R, editors. Webvision: the organization of the retina and visual system [internet]. Salt Lake City (UT): University of Utah Health Sciences Center; 2012. p. 1995.
Sharma R, Joshi S, Singh KD, Kumar A. Visual evoked Potentials: normative values and gender differences. J Clin Diagn Res. 2015;9(7):CC12–5. https://doi.org/10.7860/JCDR/2015/12764.6181. Epub 2015 Jul 1
Fountas K, Kapsalaki EZ. Surgical management of occipital gliomas: a practical atlas. In: Fountas K, Kapsalaki EZ, editors. Epilepsy surgery and intrinsic brain tumor surgery. Springer; 2019.
Verst SM, et al. Awake surgery versus VEP in tumors of visual pathway: case report. Interdisciplinary Neurosurg. 2020;20:100675.
Shahar T, Korn A, Barkay G, Biron T, Hadanny A, Gazit T, Nossek E, Ekstein M, Kesler A, Ram Z. Elaborate mapping of the posterior visual pathway in awake craniotomy. J Neurosurg. 2018;128(5):1503–11. https://doi.org/10.3171/2017.2.JNS162757. Epub 2017 Aug 25
Ota T, Kawai K, Kamada K, Kin T, Saito N. Intraoperative monitoring of cortically recorded visual response for posterior visual pathway. J Neurosurg. 2010;112:285–94.
Steňo A, Hollý V, Fabian M, Kuniak M, Timárová G, Steňo J. Direct electrical stimulation of the optic radiation in patients with covered eyes. Neurosurg Rev. 2014;37(3):527–33. https://doi.org/10.1007/s10143-014-0535-9. discussion 533. Epub 2014 Feb 28
Duffau H, Velut S, Mitchell MC, Gatignol P, Capelle L. Intra-operative mapping of the subcortical visual pathways using direct electrical stimulations. Acta Neurochir. 2004;146(3):265–9. https://doi.org/10.1007/s00701-003-0199-7. discussion 269–70. Epub 2004 Jan 8
Chan-Seng E, Moritz-Gasser S, Duffau H. Awake mapping for low-grade gliomas involving the left sagittal stratum: anatomofunctional and surgical considerations. J Neurosurg. 2014;120(5):1069–77. https://doi.org/10.3171/2014.1.JNS132015. Epub 2014 Jan 31
Nguyen HS, Sundaram SV, Mosier KM, Cohen-Gadol AA. A method to map the visual cortex during an awake craniotomy. J Neurosurg. 2011;114(4):922–6. https://doi.org/10.3171/2010.11.JNS101293. Epub 2011 Jan 14
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Gonzalez-Lopez, P., Martorell-Llobregat, C., Piqueres, M.D.C., Fernández, E. (2023). Optic Radiations Monitoring in Awake Glioma Surgery: Intraoperative Campimetry. In: Shah, A., Goel, A., Kato, Y. (eds) Functional Anatomy of the Brain: A View from the Surgeon’s Eye. Springer, Singapore. https://doi.org/10.1007/978-981-99-3412-6_7
Download citation
DOI: https://doi.org/10.1007/978-981-99-3412-6_7
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-99-3411-9
Online ISBN: 978-981-99-3412-6
eBook Packages: MedicineMedicine (R0)