Abstract
The female reproductive tract has its embryological origins in the paired Müllerian ducts and their fusion to each other and the urogenital sinus. The Müllerian ducts give rise to the oviducts, uterus, and cervix, while the urogenital sinus forms the vagina and external genitalia. Primordial germ cells formed near the yolk sac migrate to colonize the gonadal ridge, where in females interactions between germ and somatic cells coalesce to create the functional ovarian units known as follicles.
A classical morphologic understanding of the embryology of these structures has served as the foundation for a general understanding of myriad conditions due to maldevelopment or malignant transformation. Increasingly, the molecular underpinnings of these complex underlying developmental transformations are being revealed, yielding deeper insights into the biological basis of female reproductive tract disease pathophysiology and also providing many useful markers, such as Sall4, Foxl2, Wt1, and Pax8, routinely used in clinical practice. In some cases, Müllerian maldevelopment syndromes such as Müllerian agenesis are now known to be caused by mutations in the genes encoding factors required for Müllerian duct development.
The once far-fetched idea that epithelial cells of the oviduct—not the ovary itself—are the origin of most “ovarian” carcinomas now has universal acceptance. Female reproductive tract malignancies of the cervix, uterus, and ovary recently believed to have disparate cellular/embryologic origins are now understood to have a shared origin in the epithelial lining of the Müllerian ducts. This insight rationalizes many prior observations, for example, that the diverse tumor histotypes common to the cervix, endometrium, or tubo-ovarian complex are encountered across each site. This chapter summarizes our understanding of female gonadal and reproductive tract development, with an emphasis on morphologic and molecular aspects that currently appear most relevant to disease pathophysiology.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Dansereau DA, Lasko P. The development of germline stem cells in Drosophila. Methods Mol Biol. 2008;450:3–26. https://doi.org/10.1007/978-1-60327-214-8_1.
Kumar DL, DeFalco T. Of mice and men: in vivo and in vitro studies of primordial germ cell specification. Semin Reprod Med. 2017;35(2):139–46. https://doi.org/10.1055/s-0037-1599085.
De Felici M. Origin, migration, and proliferation of human primordial germ cells. In: Coticchio G, Albertini DF, De Santis L, editors. Oogenesis. London: Springer; 2013. p. 19–38. https://doi.org/10.1007/978-0-85729-826-3.
McKay DG, Hertig AT, Adams EC, Danziger S. Histochemical observations on the germ cells of human embryos. Anat Rec. 1953;117(2):201–19.
Castrillon DH, Quade BJ, Wang TY, Quigley C, Crum CP. The human VASA gene is specifically expressed in the germ cell lineage. Proc Natl Acad Sci U S A. 2000;97(17):9585–90. https://doi.org/10.1073/pnas.160274797.
De Felici M. Regulation of primordial germ cell development in the mouse. Int J Dev Biol. 2000;44(6):575–80.
Mollgard K, Jespersen A, Lutterodt MC, Yding Andersen C, Hoyer PE, Byskov AG. Human primordial germ cells migrate along nerve fibers and Schwann cells from the dorsal hind gut mesentery to the gonadal ridge. Mol Hum Reprod. 2010;16(9):621–31. https://doi.org/10.1093/molehr/gaq052.
Eildermann K, Aeckerle N, Debowski K, Godmann M, Christiansen H, Heistermann M, Schweyer S, Bergmann M, Kliesch S, Gromoll J, Ehmcke J, Schlatt S, Behr R. Developmental expression of the pluripotency factor sal-like protein 4 in the monkey, human and mouse testis: restriction to premeiotic germ cells. Cells Tissues Organs. 2012;196(3):206–20. https://doi.org/10.1159/000335031.
Mamsen LS, Brochner CB, Byskov AG, Mollgard K. The migration and loss of human primordial germ stem cells from the hind gut epithelium towards the gonadal ridge. Int J Dev Biol. 2012;56(10–12):771–8. https://doi.org/10.1387/ijdb.120202lm.
Hoyer PE, Byskov AG, Mollgard K. Stem cell factor and c-Kit in human primordial germ cells and fetal ovaries. Mol Cell Endocrinol. 2005;234(1–2):1–10. https://doi.org/10.1016/j.mce.2004.09.012.
Tanaka SS, Yamaguchi YL, Tsoi B, Lickert H, Tam PP. IFITM/Mil/fragilis family proteins IFITM1 and IFITM3 play distinct roles in mouse primordial germ cell homing and repulsion. Dev Cell. 2005;9(6):745–56. https://doi.org/10.1016/j.devcel.2005.10.010.
Chaganti RS, Rodriguez E, Mathew S. Origin of adult male mediastinal germ-cell tumours. Lancet. 1994;343(8906):1130–2.
Sanchez A, Amatruda JF. Zebrafish germ cell Tumors. Adv Exp Med Biol. 2016;916:479–94. https://doi.org/10.1007/978-3-319-30654-4_21.
Yamashiro C, Hirota T, Kurimoto K, Nakamura T, Yabuta Y, Nagaoka SI, Ohta H, Yamamoto T, Saitou M. Persistent requirement and alteration of the key targets of PRDM1 during primordial germ cell development in mice. Biol Reprod. 2016;94(1):7. https://doi.org/10.1095/biolreprod.115.133256.
Ohinata Y, Payer B, O’Carroll D, Ancelin K, Ono Y, Sano M, Barton SC, Obukhanych T, Nussenzweig M, Tarakhovsky A, Saitou M, Surani MA. Blimp1 is a critical determinant of the germ cell lineage in mice. Nature. 2005;436(7048):207–13. https://doi.org/10.1038/nature03813.
Tang WW, Kobayashi T, Irie N, Dietmann S, Surani MA. Specification and epigenetic programming of the human germ line. Nat Rev Genet. 2016;17(10):585–600. https://doi.org/10.1038/nrg.2016.88.
Clark AT. DNA methylation remodeling in vitro and in vivo. Curr Opin Genet Dev. 2015;34:82–7. https://doi.org/10.1016/j.gde.2015.09.002.
Satoh M. Histogenesis and organogenesis of the gonad in human embryos. J Anat. 1991;177:85–107.
Liu C, Peng J, Matzuk MM, Yao HH. Lineage specification of ovarian theca cells requires multicellular interactions via oocyte and granulosa cells. Nat Commun. 2015;6:6934. https://doi.org/10.1038/ncomms7934.
Karl J, Capel B. Sertoli cells of the mouse testis originate from the coelomic epithelium. Dev Biol. 1998;203(2):323–33. https://doi.org/10.1006/dbio.1998.9068.
Hu YC, Okumura LM, Page DC. Gata4 is required for formation of the genital ridge in mice. PLoS Genet. 2013;9(7):e1003629. https://doi.org/10.1371/journal.pgen.1003629.
Miyamoto N, Yoshida M, Kuratani S, Matsuo I, Aizawa S. Defects of urogenital development in mice lacking Emx2. Development. 1997;124(9):1653–64.
Birk OS, Casiano DE, Wassif CA, Cogliati T, Zhao L, Zhao Y, Grinberg A, Huang S, Kreidberg JA, Parker KL, Porter FD, Westphal H. The LIM homeobox gene Lhx9 is essential for mouse gonad formation. Nature. 2000;403(6772):909–13. https://doi.org/10.1038/35002622.
Kreidberg JA, Sariola H, Loring JM, Maeda M, Pelletier J, Housman D, Jaenisch R. WT-1 is required for early kidney development. Cell. 1993;74(4):679–91.
Eggers S, Ohnesorg T, Sinclair A. Genetic regulation of mammalian gonad development. Nat Rev Endocrinol. 2014;10(11):673–83. https://doi.org/10.1038/nrendo.2014.163.
Hastie ND. Wilms’ tumour 1 (WT1) in development, homeostasis and disease. Development. 2017;144(16):2862–72. https://doi.org/10.1242/dev.153163.
Topol L, Chen W, Song H, Day TF, Yang Y. Sox9 inhibits Wnt signaling by promoting beta-catenin phosphorylation in the nucleus. J Biol Chem. 2009;284(5):3323–33. https://doi.org/10.1074/jbc.M808048200.
Lin YT, Capel B. Cell fate commitment during mammalian sex determination. Curr Opin Genet Dev. 2015;32:144–52. https://doi.org/10.1016/j.gde.2015.03.003.
Hughes JF, Page DC. The biology and evolution of mammalian Y chromosomes. Annu Rev Genet. 2015;49:507–27. https://doi.org/10.1146/annurev-genet-112414-055311.
Koopman P. The curious world of gonadal development in mammals. Curr Top Dev Biol. 2016;116:537–45. https://doi.org/10.1016/bs.ctdb.2015.12.009.
Sekido R, Lovell-Badge R. Sex determination and SRY: down to a wink and a nudge? Trends Genet. 2009;25(1):19–29. https://doi.org/10.1016/j.tig.2008.10.008.
Spiller C, Koopman P, Bowles J. Sex determination in the mammalian germline. Annu Rev Genet. 2017;51:265–85. https://doi.org/10.1146/annurev-genet-120215-035449.
Kurilo LF. Oogenesis in antenatal development in man. Hum Genet. 1981;57(1):86–92.
Kashimada K, Svingen T, Feng CW, Pelosi E, Bagheri-Fam S, Harley VR, Schlessinger D, Bowles J, Koopman P. Antagonistic regulation of Cyp26b1 by transcription factors SOX9/SF1 and FOXL2 during gonadal development in mice. FASEB J. 2011;25(10):3561–9. https://doi.org/10.1096/fj.11-184333.
Crisponi L, Deiana M, Loi A, Chiappe F, Uda M, Amati P, Bisceglia L, Zelante L, Nagaraja R, Porcu S, Ristaldi MS, Marzella R, Rocchi M, Nicolino M, Lienhardt-Roussie A, Nivelon A, Verloes A, Schlessinger D, Gasparini P, Bonneau D, Cao A, Pilia G. The putative forkhead transcription factor FOXL2 is mutated in blepharophimosis/ptosis/epicanthus inversus syndrome. Nat Genet. 2001;27(2):159–66. https://doi.org/10.1038/84781.
Schmidt D, Ovitt CE, Anlag K, Fehsenfeld S, Gredsted L, Treier AC, Treier M. The murine winged-helix transcription factor Foxl2 is required for granulosa cell differentiation and ovary maintenance. Development. 2004;131(4):933–42. https://doi.org/10.1242/dev.00969.
Mork L, Maatouk DM, McMahon JA, Guo JJ, Zhang P, McMahon AP, Capel B. Temporal differences in granulosa cell specification in the ovary reflect distinct follicle fates in mice. Biol Reprod. 2012;86(2):37. https://doi.org/10.1095/biolreprod.111.095208.
Al-Agha OM, Huwait HF, Chow C, Yang W, Senz J, Kalloger SE, Huntsman DG, Young RH, Gilks CB. FOXL2 is a sensitive and specific marker for sex cord-stromal tumors of the ovary. Am J Surg Pathol. 2011;35(4):484–94. https://doi.org/10.1097/PAS.0b013e31820a406c.
Uda M, Ottolenghi C, Crisponi L, Garcia JE, Deiana M, Kimber W, Forabosco A, Cao A, Schlessinger D, Pilia G. Foxl2 disruption causes mouse ovarian failure by pervasive blockage of follicle development. Hum Mol Genet. 2004;13(11):1171–81. https://doi.org/10.1093/hmg/ddh124.
Ottolenghi C, Omari S, Garcia-Ortiz JE, Uda M, Crisponi L, Forabosco A, Pilia G, Schlessinger D. Foxl2 is required for commitment to ovary differentiation. Hum Mol Genet. 2005;14(14):2053–62. https://doi.org/10.1093/hmg/ddi210.
Uhlenhaut NH, Jakob S, Anlag K, Eisenberger T, Sekido R, Kress J, Treier AC, Klugmann C, Klasen C, Holter NI, Riethmacher D, Schutz G, Cooney AJ, Lovell-Badge R, Treier M. Somatic sex reprogramming of adult ovaries to testes by FOXL2 ablation. Cell. 2009;139(6):1130–42. https://doi.org/10.1016/j.cell.2009.11.021.
Shah SP, Kobel M, Senz J, Morin RD, Clarke BA, Wiegand KC, Leung G, Zayed A, Mehl E, Kalloger SE, Sun M, Giuliany R, Yorida E, Jones S, Varhol R, Swenerton KD, Miller D, Clement PB, Crane C, Madore J, Provencher D, Leung P, DeFazio A, Khattra J, Turashvili G, Zhao Y, Zeng T, Glover JN, Vanderhyden B, Zhao C, Parkinson CA, Jimenez-Linan M, Bowtell DD, Mes-Masson AM, Brenton JD, Aparicio SA, Boyd N, Hirst M, Gilks CB, Marra M, Huntsman DG. Mutation of FOXL2 in granulosa-cell tumors of the ovary. N Engl J Med. 2009;360(26):2719–29. https://doi.org/10.1056/NEJMoa0902542.
Buza N, Wong S, Hui P. FOXL2 mutation analysis of ovarian sex cord-stromal tumors: genotype-phenotype correlation with diagnostic considerations. Int J Gynecol Pathol. 2018;37(4):305–15. https://doi.org/10.1097/PGP.0000000000000426.
Sullivan SD, Castrillon DH. Insights into primary ovarian insufficiency through genetically engineered mouse models. Semin Reprod Med. 2011;29(4):283–98. https://doi.org/10.1055/s-0031-1280914.
Greenbaum MP, Yan W, Wu MH, Lin YN, Agno JE, Sharma M, Braun RE, Rajkovic A, Matzuk MM. TEX14 is essential for intercellular bridges and fertility in male mice. Proc Natl Acad Sci U S A. 2006;103(13):4982–7. https://doi.org/10.1073/pnas.0505123103.
Lei L, Spradling AC. Mouse oocytes differentiate through organelle enrichment from sister cyst germ cells. Science. 2016;352(6281):95–9. https://doi.org/10.1126/science.aad2156.
Konishi I, Fujii S, Okamura H, Parmley T, Mori T. Development of interstitial cells and ovigerous cords in the human fetal ovary: an ultrastructural study. J Anat. 1986;148:121–35.
Sforza C, Vizzotto L, Ferrario VF, Forabosco A. Position of follicles in normal human ovary during definitive histogenesis. Early Hum Dev. 2003;74(1):27–35.
Pepling ME. Follicular assembly: mechanisms of action. Reproduction. 2012;143(2):139–49. https://doi.org/10.1530/REP-11-0299.
Saatcioglu HD, Cuevas I, Castrillon DH. Control of oocyte reawakening by Kit. PLoS Genet. 2016;12(8):e1006215. https://doi.org/10.1371/journal.pgen.1006215.
Baker TG. A quantitative and cytological study of germ cells in human ovaries. Proc R Soc Lond B Biol Sci. 1963;158:417–33.
Tilly JL. Commuting the death sentence: how oocytes strive to survive. Nat Rev Mol Cell Biol. 2001;2(11):838–48. https://doi.org/10.1038/35099086.
Qin Y, Jiao X, Simpson JL, Chen ZJ. Genetics of primary ovarian insufficiency: new developments and opportunities. Hum Reprod Update. 2015;21(6):787–808. https://doi.org/10.1093/humupd/dmv036.
Hansen KR, Knowlton NS, Thyer AC, Charleston JS, Soules MR, Klein NA. A new model of reproductive aging: the decline in ovarian non-growing follicle number from birth to menopause. Hum Reprod. 2008;23(3):699–708. https://doi.org/10.1093/humrep/dem408.
Livera G, Petre-Lazar B, Guerquin MJ, Trautmann E, Coffigny H, Habert R. p63 null mutation protects mouse oocytes from radio-induced apoptosis. Reproduction. 2008;135(1):3–12. https://doi.org/10.1530/REP-07-0054.
Hutt KJ. The role of BH3-only proteins in apoptosis within the ovary. Reproduction. 2015;149(2):R81–9. https://doi.org/10.1530/REP-14-0422.
Rafique S, Sterling EW, Nelson LM. A new approach to primary ovarian insufficiency. Obstet Gynecol Clin North Am. 2012;39(4):567–86. https://doi.org/10.1016/j.ogc.2012.09.007.
McGee EA, Hsueh AJ. Initial and cyclic recruitment of ovarian follicles. Endocr Rev. 2000;21(2):200–14. https://doi.org/10.1210/edrv.21.2.0394.
Peters H, Byskov AG, Himelstein-Braw R, Faber M. Follicular growth: the basic event in the mouse and human ovary. J Reprod Fertil. 1975;45(3):559–66.
Eppig JJ, O’Brien M, Wigglesworth K. Mammalian oocyte growth and development in vitro. Mol Reprod Dev. 1996;44(2):260–73. https://doi.org/10.1002/(SICI)1098-2795(199606)44:2<260::AID-MRD17>3.0.CO;2-6.
Peters H, Byskov AG, Lintern-Moore S, Faber M, Andersen M. The effect of gonadotrophin on follicle growth initiation in the neonatal mouse ovary. J Reprod Fertil. 1973;35(1):139–41.
Castrillon DH, Miao L, Kollipara R, Horner JW, DePinho RA. Suppression of ovarian follicle activation in mice by the transcription factor Foxo3a. Science. 2003;301(5630):215–8. https://doi.org/10.1126/science.1086336.
John GB, Shirley LJ, Gallardo TD, Castrillon DH. Specificity of the requirement for Foxo3 in primordial follicle activation. Reproduction. 2007;133(5):855–63. https://doi.org/10.1530/REP-06-0051.
John GB, Gallardo TD, Shirley LJ, Castrillon DH. Foxo3 is a PI3K-dependent molecular switch controlling the initiation of oocyte growth. Dev Biol. 2008;321(1):197–204. https://doi.org/10.1016/j.ydbio.2008.06.017.
Reddy P, Liu L, Adhikari D, Jagarlamudi K, Rajareddy S, Shen Y, Du C, Tang W, Hamalainen T, Peng SL, Lan ZJ, Cooney AJ, Huhtaniemi I, Liu K. Oocyte-specific deletion of Pten causes premature activation of the primordial follicle pool. Science. 2008;319(5863):611–3. https://doi.org/10.1126/science.1152257.
Tarnawa ED, Baker MD, Aloisio GM, Carr BR, Castrillon DH. Gonadal expression of Foxo1, but not Foxo3, is conserved in diverse Mammalian species. Biol Reprod. 2013;88(4):103. https://doi.org/10.1095/biolreprod.112.105791.
Cancer Genome Atlas Research N, Kandoth C, Schultz N, Cherniack AD, Akbani R, Liu Y, Shen H, Robertson AG, Pashtan I, Shen R, Benz CC, Yau C, Laird PW, Ding L, Zhang W, Mills GB, Kucherlapati R, Mardis ER, Levine DA. Integrated genomic characterization of endometrial carcinoma. Nature. 2013;497(7447):67–73. https://doi.org/10.1038/nature12113.
Müller JP. Bildungsgeschichte der Genitalien, vol. xviii, 152 p. Düsseldorf: Arnz; 1830.
Adelmann HB, editor. Marcello Malpighi and the evolution of embryology, Cornell publications in the history of science, vol. 4. Ithaca: Cornell University Press; 1966. p. 1851–901
Hashimoto R. Development of the human Mullerian duct in the sexually undifferentiated stage. Anat Rec A Discov Mol Cell Evol Biol. 2003;272(2):514–9. https://doi.org/10.1002/ar.a.10061.
Vigier B, Picard JY, Bezard J, Josso N. Anti-Mullerian hormone: a local or long-distance morphogenetic factor? Hum Genet. 1981;58(1):85–90.
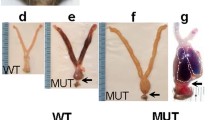
Mullen RD, Behringer RR. Molecular genetics of Mullerian duct formation, regression and differentiation. Sex Dev. 2014;8(5):281–96. https://doi.org/10.1159/000364935.
Josso N, di Clemente N, Gouedard L. Anti-Mullerian hormone and its receptors. Mol Cell Endocrinol. 2001;179(1–2):25–32.
Klattig J, Englert C. The Mullerian duct: recent insights into its development and regression. Sex Dev. 2007;1(5):271–8. https://doi.org/10.1159/000108929.
Zhao F, Franco HL, Rodriguez KF, Brown PR, Tsai MJ, Tsai SY, Yao HH. Elimination of the male reproductive tract in the female embryo is promoted by COUP-TFII in mice. Science. 2017;357(6352):717–20. https://doi.org/10.1126/science.aai9136.
Jacquinet A, Millar D, Lehman A. Etiologies of uterine malformations. Am J Med Genet A. 2016;170(8):2141–72. https://doi.org/10.1002/ajmg.a.37775.
Gruenwald P. The relation of the growing müllerian duct to the wolffian duct and its importance for the genesis of malformations. Anat Rec. 1941;81:1–19.
Kobayashi A, Shawlot W, Kania A, Behringer RR. Requirement of Lim1 for female reproductive tract development. Development. 2004;131(3):539–49. https://doi.org/10.1242/dev.00951.
Torres M, Gomez-Pardo E, Dressler GR, Gruss P. Pax-2 controls multiple steps of urogenital development. Development. 1995;121(12):4057–65.
Robboy SJ, Kurita T, Baskin L, Cunha GR. New insights into human female reproductive tract development. Differentiation. 2017;97:9–22. https://doi.org/10.1016/j.diff.2017.08.002.
Huang CC, Orvis GD, Kwan KM, Behringer RR. Lhx1 is required in Mullerian duct epithelium for uterine development. Dev Biol. 2014;389(2):124–36. https://doi.org/10.1016/j.ydbio.2014.01.025.
Vainio S, Heikkila M, Kispert A, Chin N, McMahon AP. Female development in mammals is regulated by Wnt-4 signalling. Nature. 1999;397(6718):405–9. https://doi.org/10.1038/17068.
Prunskaite-Hyyrylainen R, Skovorodkin I, Xu Q, Miinalainen I, Shan J, Vainio SJ. Wnt4 coordinates directional cell migration and extension of the Mullerian duct essential for ontogenesis of the female reproductive tract. Hum Mol Genet. 2016;25(6):1059–73. https://doi.org/10.1093/hmg/ddv621.
Kurita T. Developmental origin of vaginal epithelium. Differentiation. 2010;80(2–3):99–105. https://doi.org/10.1016/j.diff.2010.06.007.
Fujino A, Arango NA, Zhan Y, Manganaro TF, Li X, MacLaughlin DT, Donahoe PK. Cell migration and activated PI3K/AKT-directed elongation in the developing rat Mullerian duct. Dev Biol. 2009;325(2):351–62. https://doi.org/10.1016/j.ydbio.2008.10.027.
Devouassoux-Shisheboran M, Silver SA, Tavassoli FA. Wolffian adnexal tumor, so-called female adnexal tumor of probable Wolffian origin (FATWO): immunohistochemical evidence in support of a Wolffian origin. Hum Pathol. 1999;30(7):856–63.
Labastie MC, Catala M, Gregoire JM, Peault B. The GATA-3 gene is expressed during human kidney embryogenesis. Kidney Int. 1995;47(6):1597–603.
Grote D, Souabni A, Busslinger M, Bouchard M. Pax 2/8-regulated Gata 3 expression is necessary for morphogenesis and guidance of the nephric duct in the developing kidney. Development. 2006;133(1):53–61. https://doi.org/10.1242/dev.02184.
Howitt BE, Emori MM, Drapkin R, Gaspar C, Barletta JA, Nucci MR, McCluggage WG, Oliva E, Hirsch MS. GATA3 is a sensitive and specific marker of benign and malignant Mesonephric lesions in the lower female genital tract. Am J Surg Pathol. 2015;39(10):1411–9. https://doi.org/10.1097/PAS.0000000000000471.
Atsuta Y, Takahashi Y. Early formation of the Mullerian duct is regulated by sequential actions of BMP/Pax2 and FGF/Lim1 signaling. Development. 2016;143(19):3549–59. https://doi.org/10.1242/dev.137067.
Mittag J, Winterhager E, Bauer K, Grummer R. Congenital hypothyroid female pax8-deficient mice are infertile despite thyroid hormone replacement therapy. Endocrinology. 2007;148(2):719–25. https://doi.org/10.1210/en.2006-1054.
Batista MF, Lewis KE. Pax2/8 act redundantly to specify glycinergic and GABAergic fates of multiple spinal interneurons. Dev Biol. 2008;323(1):88–97. https://doi.org/10.1016/j.ydbio.2008.08.009.
Bouchard M, de Caprona D, Busslinger M, Xu P, Fritzsch B. Pax2 and Pax8 cooperate in mouse inner ear morphogenesis and innervation. BMC Dev Biol. 2010;10:89. https://doi.org/10.1186/1471-213X-10-89.
Klattig J, Sierig R, Kruspe D, Besenbeck B, Englert C. Wilms’ tumor protein Wt1 is an activator of the anti-Mullerian hormone receptor gene Amhr2. Mol Cell Biol. 2007;27(12):4355–64. https://doi.org/10.1128/MCB.01780-06.
Armstrong JF, Pritchard-Jones K, Bickmore WA, Hastie ND, Bard JB. The expression of the Wilms’ tumour gene, WT1, in the developing mammalian embryo. Mech Dev. 1993;40(1–2):85–97.
Parenti R, Perris R, Vecchio GM, Salvatorelli L, Torrisi A, Gravina L, Magro G. Immunohistochemical expression of Wilms’ tumor protein (WT1) in developing human epithelial and mesenchymal tissues. Acta Histochem. 2013;115(1):70–5. https://doi.org/10.1016/j.acthis.2012.04.006.
Shimizu M, Toki T, Takagi Y, Konishi I, Fujii S. Immunohistochemical detection of the Wilms’ tumor gene (WT1) in epithelial ovarian tumors. Int J Gynecol Pathol. 2000;19(2):158–63.
Kommoss F, Faruqi A, Gilks CB, Lamshang Leen S, Singh N, Wilkinson N, McCluggage WG. Uterine serous carcinomas frequently metastasize to the fallopian tube and can mimic serous tubal intraepithelial carcinoma. Am J Surg Pathol. 2017;41(2):161–70. https://doi.org/10.1097/PAS.0000000000000757.
Nafisi H, Ghorab Z, Ismill N, Dube V, Plotkin A, Han G, Cesari M, Lu FI, Saad R, Khalifa M, Nofech-Mozes S. Immunophenotypic analysis in early Mullerian serous carcinogenesis. Int J Gynecol Pathol. 2015;34(5):424–36. https://doi.org/10.1097/PGP.0000000000000179.
Du H, Taylor HS. The role of Hox genes in female reproductive tract development, adult function, and fertility. Cold Spring Harb Perspect Med. 2015;6(1):a023002. https://doi.org/10.1101/cshperspect.a023002.
Taylor HS, Vanden Heuvel GB, Igarashi P. A conserved Hox axis in the mouse and human female reproductive system: late establishment and persistent adult expression of the Hoxa cluster genes. Biol Reprod. 1997;57(6):1338–45.
Warot X, Fromental-Ramain C, Fraulob V, Chambon P, Dolle P. Gene dosage-dependent effects of the Hoxa-13 and Hoxd-13 mutations on morphogenesis of the terminal parts of the digestive and urogenital tracts. Development. 1997;124(23):4781–91.
Yang A, Schweitzer R, Sun D, Kaghad M, Walker N, Bronson RT, Tabin C, Sharpe A, Caput D, Crum C, McKeon F. p63 is essential for regenerative proliferation in limb, craniofacial and epithelial development. Nature. 1999;398(6729):714–8. https://doi.org/10.1038/19539.
Ince TA, Cviko AP, Quade BJ, Yang A, McKeon FD, Mutter GL, Crum CP. p63 Coordinates anogenital modeling and epithelial cell differentiation in the developing female urogenital tract. Am J Pathol. 2002;161(4):1111–7. https://doi.org/10.1016/S0002-9440(10)64387-8.
Crum CP, McKeon FD. p63 in epithelial survival, germ cell surveillance, and neoplasia. Annu Rev Pathol. 2010;5:349–71. https://doi.org/10.1146/annurev-pathol-121808-102117.
Kurita T, Mills AA, Cunha GR. Roles of p63 in the diethylstilbestrol-induced cervicovaginal adenosis. Development. 2004;131(7):1639–49. https://doi.org/10.1242/dev.01038.
Laronda MM, Unno K, Ishi K, Serna VA, Butler LM, Mills AA, Orvis GD, Behringer RR, Deng C, Sinha S, Kurita T. Diethylstilbestrol induces vaginal adenosis by disrupting SMAD/RUNX1-mediated cell fate decision in the Mullerian duct epithelium. Dev Biol. 2013;381(1):5–16. https://doi.org/10.1016/j.ydbio.2013.06.024.
Terakawa J, Rocchi A, Serna VA, Bottinger EP, Graff JM, Kurita T. FGFR2IIIb-MAPK activity is required for epithelial cell fate decision in the lower Mullerian duct. Mol Endocrinol. 2016;30(7):783–95. https://doi.org/10.1210/me.2016-1027.
Cooke PS, Spencer TE, Bartol FF, Hayashi K. Uterine glands: development, function and experimental model systems. Mol Hum Reprod. 2013;19(9):547–58. https://doi.org/10.1093/molehr/gat031.
Valdes-Dapena MA. Uterine development in late Fetal life, infancy, and childhood. In: Norris HJ, Hertig AT, Abell MR, editors. The uterus. Monographs in pathology. Baltimore: Williams & Wilkins; 1973. p. 40–67.
Fluhmann CF. The developmental anatomy of the cervix uteri. Obstet Gynecol. 1960;15:62–9.
Ogasawara Y, Okamoto S, Kitamura Y, Matsumoto K. Proliferative pattern of uterine cells from birth to adulthood in intact, neonatally castrated, and/or adrenalectomized mice, assayed by incorporation of [125I]iododeoxyuridine. Endocrinology. 1983;113(2):582–7. https://doi.org/10.1210/endo-113-2-582.
Gray CA, Taylor KM, Ramsey WS, Hill JR, Bazer FW, Bartol FF, Spencer TE. Endometrial glands are required for preimplantation conceptus elongation and survival. Biol Reprod. 2001;64(6):1608–13.
Filant J, Spencer TE. Endometrial glands are essential for blastocyst implantation and decidualization in the mouse uterus. Biol Reprod. 2013;88(4):93. https://doi.org/10.1095/biolreprod.113.107631.
Cooke PS, Ekman GC, Kaur J, Davila J, Bagchi IC, Clark SG, Dziuk PJ, Hayashi K, Bartol FF. Brief exposure to progesterone during a critical neonatal window prevents uterine gland formation in mice. Biol Reprod. 2012;86(3):63. https://doi.org/10.1095/biolreprod.111.097188.
Friedman JR, Kaestner KH. The Foxa family of transcription factors in development and metabolism. Cell Mol Life Sci. 2006;63(19–20):2317–28. https://doi.org/10.1007/s00018-006-6095-6.
Dunlap KA, Filant J, Hayashi K, Rucker EB 3rd, Song G, Deng JM, Behringer RR, DeMayo FJ, Lydon J, Jeong JW, Spencer TE. Postnatal deletion of Wnt7a inhibits uterine gland morphogenesis and compromises adult fertility in mice. Biol Reprod. 2011;85(2):386–96. https://doi.org/10.1095/biolreprod.111.091769.
Kelleher AM, Peng W, Pru JK, Pru CA, DeMayo FJ, Spencer TE. Forkhead box a2 (FOXA2) is essential for uterine function and fertility. Proc Natl Acad Sci U S A. 2017;114(6):E1018–26. https://doi.org/10.1073/pnas.1618433114.
Parr BA, McMahon AP. Sexually dimorphic development of the mammalian reproductive tract requires Wnt-7a. Nature. 1998;395(6703):707–10. https://doi.org/10.1038/27221.
Miller C, Sassoon DA. Wnt-7a maintains appropriate uterine patterning during the development of the mouse female reproductive tract. Development. 1998;125(16):3201–11.
Hayashi K, Yoshioka S, Reardon SN, Rucker EB 3rd, Spencer TE, DeMayo FJ, Lydon JP, MacLean JA 2nd. WNTs in the neonatal mouse uterus: potential regulation of endometrial gland development. Biol Reprod. 2011;84(2):308–19. https://doi.org/10.1095/biolreprod.110.088161.
Franco HL, Dai D, Lee KY, Rubel CA, Roop D, Boerboom D, Jeong JW, Lydon JP, Bagchi IC, Bagchi MK, DeMayo FJ. WNT4 is a key regulator of normal postnatal uterine development and progesterone signaling during embryo implantation and decidualization in the mouse. FASEB J. 2011;25(4):1176–87. https://doi.org/10.1096/fj.10-175349.
Wang Y, Chang H, Rattner A, Nathans J. Frizzled receptors in development and disease. Curr Top Dev Biol. 2016;117:113–39. https://doi.org/10.1016/bs.ctdb.2015.11.028.
MacDonald BT, Tamai K, He X. Wnt/beta-catenin signaling: components, mechanisms, and diseases. Dev Cell. 2009;17(1):9–26. https://doi.org/10.1016/j.devcel.2009.06.016.
Stewart CA, Wang Y, Bonilla-Claudio M, Martin JF, Gonzalez G, Taketo MM, Behringer RR. CTNNB1 in mesenchyme regulates epithelial cell differentiation during Mullerian duct and postnatal uterine development. Mol Endocrinol. 2013;27(9):1442–54. https://doi.org/10.1210/me.2012-1126.
Jeong JW, Lee HS, Franco HL, Broaddus RR, Taketo MM, Tsai SY, Lydon JP, DeMayo FJ. beta-catenin mediates glandular formation and dysregulation of beta-catenin induces hyperplasia formation in the murine uterus. Oncogene. 2009;28(1):31–40. https://doi.org/10.1038/onc.2008.363.
Saegusa M, Okayasu I. Frequent nuclear beta-catenin accumulation and associated mutations in endometrioid-type endometrial and ovarian carcinomas with squamous differentiation. J Pathol. 2001;194(1):59–67. https://doi.org/10.1002/path.856.
Abbott JA. Adenomyosis and abnormal uterine bleeding (AUB-A)-pathogenesis, diagnosis, and management. Best Pract Res Clin Obstet Gynaecol. 2017;40:68–81. https://doi.org/10.1016/j.bpobgyn.2016.09.006.
Oh SJ, Shin JH, Kim TH, Lee HS, Yoo JY, Ahn JY, Broaddus RR, Taketo MM, Lydon JP, Leach RE, Lessey BA, Fazleabas AT, Lim JM, Jeong JW. beta-Catenin activation contributes to the pathogenesis of adenomyosis through epithelial-mesenchymal transition. J Pathol. 2013;231(2):210–22. https://doi.org/10.1002/path.4224.
Gun I, Oner O, Bodur S, Ozdamar O, Atay V. Is adenomyosis associated with the risk of endometrial cancer? Med Glas (Zenica). 2012;9(2):268–72.
Vercellini P, Parazzini F, Oldani S, Panazza S, Bramante T, Crosignani PG. Adenomyosis at hysterectomy: a study on frequency distribution and patient characteristics. Hum Reprod. 1995;10(5):1160–2.
Orvis GD, Behringer RR. Cellular mechanisms of Mullerian duct formation in the mouse. Dev Biol. 2007;306(2):493–504. https://doi.org/10.1016/j.ydbio.2007.03.027.
Castrillon DH, Lee KR, Nucci MR. Distinction between endometrial and endocervical adenocarcinoma: an immunohistochemical study. Int J Gynecol Pathol. 2002;21(1):4–10.
Nucci MR, Castrillon DH, Bai H, Quade BJ, Ince TA, Genest DR, Lee KR, Mutter GL, Crum CP. Biomarkers in diagnostic obstetric and gynecologic pathology: a review. Adv Anat Pathol. 2003;10(2):55–68.
Allard S, Adin P, Gouedard L, di Clemente N, Josso N, Orgebin-Crist MC, Picard JY, Xavier F. Molecular mechanisms of hormone-mediated Mullerian duct regression: involvement of beta-catenin. Development. 2000;127(15):3349–60.
Huang CC, Orvis GD, Wang Y, Behringer RR. Stromal-to-epithelial transition during postpartum endometrial regeneration. PLoS One. 2012;7(8):e44285. https://doi.org/10.1371/journal.pone.0044285.
Cunha GR. Stromal induction and specification of morphogenesis and cytodifferentiation of the epithelia of the Mullerian ducts and urogenital sinus during development of the uterus and vagina in mice. J Exp Zool. 1976;196(3):361–70. https://doi.org/10.1002/jez.1401960310.
Chang AR. ‘Erosion’ of the uterine cervix; an anachronism. Aust N Z J Obstet Gynaecol. 1991;31(4):358–62.
Kobayashi A, Behringer RR. Developmental genetics of the female reproductive tract in mammals. Nat Rev Genet. 2003;4(12):969–80. https://doi.org/10.1038/nrg1225.
Cunha GR, Kurita T, Cao M, Shen J, Robboy S, Baskin L. Molecular mechanisms of development of the human fetal female reproductive tract. Differentiation. 2017;97:54–72. https://doi.org/10.1016/j.diff.2017.07.003.
Jesus LE, Camelier P, Bastos J, Tome AS, Dekermacher S. Clitoral abnormalities in the absence of virilization: etiology and treatment strategies. Urology. 2016;88:170–2. https://doi.org/10.1016/j.urology.2015.10.020.
Griebel ML, Redman JF, Kemp SF, Elders MJ. Hypertrophy of clitoral hood: presenting sign of neurofibromatosis in female child. Urology. 1991;37(4):337–9.
Sutphen R, Galan-Gomez E, Kousseff BG. Clitoromegaly in neurofibromatosis. Am J Med Genet. 1995;55(3):325–30. https://doi.org/10.1002/ajmg.1320550316.
Rouzi AA, Sindi O, Radhan B, Ba’aqeel H. Epidermal clitoral inclusion cyst after type I female genital mutilation. Am J Obstet Gynecol. 2001;185(3):569–71. https://doi.org/10.1067/mob.2001.117660.
Hughes JW, Guess MK, Hittelman A, Yip S, Astle J, Pal L, Inzucchi SE, Dulay AT. Clitoral epidermoid cyst presenting as pseudoclitoromegaly of pregnancy. AJP Rep. 2013;3(1):57–62. https://doi.org/10.1055/s-0033-1334461.
Williams CE, Nakhal RS, Achermann JC, Creighton SM. Persistent unexplained congenital clitoromegaly in females born extremely prematurely. J Pediatr Urol. 2013;9(6 Pt A):962–5. https://doi.org/10.1016/j.jpurol.2013.03.001.
Mayoglou L, Dulabon L, Martin-Alguacil N, Pfaff D, Schober J. Success of treatment modalities for labial fusion: a retrospective evaluation of topical and surgical treatments. J Pediatr Adolesc Gynecol. 2009;22(4):247–50. https://doi.org/10.1016/j.jpag.2008.09.003.
Ziglioli F, Fornia S, Ciuffireda M, Meli S, Dinale F, Simonazzi M, Cortellini P. Lichen sclerosus: a review of literature and a case of an atypic surgical treatment. Acta Biomed. 2011;82(1):51–7.
Dietrich JE, Millar DM, Quint EH. Obstructive reproductive tract anomalies. J Pediatr Adolesc Gynecol. 2014;27(6):396–402. https://doi.org/10.1016/j.jpag.2014.09.001.
Olive DL, Henderson DY. Endometriosis and mullerian anomalies. Obstet Gynecol. 1987;69(3 Pt 1):412–5.
Loscalzo IL, Catapano M, Loscalzo J, Sama A. Imperforate hymen with bilateral hydronephrosis: an unusual emergency department diagnosis. J Emerg Med. 1995;13(3):337–9.
Iwasa Y, Fletcher CD. Distinctive prepubertal vulval fibroma: a hitherto unrecognized mesenchymal tumor of prepubertal girls: analysis of 11 cases. Am J Surg Pathol. 2004;28(12):1601–8.
Vargas SO, Kozakewich HP, Boyd TK, Ecklund K, Fishman SJ, Laufer MR, Perez-Atayde AR. Childhood asymmetric labium majus enlargement: mimicking a neoplasm. Am J Surg Pathol. 2005;29(8):1007–16.
Khunda S, Nakash A. Double vulva. J Obstet Gynaecol. 1999;19(1):94–5. https://doi.org/10.1080/01443619966155.
Bellemare S, Dibden L. Absence of the clitoris in a 13-year-old adolescent: medical implications for child and adolescent health. J Pediatr Adolesc Gynecol. 2005;18(6):415–8. https://doi.org/10.1016/j.jpag.2005.09.011.
Ruggeri G, Gargano T, Antonellini C, Carlini V, Randi B, Destro F, Lima M. Vaginal malformations: a proposed classification based on embryological, anatomical and clinical criteria and their surgical management (an analysis of 167 cases). Pediatr Surg Int. 2012;28(8):797–803. https://doi.org/10.1007/s00383-012-3121-7.
Wang J, Ezzat W, Davidson M. Transverse vaginal septum. A case report. J Reprod Med. 1995;40(2):163–6.
Rana A, Manandhar B, Amatya A, Baral J, Gurung G, Giri A, Giri K. Mucocolpos due to complete transverse septum in middle third of vagina in a 17-year-old girl. J Obstet Gynaecol Res. 2002;28(2):86–8.
Pena A. Cloaca—historical aspects and terminology. Semin Pediatr Surg. 2016;25(2):62–5. https://doi.org/10.1053/j.sempedsurg.2015.11.002.
Gupta A, Bischoff A, Pena A, Runck LA, Guasch G. The great divide: septation and malformation of the cloaca, and its implications for surgeons. Pediatr Surg Int. 2014;30(11):1089–95. https://doi.org/10.1007/s00383-014-3593-8.
Chan YY, Jayaprakasan K, Zamora J, Thornton JG, Raine-Fenning N, Coomarasamy A. The prevalence of congenital uterine anomalies in unselected and high-risk populations: a systematic review. Hum Reprod Update. 2011;17(6):761–71. https://doi.org/10.1093/humupd/dmr028.
Hammoud AO, Gibson M, Peterson CM, Kerber RA, Mineau GP, Hatasaka H. Quantification of the familial contribution to mullerian anomalies. Obstet Gynecol. 2008;111(2 Pt 1):378–84. https://doi.org/10.1097/01.AOG.0000267219.10869.9f.
Duru UA, Laufer MR. Discordance in Mayer-von Rokitansky-Kuster-Hauser syndrome noted in monozygotic twins. J Pediatr Adolesc Gynecol. 2009;22(4):e73–5. https://doi.org/10.1016/j.jpag.2008.07.012.
Grimbizis GF, Gordts S, Di Spiezio Sardo A, Brucker S, De Angelis C, Gergolet M, Li TC, Tanos V, Brolmann H, Gianaroli L, Campo R. The ESHRE-ESGE consensus on the classification of female genital tract congenital anomalies. Gynecol Surg. 2013;10(3):199–212. https://doi.org/10.1007/s10397-013-0800-x.
Ludwin A, Martins WP, Nastri CO, Ludwin I, Coelho Neto MA, Leitao VM, Acien M, Alcazar JL, Benacerraf B, Condous G, De Wilde RL, Emanuel MH, Gibbons W, Guerriero S, Hurd WW, Levine D, Lindheim S, Pellicer A, Petraglia F, Saridogan E. Congenital Uterine Malformation by Experts (CUME): better criteria for distinguishing between normal/arcuate and septate uterus? Ultrasound Obstet Gynecol. 2018;51(1):101–9. https://doi.org/10.1002/uog.18923.
Ludwin A, Ludwin I, Kudla M, Kottner J. Reliability of the European Society of Human Reproduction and Embryology/European Society for Gynaecological Endoscopy and American Society for Reproductive Medicine classification systems for congenital uterine anomalies detected using three-dimensional ultrasonography. Fertil Steril. 2015;104(3):688–97 e688. https://doi.org/10.1016/j.fertnstert.2015.06.019.
Kives S. Müllerian anomaly classification systems. In: Pfeifer SM, editor. Congenital Müllerian anomalies: diagnosis and management. Cham: Springer International Publishing; 2016. p. 3–12. https://doi.org/10.1007/978-3-319-27231-3_1.
Bombard DS 2nd, Mousa SA. Mayer-Rokitansky-Kuster-Hauser syndrome: complications, diagnosis and possible treatment options: a review. Gynecol Endocrinol. 2014;30(9):618–23. https://doi.org/10.3109/09513590.2014.927855.
Prior M, Richardson A, Asif S, Polanski L, Parris-Larkin M, Chandler J, Fogg L, Jassal P, Thornton JG, Raine-Fenning NJ. Outcome of assisted reproduction in women with congenital uterine anomalies: a prospective observational study. Ultrasound Obstet Gynecol. 2018;51(1):110–7. https://doi.org/10.1002/uog.18935.
Kaufman Y, Lam A. The pelvic uterus-like mass--a primary or secondary Mullerian system anomaly? J Minim Invasive Gynecol. 2008;15(4):494–7. https://doi.org/10.1016/j.jmig.2008.03.002.
Cozzutto C. Uterus-like mass replacing ovary: report of a new entity. Arch Pathol Lab Med. 1981;105(10):508–11.
Sopha SC, Rosado FG, Smith JJ, Merchant NB, Shi C. Hepatic uterus-like mass misdiagnosed as hepatic abscess. Int J Surg Pathol. 2015;23(2):134–9. https://doi.org/10.1177/1066896914534465.
Gonzalez RS, Vnencak-Jones CL, Shi C, Fadare O. Endomyometriosis (“uterus-like mass”) in an XY male: case report with molecular confirmation and literature review. Int J Surg Pathol. 2014;22(5):421–6. https://doi.org/10.1177/1066896913501385.
Kakkar A, Sharma MC, Garg A, Goyal N, Suri V, Sarkar C, Mahapatra AK. Uterus-like mass in association with neural tube defect: a case report and review of the literature. Pediatr Neurosurg. 2012;48(4):240–4. https://doi.org/10.1159/000348811.
Rahilly MA, al-Nafussi A. Uterus-like mass of the ovary associated with endometrioid carcinoma. Histopathology. 1991;18(6):549–51.
Nakakita B, Abiko K, Mikami Y, Kido A, Baba T, Yoshioka Y, Yamaguchi K, Matsumura N, Konishi I. Clear cell carcinoma arising from a uterus-like mass. Pathol Int. 2014;64(11):576–80. https://doi.org/10.1111/pin.12218.
Seki A, Maeshima A, Nakagawa H, Shiraishi J, Murata Y, Arai H, Kubochi K, Kuramochi S. A subserosal uterus-like mass presenting after a sliding hernia of the ovary and endometriosis: a rare entity with a discussion of the histogenesis. Fertil Steril. 2011;95(5):1788 e1715–89. https://doi.org/10.1016/j.fertnstert.2010.11.051.
Mortlock DP, Innis JW. Mutation of HOXA13 in hand-foot-genital syndrome. Nat Genet. 1997;15(2):179–80. https://doi.org/10.1038/ng0297-179.
Jorgensen EM, Ruman JI, Doherty L, Taylor HS. A novel mutation of HOXA13 in a family with hand-foot-genital syndrome and the role of polyalanine expansions in the spectrum of Mullerian fusion anomalies. Fertil Steril. 2010;94(4):1235–8. https://doi.org/10.1016/j.fertnstert.2009.05.057.
Cheng Z, Zhu Y, Su D, Wang J, Cheng L, Chen B, Wei Z, Zhou P, Wang B, Ma X, Cao Y. A novel mutation of HOXA10 in a Chinese woman with a Mullerian duct anomaly. Hum Reprod. 2011;26(11):3197–201. https://doi.org/10.1093/humrep/der290.
Liatsikos SA, Grimbizis GF, Georgiou I, Papadopoulos N, Lazaros L, Bontis JN, Tarlatzis BC. HOX A10 and HOX A11 mutation scan in congenital malformations of the female genital tract. Reprod Biomed Online. 2010;21(1):126–32. https://doi.org/10.1016/j.rbmo.2010.03.015.
Schinzel A. Phocomelia and additional anomalies in two sisters. Hum Genet. 1990;84(6):539–41.
Coffinier C, Barra J, Babinet C, Yaniv M. Expression of the vHNF1/HNF1beta homeoprotein gene during mouse organogenesis. Mech Dev. 1999;89(1–2):211–3.
Lokmane L, Heliot C, Garcia-Villalba P, Fabre M, Cereghini S. vHNF1 functions in distinct regulatory circuits to control ureteric bud branching and early nephrogenesis. Development. 2010;137(2):347–57. https://doi.org/10.1242/dev.042226.
Lim D, Ip PP, Cheung AN, Kiyokawa T, Oliva E. Immunohistochemical comparison of ovarian and uterine endometrioid carcinoma, endometrioid carcinoma with clear cell change, and clear cell carcinoma. Am J Surg Pathol. 2015;39(8):1061–9. https://doi.org/10.1097/PAS.0000000000000436.
Pabuccu E, Kahraman K, Taskin S, Atabekoglu C. Unilateral absence of fallopian tube and ovary in an infertile patient. Fertil Steril. 2011;96(1):e55–7. https://doi.org/10.1016/j.fertnstert.2011.04.027.
Rapisarda G, Pappalardo EM, Arancio A, La Greca M. Unilateral ovarian and fallopian tube agenesis. Arch Gynecol Obstet. 2009;280(5):849–50. https://doi.org/10.1007/s00404-009-1018-z.
Tanaka Y, Koyama S, Kobayashi M, Kubota S, Nakamura R, Isobe M, Shiki Y. Complex Mullerian malformation without any present classification: unilateral ovarian and tubal absence with an arcuate uterus. Asian J Endosc Surg. 2013;6(1):55–7. https://doi.org/10.1111/j.1758-5910.2012.00159.x.
Mylonas I, Hansch S, Markmann S, Bolz M, Friese K. Unilateral ovarian agenesis: report of three cases and review of the literature. Arch Gynecol Obstet. 2003;268(1):57–60. https://doi.org/10.1007/s00404-002-0451-z.
Gandhi KR, Siddiqui AU, Wabale RN, Daimi SR. The accessory fallopian tube: a rare anomaly. J Hum Reprod Sci. 2012;5(3):293–4. https://doi.org/10.4103/0974-1208.106344.
Rottenstreich M, Smorgick N, Pansky M, Vaknin Z. Isolated torsion of accessory fallopian tube in a young adolescent. J Pediatr Adolesc Gynecol. 2016;29(4):e57–8. https://doi.org/10.1016/j.jpag.2016.03.003.
Ucar MG, Ilhan TT, Gul A, Korkutan C, Celik C. Patient with three fallopian tubes at right adnexa. J Clin Diagn Res. 2017;11(2):QJ03–4. https://doi.org/10.7860/JCDR/2017/22713.9263.
Narayanan R, Rajeev MA. Duplication of the fallopian tube. J Hum Reprod Sci. 2008;1(1):35–6.
Liu Q, Liu HQ, Jiang YY, Sun XB. Is unilateral uterine adnexa absence a congenital developmental abnormality or posteriority? Summary of 39 cases and literature review. Arch Gynecol Obstet. 2013;288(3):555–61. https://doi.org/10.1007/s00404-013-2891-z.
Verkauf BS, Bernhisel MA. Ovarian maldescent. Fertil Steril. 1996;65(1):189–92.
Veurink M, Koster M, LT B. The history of DES, lessons to be learned. Pharm World Sci. 2005;27(3):139–43. https://doi.org/10.1007/s11096-005-3663-z.
Herbst AL, Ulfelder H, Poskanzer DC. Adenocarcinoma of the vagina. Association of maternal stilbestrol therapy with tumor appearance in young women. N Engl J Med. 1971;284(15):878–81. https://doi.org/10.1056/NEJM197104222841604.
Ma L, Benson GV, Lim H, Dey SK, Maas RL. Abdominal B (AbdB) Hoxa genes: regulation in adult uterus by estrogen and progesterone and repression in mullerian duct by the synthetic estrogen diethylstilbestrol (DES). Dev Biol. 1998;197(2):141–54. https://doi.org/10.1006/dbio.1998.8907.
Kaufman RH, Adam E, Binder GL, Gerthoffer E. Upper genital tract changes and pregnancy outcome in offspring exposed in utero to diethylstilbestrol. Am J Obstet Gynecol. 1980;137(3):299–308.
Goldberg JM, Falcone T. Effect of diethylstilbestrol on reproductive function. Fertil Steril. 1999;72(1):1–7.
Swan SH. Intrauterine exposure to diethylstilbestrol: long-term effects in humans. APMIS. 2000;108(12):793–804.
John GB, Shidler MJ, Besmer P, Castrillon DH. Kit signaling via PI3K promotes ovarian follicle maturation but is dispensable for primordial follicle activation. Dev Biol. 2009;331(2):292–9. https://doi.org/10.1016/j.ydbio.2009.05.546.
Clevers H. Wnt/beta-catenin signaling in development and disease. Cell. 2006;127(3):469–80. https://doi.org/10.1016/j.cell.2006.10.018.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Science Press & Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Castrillon, D.H. (2019). Development and Maldevelopment of the Female Reproductive System. In: Zheng, W., Fadare, O., Quick, C., Shen, D., Guo, D. (eds) Gynecologic and Obstetric Pathology, Volume 1. Springer, Singapore. https://doi.org/10.1007/978-981-13-3016-2_1
Download citation
DOI: https://doi.org/10.1007/978-981-13-3016-2_1
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-3015-5
Online ISBN: 978-981-13-3016-2
eBook Packages: MedicineMedicine (R0)