Abstract
In liver transplantation, prolonged ischemia and/or a relatively small graft (living, split, reduced) are the risk factors for liver dysfunction. Novel measures to enhance liver function with a smaller graft can be a clue for safe partial or living-donor liver transplantation or safe hepatectomy for malignant disease. The therapeutic potential and immunomodulatory effects of mesenchymal stem cells (MSCs) have been reported. In this chapter, recent finding on the positive effect of MSCs for liver transplantation and hepatectomy are discussed.
Our rat experiment revealed that introduction of MSCs provides trophic support to the I/R-injured liver by inhibiting hepatocellular apoptosis and by stimulating regeneration, which is shown with the pig model as well. In the rat liver transplantation model, portal transfusion of the MSCs ameliorates the injury of the liver graft after prolonged cold preservation and transplantation. Those findings together suggest a potential advantage with partial or living-donor liver transplantation. The most severe complication with cell therapy is embolus formation due to cell aggregation. However, with modification of the solution, we can keep cells in a suspended form for several hours, which secures safe administration of MSCs.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
Keywords
- Liver transplantation
- Mesenchymal stem cell
- Hepatectomy
- Ischemia
- Reperfusion
- Liver failure
- Living donor
- Partial liver transplantation
Clinical Liver Transplantation: Deceased Donor vs. Living Donor
Statistics
Liver transplantation has been successfully used as a treatment for end-stage liver disease, though there has been discussion regarding where the liver graft is obtained, i.e., from a deceased donor or a living donor. In the USA, the majority of liver transplantation is done with deceased donors, and the number of living-donor liver transplantations (LDLTs) is limited. The reason why LDLT is not popular in the USA is due to the death of a donor in 2002. Since 2001, the number of patients who have undergone LDLT has declined. On the other hand, in Japan, most liver transplantation is done with LDLT. Though the organ transplantation law took effect in 1997, the number of deceased donor liver transplantations (DDLTs) has been minimal; this is partly because the law itself is very strict in comparison with those of Western countries. Even since modification of the law in 2010, the annual number of DDLTs has been limited to below 50. The ratio of the numbers of LDLTs to DDLTs is 10:1 [1].
Operations and the Post-transplant Course
In DDLT, the whole liver is used, and it has a high reserve capacity (Fig. 1). In other words, the liver volume is sufficient for the recipient throughout the postoperative course from the immediate post-transplant period. That is true with LDLT as well; therefore, a larger graft is preferable in terms of the recipient’s postoperative course. However, harvesting a larger graft from a living donor may cause complications, and there have been some reports of donor deaths. Currently, we primarily use smaller grafts such as left lobe grafts, in our program, though small-for-size syndrome (SFSS) occasionally follows in recipients, which can be lethal. Since LDLT is a type of partial liver transplantation (PLTx), the possibility of SFSS is unavoidable. Functional impairment conditions such as prolonged cholestasis, ascites, coagulopathy, and encephalopathy are considered to result from SFSS that occurs after LDLT [2]. They strongly affect patient survival and clinical costs for the whole treatment. Therefore, novel measures to enhance liver function with smaller grafts may be the key to safe PLTx or LDLT.
Postoperative course of whole vs. partial liver transplantation, showing the difference between DDLT and LDLT after the operation. There is no change in size with DDLT, whereas graft enlargement is observed with LDLT. Functional recovery follows volume recovery; therefore, there should be some critical period with LDLT after operation
Mesenchymal Stem Cells
Characteristics
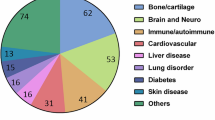
Mesenchymal stem cells (MSCs), present in the human body in large amounts, can be candidates for stem cell–based therapy for liver diseases. Recently, the therapeutic potential and immunomodulatory effect of MSCs have been revealed. Adipose tissue–derived mesenchymal stem cells (AT-MSCs), because of their high accessibility with minimal invasiveness, are especially attractive in the context of future clinical applications. MSCs can differentiate into multiple types of lineages, such as chondrogenic, osteogenic, and adipogenic, depending on the microenvironment around them. Importantly, human MSCs represent an advantageous cell type for allogeneic transplantation, as they are immunoprivileged with low human leukocyte antigen (HLA) I and no HLA II expression, thereby reducing the risk of allogeneic transplant rejection and preventing graft-versus-host disease (GVHD). According to Banas et al., adipose tissue–derived (AT) MSCs can improve liver functions, which we have verified by changes in the levels of biochemical parameters. Ammonia, uric acid, glutamic–pyruvic transaminase, and glutamic–oxaloacetic transaminase concentrations returned to a nearly normal level after AT-MSC transplantation. It was shown that AT-MSCs secrete interleukin 1 receptor (IL-1R), IL-6, IL-8, granulocyte colony–stimulating factor (G-CSF), granulocyte-macrophage colony–stimulating factor (GM-CSF), monocyte chemotactic protein 1, nerve growth factor, and hepatocyte growth factor, suggesting that AT-MSCs account for broad therapeutic efficacy in animal models of liver diseases and in the clinical settings of liver disease treatment [3].
Isolation Techniques
AT-MSCs can be derived from subcutaneous adipose tissue. Adipose tissue was minced with scissors and scalpels into less than 3 mm pieces and, after gentle shaking with an equal volume of PBS(−), the mixture was separated into two phases. The upper phase (containing stem cells, adipocytes, and blood), after washing with phosphate-buffered saline (PBS) (−), was enzymatically dissociated with 0.075 % collagenase (type I)/PBS(−) for 1 h at 37 °C with gentle shaking. The dissociated tissue was then mixed with an equal volume of DMEM, supplemented with 10 % fetal bovine serum (FBS) and incubated for 10 min at room temperature. The solution was then separated into two phases. The lower phase was centrifuged at 1500 rpm for 5 min at 20 °C. The cellular pellet was resuspended in 160 mM NH4Cl to eliminate erythrocytes and passed through a 40 μm mesh filter into a new tube. The cells were resuspended in an equal volume of DMEM/10 % FBS and then centrifuged. Isolation resulted in obtaining 7.7 × 106 of adherent cells for a primary culture from 5 g of adipose tissue (approximately 1.0 × 105 to 4.6 × 106/1 g) after 7–10 days of culture. The cells were suspended in DMEM/10 % FBS plated in a concentration of 1–5 × 106 cells/75 cm2. The cells with 70–80 % confluence were harvested with 0.25 % trypsin EDTA and then re-plated at 1.0 × 105 cells/60 mm dish and used for analysis [4].
Mesenchymal Stem Cells for Rat Hepatectomy
Rat Hepatectomy Model
Our rat model provided the ideal animal model to research I/R injury after major hepatectomy by the Pringle maneuver or liver transplantation with small-for-size grafts (Fig. 2) [5]. Intestinal congestion was avoided during the application of hepatic ischemia by bypassing portal flow through nonischemic lobes (the right and caudate lobes). Moreover, the left lateral and the left portion of the medial lobes, as well as the nonischemic lobes, were excised at the onset of reflow to mimic the clinical condition of liver transplantation with small-for-size grafts or major hepatectomy by the Pringle maneuver in order to research postischemic liver functions.
Outcome After MSC Injection
Male Lewis rats were separated into two groups: an MSC group given MSCs after reperfusion as a treatment, and a control group given phosphate-buffered saline after reperfusion as a placebo. The results of liver function tests, pathologic changes in the liver, and the remnant liver regeneration rate were assessed. The fate of transplanted MSCs in the luciferase-expressing rats was examined by in vivo luminescent imaging. The MSC group showed peak luciferase activity of transplanted MSCs in the remnant liver 24 h after reperfusion, after which luciferase activity gradually declined. The elevation of serum alanine transaminase levels was significantly reduced by the MSC injection. Histopathological findings showed that the vacuolar change was lesser in the MSC group than in the control group. In addition, a significantly lower percentage of TUNEL-positive cells was observed in the MSC group than in the controls. The remnant liver regeneration rate was accelerated in the MSC group. The above results suggest that MSC transplantation provides trophic support to the I/R-injured liver by inhibiting hepatocellular apoptosis and by stimulating regeneration.
Mesenchymal Stem Cells for Pig Ischemia/Reperfusion Injury
Pig Ischemia Reperfusion Model
Following rat hepatectomy experiments, a preclinical pig model was introduced (Fig. 3). In our model, long warm ischemia of up to 90 min is simulated for Pringle’s procedure during hepatectomy or ischemia/reperfusion injury during liver transplantation. Inflow occlusion, such as Pringle’s occlusion for a long period, causes mesenteric congestion, which affects the outcome and can sometimes be lethal. Therefore, a portacaval shunt between the splenic vein and the internal jugular vein was placed during inflow occlusion. The clamp was place at the hepatoduodenal ligament for 90 min with intensive monitoring for vital signs. After the declamp, MSCs (1.0 × 107/kg) were injected in the MSC group. An initial problem with the MSC injection was probable hepatic embolism. Injection of the MSCs just after collection from the plates led to severe aggregation of cells, followed by embolus formation. Accordingly, we modified our protocol by immersing the MSCs in an ET-Kyoto solution so that the cells would not aggregate. Thereafter, no lethal complication was encountered. After the procedure, the pig was monitored for survival and daily laboratory examinations including AST, ALT, LDH, and portal venous pressure.
Outcome After MSC Injection (Fig. 4)
All pigs in the MSC group (n = 5) and control group (n = 5) survived during an observation period for 7 days. In the control group, AST, ALT, and LDH peaked several hours after the operation and returned to normal in 3 days. However, this increase in laboratory parameters was not observed in the MSC group. In terms of adverse effects, portal venous pressure (PVP) was kept stable without an increase throughout the course, in both the MSC group and the control group. Therefore, the modified method for cell preparation is effective to avoid cell aggregation and leads to safe application of this method in the clinical setting. As we see from the laboratory results, the protective effect of MSCs is suggested in prolonged warm ischemia during surgery. This may lead to wider indications in liver surgery and transplantation.
Mesenchymal Stem Cells for Rat Whole Liver Transplantation with a Long Preservation Period
Rat Liver Transplantation Model
In the previous section, we showed that MSCs provide a protective effect against hepatic ischemia- reperfusion injury and stimulate liver regeneration in rat hepatectomy. We further evaluated the effect of MSCs on liver transplantation after prolonged cold preservation by using a rat liver transplantation model. Adipose tissue–derived MSCs from luciferase-transgenic Lewis (Luc-Tg LEW) rats were cultured and preserved in ET-Kyoto solution before use. Male Lewis rats were used as transplantation donors and recipients. The rats were randomly assigned to two groups: an MSC group and a control group. The liver grafts were retrieved and preserved in UW solution at 4 °C for 24 h. After preservation, 1 × 105 of MSCs in 0.2 ml of ET-Kyoto solution were transfused via the portal vein of the graft in the MSC group, and ET-Kyoto solution only was transfused in the control group. Then the liver graft was orthotopically transplanted into a recipient rat by the cuff technique of Kamada and Calne, with minor modification. Both the superior and inferior hepatic vena cava were anastomosed by a running suture. The portal vein was connected by a polyethylene cuff and the bile duct by a stent. The hepatic artery was reconstructed by the sleeve method. The survival of the recipient rats was evaluated for 7 days after transplantation.
Outcome After MSCs Injection
The anhepatic times were 15.5 ± 0.7 min in the MSC group and 15.4 ± 1.3 min in the control group. The inferior vena cava clamping times were 27.6 ± 1.2 min and 27.1 ± 1.7 min, respectively. Both parameters did not differ significantly between the groups. Liver enzymes were better in the MSC group. In the control group, prominent necrosis and ballooning of cells in the adjacent area were observed, whereas the findings were almost normal in the MSC group (Fig. 5). In the MSC group, DLK/OV6 double positive cells were observed, whereas positive cells were minimal in the control group. These data support the positive effect of MSCs in ameliorating ischemia/reperfusion injury. The regenerative effect of MSCs was shown as well. The 7-day survival was significantly better in the MSC group than in the control group (7/8 vs. 3/8; Fisher’s exact test, p < 0.05) (Fig. 6). Portal transfusion of the MSCs ameliorated the injury of the liver graft after prolonged cold preservation and transplantation.
Experimental Models for Clinical Application
Reduced Liver Transplantation (Rat) as a Model for Living-Donor Liver Transplantation
During the donor operation, the right lobe (RL) of the liver was selected as the graft for the 20 % PLTx group, while the superior right lobe (SRL) was selected for the 15 % PLTx group, on the basis of the rat liver anatomy. Liver grafts were preserved in ice-cold HTK solution before implantation for 180 min. The SHVC was sewn with an 8-0 Prolene continuous suture, and the portal vein was anastomosed using a cuff technique. After confirming reflow, the infrahepatic vena cava (IHVC) was anastomosed using an 8-0 nylon continuous suture. The hepatic artery was connected using a sleeve technique, and the bile duct was reconstructed over an intraluminal stent. With this model, 7-day survival was 100 % with the 20 % graft and 17 % with the 15 % graft. Experiments assessing the efficacy of MSCs are under evaluation.
Partial Liver Transplantation (Pig) as a Model for Living-Donor Liver Transplantation
For this preclinical study, the Clawn miniature pig was used for the partial liver transplantation model [6]. The porcine liver consists of four lobes. The right lateral lobe (RLL) accounts for 30 % of the whole liver. The structure of the porta hepatis was carefully dissected and cut in order to resect the lobes other than the RLL. Seventy percent of the liver was resected in the donor, not on the back table, to confirm hemostasis. Then the graft was preserved in the preservation solution for 3–24 h, followed by implantation into the recipient. In the recipient, prior to total hepatectomy, a portacaval shunt was placed to avoid mesenteric congestion. The inferior vena cava (suprahepatic and infrahepatic), portal vein, hepatic artery, and bile duct were sewn (Fig. 7).
Future Perspectives
Source for MSCs
MSC have been isolated from almost every type of tissue stroma, such as the bone marrow, adipose tissue, umbilical cord blood, placenta, kidney, liver, heart, and spleen. There are many reports on the positive immunomodulatory effect or regenerative effect of MSCs of bone marrow origin. However, retrieval of bone marrow from healthy volunteers or patients seems invasive. On the other hand, Banas et al. reported a stronger effect of adipose tissue–derived MSCs compared with BM-MSCs. Moreover, subcutaneous adipose tissue can be safely retrieved under local anesthesia or during a major operation. We have been focusing on utilizing MSCs from adipose tissue. The remaining problem is from whom and when adipose tissue can be retrieved. Potential donors are the patient him- or herself, the donor of the organ in transplantation, or a third party. One of the advantages of MSCs compared with other cell sources is that MSCs express less HLA, leading to less rejection. Moreover, the regenerative or immunomodulatory effects are expected only in the short term, not in the long term. For use in cancer patients, we propose use of the patient’s own MSCs without immunosuppression. On the other hand, cells from all three sources can be utilized in transplant recipients under immunosuppression. For an elective cancer operation, the patient’s own MSCs can be retrieved and cultured for several weeks. However, stocked cells from a third party can be used for organ transplantation performed on an emergency basis [7, 8].
Complications
The most severe complication we have encountered is embolus formation due to cell aggregation. However, with the modification using ET-Kyoto solution, we can keep cells in a suspended form for several hours, which secures safe administration of the MSCs. ET-Kyoto solution is commercially available, and its safety is established. Potential transformation of MSCs into malignant cells can be problematic; however, the lifespan of the cells is limited, according to our study, and they can be eliminated within 2 weeks. Mild rejection will help to eliminate cells after a certain period as well.
Conclusion
Thanks to the support of the Uehara Memorial Foundation, we have been able to show the positive effect of MSCs with liver surgery. Cell damage during ischemia reperfusion injury is ameliorated, and liver regeneration after hepatectomy is enhanced by use of intravenous or intraportal MSCs. These positive effects have been shown both in vitro and in vivo including in a preclinical pig model.
References
Uemoto S (2010) [Liver transplantation]. Nihon Rinsho 68(12):2277–2280
Yagi S et al (2012) Small-for-size syndrome in living donor liver transplantation. Hepatobiliary Pancreat Dis Int 11(6):570–576
Banas A et al (2008) IFATS collection: in vivo therapeutic potential of human adipose tissue mesenchymal stem cells after transplantation into mice with liver injury. Stem Cells 26(10):2705–2712
Banas A et al (2007) Adipose tissue-derived mesenchymal stem cells as a source of human hepatocytes. Hepatology 46(1):219–228
Kanazawa H et al (2011) Bone marrow-derived mesenchymal stem cells ameliorate hepatic ischemia reperfusion injury in a rat model. PLoS One 6(4):e19195
Hori T et al (2014) How to successfully resect 70 % of the liver in pigs to model an extended hepatectomy with an insufficient remnant or liver transplantation with a small-for-size graft. Surg Today 44(11):2201–2207
Dahlke MH et al (2009) Toward MSC in solid organ transplantation: 2008 position paper of the MiSOT Study Group. Transplantation 88(5):614–619
Franquesa M et al (2013) Mesenchymal Stem Cells in Solid Organ Transplantation (MiSOT) Fourth Meeting: lessons learned from first clinical trials. Transplantation 96(3):234–238
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is distributed under the terms of the Creative Commons Attribution Noncommercial License, which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Copyright information
© 2015 The Author(s)
About this paper
Cite this paper
Uemoto, S. et al. (2015). Introduction of Mesenchymal Stem Cells for Liver Surgery (Hepatectomy and Transplantation). In: Nakao, K., Minato, N., Uemoto, S. (eds) Innovative Medicine. Springer, Tokyo. https://doi.org/10.1007/978-4-431-55651-0_23
Download citation
DOI: https://doi.org/10.1007/978-4-431-55651-0_23
Publisher Name: Springer, Tokyo
Print ISBN: 978-4-431-55650-3
Online ISBN: 978-4-431-55651-0
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)