Abstract
Calcium phosphate materials have been advocated as useful implantable scaffolds for bone tissue engineering. We have reported that synthetic octacalcium phosphate (OCP) is capable of enhancing differentiation of hard tissue-forming cells including osteoblastic cells, osteoclast precursor cells, and odontoblastic cells. The differentiation of mesenchymal stem cells is promoted to form new bone in the presence of OCP with atelo-collagen in vivo condition. The stimulatory capacity of OCP to conduct new bone increases with the copresence of amorphous calcium phosphate (ACP). Physical and chemical analyses of the materials suggested that the bioactivity of such hydroxyapatite (HA) precursor phases is induced as a result of the progressive change of chemical property of these materials during the hydrolysis into HA under physiological environment. The composite materials composed of OCP and natural polymers are capable of repairing not only mineralized tissues but also non-mineralized tissue. The form of OCP-based materials and the tissue responses to the materials will be summarized.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
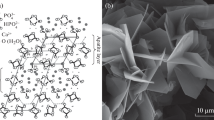
Calcium phosphate ceramics, such as sintered hydroxyapatite (HA, Ca10(PO4)6(OH)2) and β-tricalcium phosphate (β-TCP, β-Ca3(PO4)2), have widely been used as filling materials for various bone defects due to the superior osteoconductivity which is capable of bonding to bone tissue without intervention of connective tissues [1]. HA and β-TCP have been used as implantable scaffold materials with mesenchymal stem cells (MSCs) for bone regeneration [2]. These calcium phosphate materials provide suitable site where osteoblastic cells can attach, proliferate, and differentiate [2]. The physicochemical property of calcium phosphate materials affects the cellular responses to some extent [3, 4]. Octacalcium phosphate (OCP, Ca8H2(PO4)6·5H2O) is a non-sintered calcium phosphate material which was first proven to directly bond to bone tissue by onlaying it on mouse calvaria [5]. OCP has been regarded as a precursor phase in HA formation from supersaturated calcium and phosphate solutions with respect to HA and is therefore suggested to be a precursor to bone apatite crystals [6, 7] as well as amorphous calcium phosphate (ACP, Ca3(PO4)2·nH2O) [8]. OCP shows diversity regarding the stoichiometry [9] and the microstructure [10] depending on the preparation condition [11], which controls its bioactivity in vitro and in vivo [11]. This article summarizes the bioactivity of OCP and the composite materials with natural polymers as scaffold materials we have reported previously.
2 Mineralized and Non-mineralized Tissue Responses
OCP displays a unique osteoconductive property which tends to biodegrade and be followed by new bone formation if implanted in various bone defects, including the defects in intramembranous bone and long bones in various animal models [11, 12]. The efficacy of OCP has recently been reported by implanting its composite with collagen in human maxilla after cystectomy [13]. The stimulatory capacity of OCP could be induced by the environmental changes around the crystals, including calcium ion concentration change, due to the progressive hydrolysis from OCP to HA under physiological conditions [5, 14, 15]. The hydrolysis of OCP to HA is enhanced if ACP coexists with OCP, and the bone regenerative capacity of OCP is augmented by mechanically mixing OCP with ACP in rat critical-sized calvaria defect [16]. A composite of OCP with gelatin matrix, prepared through a wet synthesis, showed a greater biodegradable property coupled with a greater bone regenerative property if the material was implanted in rat critical-sized calvaria defect [17, 18]. The in vivo studies indicated that OCP/gelatin composite repairs not only rabbit tibia defect model [19] but also reforms infraspinatus tendon insertion using rabbit rotator cuff tear model [20].
3 Matrix Materials for Calcium Phosphate
Various calcium phosphate composites with natural polymers have been developed for bone and other tissue engineering (Table 10.1). Collagen (Col) is the major component of extracellular matrix proteins in bone, and its reconstituted Col has been utilized as matrix materials for calcium phosphates. HA/Col composites have been prepared by different processes, such as direct physical mixing [21, 22], chemical deposition of HA [23], or biomimetic mineralization [24]. Biodegradable calcium phosphates/Col composites, such as OCP/Col and β-TCP/Col, have also been obtained using coprecipitation methods [25, 26] and by physical mixing [27]. Gelatin (Gel) is a denatured form of collagen and has the advantage of higher biodegradability. HA/Gel composites have been obtained in various forms, not only in porous form but also in film and particle forms [28–31]. OCP/Gel composites have been prepared by physical mixing and coprecipitation [17, 18]. Other natural polymers, such as chitosan and silk fibroin, have also been combined with calcium phosphates [32–37].
Alginate (Alg) is a natural polysaccharide obtained from brown algae and applied for wound healing and drug delivery due to its biocompatibility. HA/Alg and β-TCP/Alg have been prepared as porous scaffolds or beads [38–41]. Our group has developed OCP/Alg porous scaffolds [42, 43]. Although it is known that Alg is not able to interact with mammalian cells [44], OCP/Alg was capable of enhancing osteoblastic cell attachment and bone formation depending on the pore size and the porosity of the composites [42]. OCP/Alg beads including osteoblastic cells have a potential to activate and deliver osteoblastic cells from the beads to the local sites of bone defects [45]. Hyaluronic acid (HyA) is a major component of the extracellular matrix in the connective tissue. HyA hydrogel can be used as injectable materials filling bone defects directly and has been reported to promote bone regeneration [46, 47]. OCP/HyA is a bone substitute material which was proven to show the injectable and bioactive properties [48].
4 Cell Responses to Calcium Phosphate Materials
We have reported that OCP induces osteoblastic differentiation of mouse stromal cells [15, 51]. When mouse ST2 cells were cultured on the OCP or HA coatings, expression of osteogenic markers, such as type I collagen, alkaline phosphatase, and osterix, was enhanced on the OCP coating plates in an OCP dose-dependent manner [51]. We also reported that OCP enhanced alkaline phosphatase (ALP) activity of mouse mesenchymal stem cell line D1 cells in a three-dimensional cell culture system compared to HA and β-TCP [52]. When rat dental pulp cells were cultured on the OCP or HA coatings, OCP promoted their odontoblastic differentiation more than HA, as confirmed by ALP activity, mineralization, and enhancement of dentine sialophosphoprotein expression [53]. Furthermore, OCP is capable of inducing osteoclast formation from bone marrow cells in vitro in the presence of osteoblasts without vitamin D3 [54].
OCP can gradually convert into the crystal structure of apatite in the physiological conditions [11]. The conversion induces the release of phosphate ions to the periphery of the crystals and the uptake of calcium ion into the crystals [14]. We demonstrated that these changes in ion concentration have effects on osteoblastic differentiation through the phosphorylation of p38 MAP kinase [55], migration of macrophage-like cells [56], and osteoclastic differentiation by the increase of the expression of RANKL in osteoblasts [54].
5 Conclusion
We have designed OCP-based materials and reported their tissue regenerative properties not only in the calcified tissues but also in the noncalcified tissue. The physicochemical properties of OCP induced in the conversion process from OCP to HA could be involved in promoting osteoblastic and osteoclastic differentiation and bone formation and reformation of infraspinatus tendon insertion. The composite materials of OCP with natural polymers, described in this article, could be used as scaffold materials for mineralized tissue regeneration and potentially for non-mineralized tissue regeneration.
References
LeGeros RZ. Calcium phosphate-based osteoinductive materials. Chem Rev. 2008;108:4742–53.
Matsushima A, Kotobuki N, Tadokoro M, Kawate K, Yajima H, Takakura Y, et al. In vivo osteogenic capability of human mesenchymal cells cultured on hydroxyapatite and on beta-tricalcium phosphate. Artif Organs. 2009;33:474–81.
Liu Y, Cooper PR, Barralet JE, Shelton RM. Influence of calcium phosphate crystal assemblies on the proliferation and osteogenic gene expression of rat bone marrow stromal cells. Biomaterials. 2007;28:1393–403.
Sun JS, Tsuang YH, Chang WH, Li J, Liu HC, Lin FH. Effect of hydroxyapatite particle size on myoblasts and fibroblasts. Biomaterials. 1997;18:683–90.
Suzuki O, Nakamura M, Miyasaka Y, Kagayama M, Sakurai M. Bone formation on synthetic precursors of hydroxyapatite. Tohoku J Exp Med. 1991;164:37–50.
Brown W. Crystal growth of bone mineral. Clin Orthop Relat Res. 1966;44:205–20.
Brown WE, Smith JP, Lehr JR, Frazier AW. Crystallographic and chemical relations between octacalcium phosphate and hydroxyapatite. Nature. 1962;196:1050–5.
Eanes ED, Gillessen IH, Posner AS. Intermediate states in the precipitation of hydroxyapatite. Nature. 1965;208:365–7.
Miyatake N, Kishimoto KN, Anada T, Imaizumi H, Itoi E, Suzuki O. Effect of partial hydrolysis of octacalcium phosphate on its osteoconductive characteristics. Biomaterials. 2009;30:1005–14.
Honda Y, Anada T, Kamakura S, Morimoto S, Kuriyagawa T, Suzuki O. The effect of microstructure of octacalcium phosphate on the bone regenerative property. Tissue Eng Part A. 2009;15:1965–73.
Suzuki O. Octacalcium phosphate: osteoconductivity and crystal chemistry. Acta Biomater. 2010;6:3379–87.
Suzuki O. Octacalcium phosphate (OCP)-based bone substitute materials. Jpn Dent Sci Rev. 2013;49:58–71.
Kawai T, Echigo S, Matsui K, Tanuma Y, Takahashi T, Suzuki O, et al. First clinical application of octacalcium phosphate collagen composite in human bone defect. Tissue Eng Part A. 2014;20:1336–41.
Suzuki O, Kamakura S, Katagiri T. Surface chemistry and biological responses to synthetic octacalcium phosphate. J Biomed Mater Res B Appl Biomater. 2006;77:201–12.
Suzuki O, Kamakura S, Katagiri T, Nakamura M, Zhao B, Honda Y, et al. Bone formation enhanced by implanted octacalcium phosphate involving conversion into Ca-deficient hydroxyapatite. Biomaterials. 2006;27:2671–81.
Kobayashi K, Anada T, Handa T, Kanda N, Yoshinari M, Takahashi T, et al. Osteoconductive property of a mechanical mixture of octacalcium phosphate and amorphous calcium phosphate. ACS Appl Mater Interfaces. 2014;6:22602–11.
Handa T, Anada T, Honda Y, Yamazaki H, Kobayashi K, Kanda N, et al. The effect of an octacalcium phosphate co-precipitated gelatin composite on the repair of critical-sized rat calvarial defects. Acta Biomater. 2012;8:1190–200.
Ishiko-Uzuka R, Anada T, Kobayashi K, Kawai T, Tanuma Y, Sasaki K, et al. Oriented bone regenerative capacity of octacalcium phosphate/gelatin composites obtained through two-step crystal preparation method. J Biomed Mater Res B Appl Biomater 2016 in press.
Suzuki K, Honda Y, Anada T, Handa T, Miyatake N, Takahashi A, et al. Stimulatory capacity of an octacalcium phosphate/gelatin composite on bone regeneration. Phosphorus Res Bull. 2012;26:53–8.
Itoigawa Y, Suzuki O, Sano H, Anada T, Handa T, Hatta T, et al. The role of an octacalcium phosphate in the re-formation of infraspinatus tendon insertion. J Shoulder Elbow Surg. 2015;24:e175–84.
Asran AS, Henning S, Michler GH. Polyvinyl alcohol–collagen–hydroxyapatite biocomposite nanofibrous scaffold: Mimicking the key features of natural bone at the nanoscale level. Polymer. 2010;51:868–76.
Curtin CM, Cunniffe GM, Lyons FG, Bessho K, Dickson GR, Duffy GP, et al. Innovative collagen nano-hydroxyapatite scaffolds offer a highly efficient non-viral gene delivery platform for stem cell-mediated bone formation. Adv Mater. 2012;24:749–54.
Kikuchi M, Itoh S, Ichinose S, Shinomiya K, Tanaka J. Self-organization mechanism in a bone-like hydroxyapatite/collagen nanocomposite synthesized in vitro and its biological reaction in vivo. Biomaterials. 2001;22:1705–11.
Liu Y, Li N, Qi YP, Dai L, Bryan TE, Mao J, Pashley DH, Tay FR. Intrafibrillar collagen mineralization produced by biomimetic hierarchical nanoapatite assembly. Adv Mater. 2011;23:975–80.
Gotterbarm T, Richter W, Jung M, Berardi Vilei S, Mainil-Varlet P, Yamashita T, et al. An in vivo study of a growth-factor enhanced, cell free, two-layered collagen-tricalcium phosphate in deep osteochondral defects. Biomaterials. 2006;27:3387–95.
Honda Y, Kamakura S, Sasaki K, Suzuki O. Formation of bone-like apatite enhanced by hydrolysis of octacalcium phosphate crystals deposited in collagen matrix. J Biomed Mater Res B Appl Biomater. 2007;80:281–9.
Kamakura S, Sasaki K, Honda Y, Anada T, Suzuki O. Octacalcium phosphate combined with collagen orthotopically enhances bone regeneration. J Biomed Mater Res B Appl Biomater. 2006;79:210–17.
Bigi A, Panzavolta S, Roveri N. Hydroxyapatite-gelatin films: a structural and mechanical characterization. Biomaterials. 1998;19:739–44.
Chang MC, Ko CC, Douglas WH. Preparation of hydroxyapatite-gelatin nanocomposite. Biomaterials. 2003;24:2853–62.
Kim HW, Kim HE, Salih V. Stimulation of osteoblast responses to biomimetic nanocomposites of gelatin-hydroxyapatite for tissue engineering scaffolds. Biomaterials. 2005;26:5221–30.
Liu X, Smith L, Hu J, Ma PX. Biomimetic nanofibrous gelatin/apatite composite scaffolds for bone tissue engineering. Biomaterials. 2009;30:2252–8.
Choi Y, Cho S, Park DJ, Park HH, Heo S, Jin HJ. Silk fibroin particles as templates for mineralization of calcium-deficient hydroxyapatite. J Biomed Mater Res Part B. 2012;100B:2029–34.
Manjubala I, Shelor S, Bössert J, Jandt KD. Mineralisation of chitosan scaffolds with nano-apatite formation by double diffusion technique. Acta Biomater. 2006;2:75–84.
Shi P, Teh T, Toh SL, Goh JC. Variation of the effect of calcium phosphate enhancement of implanted silk fibroin ligament bone integration. Biomaterials. 2013;34:5947–57.
Thein-Han WW, Misra RD. Biomimetic chitosan-nanohydroxyapatite composite scaffolds for bone tissue engineering. Acta Biomater. 2009;5:1182–97.
Wang G, Zheng L, Zhao H, Miao J, Sun C, Liu H, Huang Z, Yu X, Wang J, Tao X. Construction of a fluorescent nanostructured chitosan-hydroxyapatite scaffold by nanocrystallon induced biomimetic mineralization and its cell biocompatibility. ACS Appl Mater Interfaces. 2011;3:1692–701.
Zhang Y, Zhang M. Synthesis and characterization of macroporous chitosan/calcium phosphate composite scaffolds for tissue engineering. J Biomed Mater Res. 2001;55:304–12.
Matsuno T, Hashimoto Y, Adachi S, Omata K, Yoshitaka Y, Ozeki Y, Umezu Y, Tabata Y, Nakamura M, Satoh T. Preparation of injectable 3D-formed beta-tricalcium phosphate bead/alginate composite for bone tissue engineering. Dent Mater J. 2008;27:827–34.
Suárez-González D, Barnhart K, Saito E, Vanderby Jr R, Hollister SJ, Murphy WL. Controlled nucleation of hydroxyapatite on alginate scaffolds for stem cell-based bone tissue engineering. J Biomed Mater Res A. 2010;95:222–34.
Turco G, Marsich E, Bellomo F, Semeraro S, Donati I, Brun F, Grandolfo M, Accardo A, Paoletti S. Alginate/Hydroxyapatite biocomposite for bone ingrowth: a trabecular structure with high and isotropic connectivity. Biomacromolecules. 2009;10:575–1583.
Xie M, Olderoy M, Andreassen JP, Selbach SM, Strand BL, Sikorski P. Alginate-controlled formation of nanoscale calcium carbonate and hydroxyapatite mineral phase within hydrogel networks. Acta Biomater. 2010;6:3665–75.
Fuji T, Anada T, Honda Y, Shiwaku Y, Koike H, Kamakura S, et al. Octacalcium phosphate-precipitated alginate scaffold for bone regeneration. Tissue Eng Part A. 2009;15:3525–35.
Shiraishi N, Anada T, Honda Y, Masuda T, Sasaki K, Suzuki O. Preparation and characterization of porous alginate scaffolds containing various amounts of octacalcium phosphate (OCP) crystals. J Mater Sci Mater Med 2010 in press.
Smetana Jr K. Cell biology of hydrogels. Biomaterials. 1993;14:1046–50.
Endo K, Anada T, Yamada M, Seki M, Sasaki K, Suzuki O. Enhancement of osteoblastic differentiation in alginate gel beads with bioactive octacalcium phosphate particles. Biomed Mater. 2015;10:065019.
Jeong SH, Fan Y, Baek JU, Song J, Choi TH, Kim SW, Kim HE. Long-lasting and bioactive hyaluronic acid-hydroxyapatite composite hydrogels for injectable dermal fillers: physical properties and in vivo durability. J Biomater Appl 2016 in press.
Lee JH, Kim J, Baek HR, Lee KM, Seo JH, Lee HK, Lee AY, Zheng GB, Chang BS, Lee CK. Fabrication of an rhBMP-2 loaded porous β-TCP microsphere-hyaluronic acid-based powder gel composite and evaluation of implant osseointegration. J Mater Sci Mater Med. 2014;25:2141–51.
Suzuki K, Anada T, Miyazaki T, Miyatake N, Honda Y, Kishimoto KN, et al. Effect of addition of hyaluronic acids on the osteoconductivity and biodegradability of synthetic octacalcium phosphate. Acta Biomater. 2014;10:531–43.
Takahashi Y, Yamamoto M, Tabata Y. Osteogenic differentiation of mesenchymal stem cells in biodegradable sponges composed of gelatin and beta-tricalcium phosphate. Biomaterials. 2005;26:3587–96.
Kino R, Ikoma T, Monkawa A, Yunoki S, Munekata M, Tanaka J, Asakura T. Deposition of bone-like apatite on modified silk fibroin films from simulated body fluid. J Appl Polym Sci. 2006;99:2822–30.
Anada T, Kumagai T, Honda Y, Masuda T, Kamijo R, Kamakura S, et al. Dose-dependent osteogenic effect of octacalcium phosphate on mouse bone marrow stromal cells. Tissue Eng Part A. 2008;14:965–78.
Anada T, Sato T, Kamoya T, Shiwaku Y, Tsuchiya K, Takano-Yamamoto T, Sasaki K, Suzuki O. Evaluation of bioactivity of octacalcium phosphate using osteoblastic cell aggregates on a spheroid culture device. Regen Ther. 2016;3:58–62.
Wang X, Suzawa T, Miyauchi T, Zhao B, Yasuhara R, Anada T, et al. Synthetic octacalcium phosphate-enhanced reparative dentine formation via induction of odontoblast differentiation. J Tissue Eng Regen Med. 2015;9:1310–20.
Takami M, Mochizuki A, Yamada A, Tachi K, Zhao B, Miyamoto Y, et al. Osteoclast differentiation induced by synthetic octacalcium phosphate through RANKL expression in osteoblasts. Tissue Eng Part A. 2009;15:3991–4000.
Nishikawa R, Anada T, Ishiko-Uzuka R, Suzuki O. Osteoblastic differentiation of stromal ST-2 cells from octacalcium phosphate exposure via p38 signaling pathway. Dent Mater J. 2014;33:242–51.
Hirayama B, Aanda T, Shiwaku Y, Miyatake N, Tsuchiya K, Nakamura M, Takahashi T, Suzuki O. Immune cell response and subsequent bone formation induced by implantation of octacalcium phosphate in a rat tibia defect. RSC Adv. 2016;6:57475–84.
Acknowledgments
The studies reported in the present article were supported in part by Grants-in-aid (23106010, 26293417, and 15K15720) from the Ministry of Education, Science, Sports, and Culture of Japan.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
This chapter is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, duplication, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the work’s Creative Commons license, unless indicated otherwise in the credit line; if such material is not included in the work’s Creative Commons license and the respective action is not permitted by statutory regulation, users will need to obtain permission from the license holder to duplicate, adapt or reproduce the material.
Copyright information
© 2017 The Author(s)
About this paper
Cite this paper
Suzuki, O., Anada, T., Shiwaku, Y. (2017). Efficacy of Calcium Phosphate-Based Scaffold Materials on Mineralized and Non-mineralized Tissue Regeneration. In: Sasaki, K., Suzuki, O., Takahashi, N. (eds) Interface Oral Health Science 2016. Springer, Singapore. https://doi.org/10.1007/978-981-10-1560-1_10
Download citation
DOI: https://doi.org/10.1007/978-981-10-1560-1_10
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-1559-5
Online ISBN: 978-981-10-1560-1
eBook Packages: MedicineMedicine (R0)