Abstract
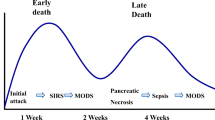
Acute pancreatitis is an inflammatory process of the pancreas with a highly variable clinical course. Its severe complications are still a tough challenge for surgeons. A consensus about the classification has not been reached yet: too many scoring systems exist; they typically require 48 h to become accurate, when the assessment of an experienced surgeon provides evaluation of the disease outcome as good as any grading score. An accurate early prediction of the acute pancreatitis evolution remains uncertain, and a unique reliable classification is still an open matter.
Biliary etiology is the leading cause, and recurrent biliary events are common in the first 30 days from index episode. Subsequent attacks could be more severe than the first one; so they have to be prevented. In mild acute pancreatitis, if no common bile duct obstruction but gallstones are detected, laparoscopic cholecystectomy should be performed during the index hospitalization, as soon as pancreatitis symptoms cool off.
20 % of biliary pancreatitis have persistent bile duct stones. In case of common bile duct stones clearance should be obtained by preoperative ERCP or, in selected centers, by laparoscopic removal of bile duct stones during cholecystectomy. Probably a waiting period of 48 h may give more opportunities to a small stone wedged in the papilla of Oddi to pass spontaneously into the duodenum. Acute cholangitis and persistent bile duct obstruction are indications for urgent ERCP.
Surgery is contraindicated in severe acute pancreatitis: the only permitted surgical indications requiring an emergency laparotomy are acute complications such as abdominal compartment syndrome, bowel ischemia, ongoing acute bleeding, or gastric outlet, intestinal, or biliary obstruction.
When pancreatic necrosis requires treatment for clinical signs of sepsis or multiorgan failure that does not improve despite optimal therapy, a step-up approach consisting of percutaneous drainage, followed, if necessary, by minimally invasive retroperitoneal debridement should be undertaken. Open surgery should be reserved to patients not responding to minimally invasive treatment and in acute complications, because it does not maintain abdominal compartmentalization and may cause intra-abdominal spread of the infection.
The abdominal compartment syndrome is the most lethal complication in the course of severe acute pancreatitis. It should be managed by prompt laparostomy or fasciotomy; today laparoscopy is formally contraindicated in these cases.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Bradley EL, Dexter ND (2010) Management of severe acute pancreatitis: a surgical odyssey. Ann Surg 251:6–17. doi:10.1097/SLA.0b013e3181c72b79
Banks PA, Bollen TL, Dervenis C et al (2013) Classification of acute pancreatitis—2012: revision of the Atlanta classification and definitions by international consensus. Gut 62:102–111
Talukdar R, Bhattacharrya A, Rao B et al (2014) Clinical utility of the revised Atlanta classification of acute pancreatitis in a prospective cohort: have all loose ends been tied? Pancreatol Off J Int Assoc Pancreatol IAP Al 14:257–262. doi:10.1016/j.pan.2014.06.003
Dellinger EP, Forsmark CE, Layer P et al (2012) Determinant-based classification of acute pancreatitis severity: an international multidisciplinary consultation. Ann Surg 256:875–880
Acevedo-Piedra NG, Moya-Hoyo N, Rey-Riveiro M et al (2014) Validation of the determinant-based classification and revision of the Atlanta classification systems for acute pancreatitis. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc 12:311–316. doi:10.1016/j.cgh.2013.07.042
van Santvoort H, Bakker O, Besselink M et al (2011) Prediction of common bile duct stones in the earliest stages of acute biliary pancreatitis. Endoscopy 43:8–13. doi:10.1055/s-0030-1255866
Schepers NJ, Besselink MGH, van Santvoort HC et al (2013) Early management of acute pancreatitis. Best Pract Res Clin Gastroenterol 27:727–743. doi:10.1016/j.bpg.2013.08.007
Bollen TL, Singh VK, Maurer R et al (2012) A comparative evaluation of radiologic and clinical scoring systems in the early prediction of severity in acute pancreatitis. Am J Gastroenterol 107:612–619. doi:10.1038/ajg.2011.438
Brisinda G, Crocco A, Giustacchini P (2014) Classification of the severity of acute pancreatitis: how much is really needed for a new classification? Ann Surg. doi:10.1097/SLA.0000000000000625
Bernardoni L, Frulloni L, Benini L, Gabbrielli A (2014) Aggiornamento delle linee guida della pancreatite acuta. Giorn Ital Endosc Dig 37:25–30
Cho JH, Kim TN, Chung HH, Kim KH (2015) Comparison of scoring systems in predicting the severity of acute pancreatitis. World J Gastroenterol 21:2387–2394. doi:10.3748/wjg.v21.i8.2387
Bakker OJ, Issa Y, van Santvoort HC et al (2014) Treatment options for acute pancreatitis. Nat Rev Gastroenterol Hepatol 11:462–469. doi:10.1038/nrgastro.2014.39
Kuo DC, Rider AC, Estrada P, et al (2015) Acute pancreatitis: what’s the score? J Emerg Med. doi:10.1016/j.jemermed.2015.02.018
Andersson B, Andrén-Sandberg Å, Nilsson J, Andersson R (2012) Survey of the management of acute pancreatitis in surgical departments in Sweden. Scand J Gastroenterol 47:1064–1070. doi:10.3109/00365521.2012.685752
Talukdar R, Rau BM (2015) Determinant-based classification of severity of acute pancreatitis: have we really reached consensus? Ann Surg 261, e22. doi:10.1097/SLA.0000000000000507
Petrov MS, Vege SS, Windsor JA (2012) Global survey of controversies in classifying the severity of acute pancreatitis. Eur J Gastroenterol Hepatol 24:715–721. doi:10.1097/MEG.0b013e328351d340
(2013) IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology 13:e1–e15. doi:10.1016/j.pan.2013.07.063
Tenner S, Baillie J, DeWitt J, et al (2013) American College of Gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol 108:1400–1415, 1416. doi:10.1038/ajg.2013.218
Yadav D (2014) Acute pancreatitis: too many classifications-what is a clinician or researcher to do? Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc 12:317–319. doi:10.1016/j.cgh.2013.09.051
Kokosis G, Perez A, Pappas TN (2014) Surgical management of necrotizing pancreatitis: an overview. World J Gastroenterol 20:16106–16112. doi:10.3748/wjg.v20.i43.16106
Yokoe M, Takada T, Mayumi T et al (2015) Japanese guidelines for the management of acute pancreatitis: Japanese Guidelines 2015. J Hepato-Biliary-Pancreat Sci 22:405–432. doi:10.1002/jhbp.259
Italian Association for the Study of the Pancreas (AISP), Pezzilli R, Zerbi A, et al (2015) Consensus guidelines on severe acute pancreatitis. Dig Liver Dis Off J Ital Soc Gastroenterol Ital Assoc Study Liver. doi:10.1016/j.dld.2015.03.022
Shen H-N, Wang W-C, Lu C-L, Li C-Y (2013) Effects of gender on severity, management and outcome in acute biliary pancreatitis. PLoS One 8, e57504. doi:10.1371/journal.pone.0057504
Yadav D, Lowenfels AB (2013) The epidemiology of pancreatitis and pancreatic cancer. Gastroenterology 144:1252–1261. doi:10.1053/j.gastro.2013.01.068
Gurusamy KS, Nagendran M, Davidson BR (2013) Early versus delayed laparoscopic cholecystectomy for acute gallstone pancreatitis. Cochrane Database Syst Rev 9, CD010326
Zhao X, Chen D-Z, Lang R et al (2013) Enhanced recovery in the management of mild gallstone pancreatitis: a prospective cohort study. Surg Today 43:643–647. doi:10.1007/s00595-012-0364-9
Pérez LJR, Parra JF, Aldana Dimas G (2014) Seguridad de la colecistectomía laparoscópica temprana (<48h) para pacientes con pancreatitis aguda biliar leve: revisión sistemática de la literatura y metaanálisis. Cir Esp 92:107–113. doi:10.1016/j.ciresp.2013.01.024
van Baal MC, Besselink MG, Bakker OJ et al (2012) Timing of cholecystectomy after mild biliary pancreatitis: a systematic review. Ann Surg 255:860–866
Nguyen GC, Rosenberg M, Chong RY, Chong CA (2012) Early cholecystectomy and ERCP are associated with reduced readmissions for acute biliary pancreatitis: a nationwide, population-based study. Gastrointest Endosc 75:47–55. doi:10.1016/j.gie.2011.08.028
Mador BD, Panton ONM, Hameed SM (2014) Early versus delayed cholecystectomy following endoscopic sphincterotomy for mild biliary pancreatitis. Surg Endosc 28:3337–3342. doi:10.1007/s00464-014-3621-8
Bakker OJ, van Santvoort HC, Hagenaars JC et al (2011) Timing of cholecystectomy after mild biliary pancreatitis. Br J Surg 98:1446–1454. doi:10.1002/bjs.7587
da Costa DW, Bouwense SA, Schepers NJ et al (2015) Same-admission versus interval cholecystectomy for mild gallstone pancreatitis (PONCHO): a multicentre randomised controlled trial. Lancet Lond Engl 386:1261–1268. doi:10.1016/S0140-6736(15)00274-3
Bouwense SAW, Bakker OJ, van Santvoort HC et al (2011) Safety of cholecystectomy in the first 48 hours after admission for gallstone pancreatitis not yet proven. Ann Surg 253:1053–1054. doi:10.1097/SLA.0b013e3182172dd7
Isogai M, Kaneoka Y, Maeda A (2011) Is early cholecystectomy within 48 hours of admission for mild gallstone pancreatitis classified by ranson score appropriate? Ann Surg 253:1052–1053. doi:10.1097/SLA.0b013e3182172dc4
Johnson PM, Walsh MJ (2012) The impact of intraoperative cholangiography on recurrent pancreatitis and biliary complications in patients with gallstone pancreatitis. J Gastrointest Surg 16:2220–2224. doi:10.1007/s11605-012-2041-0
Castoldi L, De Rai P, Zerbi A et al (2013) Long term outcome of acute pancreatitis in Italy: results of a multicentre study. Dig Liver Dis 45:827–832. doi:10.1016/j.dld.2013.03.012
Johnstone M, Marriott P, Royle TJ et al (2014) The impact of timing of cholecystectomy following gallstone pancreatitis. Surgeon 12:134–140. doi:10.1016/j.surge.2013.07.006
Judkins SE, Moore EE, Witt JE et al (2011) Surgeons provide definitive care to patients with gallstone pancreatitis. Am J Surg 202:673–678. doi:10.1016/j.amjsurg.2011.06.031
El-Dhuwaib Y, Deakin M, David G et al (2012) Definitive management of gallstone pancreatitis in England. Ann R Coll Surg Engl 94:402–406. doi:10.1308/003588412X13171221591934
Hwang SS, Li BH, Haigh PI (2013) Gallstone pancreatitis without cholecystectomy. JAMA Surg 148:867. doi:10.1001/jamasurg.2013.3033
Trust MD, Sheffield KM, Boyd CA et al (2011) Gallstone pancreatitis in older patients: are we operating enough? Surgery 150:515–525. doi:10.1016/j.surg.2011.07.072
Bencini L (2014) Modern approach to cholecysto-choledocholithiasis. World J Gastrointest Endosc 6:32. doi:10.4253/wjge.v6.i2.32
de C Ferreira LEVV, Baron TH (2013) Acute biliary conditions. Best Pract Res Clin Gastroenterol 27:745–756. doi:10.1016/j.bpg.2013.08.008
Sandzén B, Haapamäki MM, Nilsson E et al (2012) Treatment of common bile duct stones in Sweden 1989-2006: an observational nationwide study of a paradigm shift. World J Surg 36:2146–2153. doi:10.1007/s00268-012-1648-3
Dasari BVM, Tan CJ, Gurusamy KS et al (2013) Surgical versus endoscopic treatment of bile duct stones. Cochrane Database Syst Rev 12, CD003327. doi:10.1002/14651858.CD003327.pub4
Baucom RB, Feurer ID, Shelton JS, et al (2015) Surgeons, ERCP, and laparoscopic common bile duct exploration: do we need a standard approach for common bile duct stones? Surg Endosc doi:10.1007/s00464-015-4273-z
Tse F, Yuan Y (2012) Early routine endoscopic retrograde cholangiopancreatography strategy versus early conservative management strategy in acute gallstone pancreatitis. Cochrane Database Syst Rev 5, CD009779. doi:10.1002/14651858.CD009779.pub2
van Geenen E-JM, van Santvoort HC, Besselink MGH et al (2013) Lack of consensus on the role of endoscopic retrograde cholangiography in acute biliary pancreatitis in published meta-analyses and guidelines: a systematic review. Pancreas 42:774–780. doi:10.1097/MPA.0b013e318287d208
Bignell M, Dearing M, Hindmarsh A, Rhodes M (2011) ERCP and endoscopic sphincterotomy (ES): a safe and definitive management of gallstone pancreatitis with the gallbladder left in situ. J Gastrointest Surg Off J Soc Surg Aliment Tract 15:2205–2210. doi:10.1007/s11605-011-1729-x
Worhunsky DJ, Visser BC (2013) Gallstone pancreatitis: why not cholecystectomy? JAMA Surg 148:872. doi:10.1001/jamasurg.2013.3063
Mustafa A, Begaj I, Deakin M et al (2014) Long-term effectiveness of cholecystectomy and endoscopic sphincterotomy in the management of gallstone pancreatitis. Surg Endosc 28:127–133. doi:10.1007/s00464-013-3138-6
van Santvoort HC, Bakker OJ, Bollen TL et al (2011) A conservative and minimally invasive approach to necrotizing pancreatitis improves outcome. Gastroenterology 141:1254–1263. doi:10.1053/j.gastro.2011.06.073
Hajjar NA, Iancu C, Bodea R (2012) Modern therapeutic approach of acute severe forms of pancratitis. A review of the literature and experience of Surgical Department No III Cluj. Chir Buchar Rom 1990 107:605–610
Phillip V, Steiner JM, Algül H (2014) Early phase of acute pancreatitis: assessment and management. World J Gastrointest Pathophysiol 5:158–168. doi:10.4291/wjgp.v5.i3.158
Rodriguez JR, Razo AO, Targarona J et al (2008) Debridement and closed packing for sterile or infected necrotizing pancreatitis: insights into indications and outcomes in 167 patients. Ann Surg 247:294–299. doi:10.1097/SLA.0b013e31815b6976
Raraty MGT, Halloran CM, Dodd S et al (2010) Minimal access retroperitoneal pancreatic necrosectomy: improvement in morbidity and mortality with a less invasive approach. Ann Surg 251:787–793. doi:10.1097/SLA.0b013e3181d96c53
Sermoneta D, Di Mugno M, Spada PL et al (2010) Intra-abdominal vacuum-assisted closure (VAC) after necrosectomy for acute necrotising pancreatitis: preliminary experience. Int Wound J 7:525–530. doi:10.1111/j.1742-481X.2010.00727.x
Besselink MGH, van Santvoort HC, Nieuwenhuijs VB et al (2006) Minimally invasive “step-up approach” versus maximal necrosectomy in patients with acute necrotising pancreatitis (PANTER trial): design and rationale of a randomised controlled multicenter trial [ISRCTN13975868]. BMC Surg 6:6. doi:10.1186/1471-2482-6-6
Mamlouk MD, van Sonnenberg E (2011) Interventional radiology for necrotizing pancreatitis. J Gastrointest Surg Off J Soc Surg Aliment Tract 15:1101–1103. doi:10.1007/s11605-011-1507-9
Fink D, Soares R, Matthews JB, Alverdy JC (2011) History, goals, and technique of laparoscopic pancreatic necrosectomy. J Gastrointest Surg 15:1092–1097. doi:10.1007/s11605-011-1506-x
Bakker OJ, van Santvoort HC, van Brunschot S et al (2012) Endoscopic transgastric vs surgical necrosectomy for infected necrotizing pancreatitis: a randomized trial. JAMA 307:1053. doi:10.1001/jama.2012.276
Bausch D, Wellner U, Kahl S et al (2012) Minimally invasive operations for acute necrotizing pancreatitis: comparison of minimally invasive retroperitoneal necrosectomy with endoscopic transgastric necrosectomy. Surgery 152:S128–S134. doi:10.1016/j.surg.2012.05.021
Babu RY, Gupta R, Kang M et al (2013) Predictors of surgery in patients with severe acute pancreatitis managed by the step-up approach. Ann Surg 257:737–750. doi:10.1097/SLA.0b013e318269d25d
Dupuis CS, Baptista V, Whalen G et al (2013) Diagnosis and management of acute pancreatitis and its complications. Gastrointest Interv 2:36–46. doi:10.1016/j.gii.2013.03.001
Tang C, Wang B, Xie B et al (2011) Treatment of severe acute pancreatitis through retroperitoneal laparoscopic drainage. Front Med 5:302–305. doi:10.1007/s11684-011-0145-7
Wronski M, Cebulski W, Slodkowski M et al (2012) Retroperitoneal minimally invasive pancreatic necrosectomy using single-port access. Surg Laparosc Endosc Percutan Tech 22:e8–e11. doi:10.1097/SLE.0b013e31823fbec5
Fogel EL (2011) Endoscopic pancreatic necrosectomy. J Gastrointest Surg Off J Soc Surg Aliment Tract 15:1098–1100. doi:10.1007/s11605-011-1505-y
Worhunsky DJ, Qadan M, Dua MM et al (2014) Laparoscopic transgastric necrosectomy for the management of pancreatic necrosis. J Am Coll Surg 219:735–743. doi:10.1016/j.jamcollsurg.2014.04.012
Bang JY, Holt BA, Hawes RH et al (2014) Outcomes after implementing a tailored endoscopic step-up approach to walled-off necrosis in acute pancreatitis. Br J Surg 101:1729–1738. doi:10.1002/bjs.9664
Tan V, Charachon A, Lescot T et al (2014) Endoscopic transgastric versus surgical necrosectomy in infected pancreatic necrosis. Clin Res Hepatol Gastroenterol 38:770–776. doi:10.1016/j.clinre.2014.06.016
Bausch D, Keck T (2013) Laparoscopic pancreatic resections. Langenbecks Arch Surg 398:939–945. doi:10.1007/s00423-013-1108-z
Kirkpatrick AW, Roberts DJ, De Waele J et al (2013) Intra-abdominal hypertension and the abdominal compartment syndrome: updated consensus definitions and clinical practice guidelines from the World Society of the Abdominal Compartment Syndrome. Intensive Care Med 39:1190–1206. doi:10.1007/s00134-013-2906-z
Boone B, Zureikat A, Hughes SJ et al (2013) Abdominal compartment syndrome is an early, lethal complication of acute pancreatitis. Am Surg 79:601–607
Mentula P, Leppäniemi A (2014) Position paper: timely interventions in severe acute pancreatitis are crucial for survival. World J Emerg Surg 9:15. doi:10.1186/1749-7922-9-15
Trikudanathan G, Vege SS (2014) Current concepts of the role of abdominal compartment syndrome in acute pancreatitis – an opportunity or merely an epiphenomenon. Pancreatol Off J Int Assoc Pancreatol IAP Al 14:238–243. doi:10.1016/j.pan.2014.06.002
van Brunschot S, Schut AJ, Bouwense SA et al (2014) Abdominal compartment syndrome in acute pancreatitis: a systematic review. Pancreas 43:665–674. doi:10.1097/MPA.0000000000000108
Anand RJ, Ivatury RR (2011) Surgical management of intra-abdominal hypertension and abdominal compartment syndrome. Am Surg 77(Suppl 1):S42–S45
Leppäniemi A (2009) Surgical management of abdominal compartment syndrome; indications and techniques. Scand J Trauma Resusc Emerg Med 17:17. doi:10.1186/1757-7241-17-17
Camps I, Arméstar F, Cuadrado M, Mesalles E (2009) VAC (vacuum-assisted closure) “covered” laparostomy to control abdominal compartmental syndrome in a case of emphysematous pancreatitis. Cir Esp 86:250–251. doi:10.1016/j.ciresp.2009.05.011
Hu HK, Du XJ, Li A, et al (2012) A minimally invasive management for abdominal compartment syndrome in severe acute pancreatitis. Pak J Med Sci. doi:10.12669/pjms.291.2721
Park S, Lee S, Lee HD et al (2014) Abdominal compartment syndrome in severe acute pancreatitis treated with percutaneous catheter drainage. Clin Endosc 47:469. doi:10.5946/ce.2014.47.5.469
Zhu H (2015) Embryonic natural orifice transluminal endoscopic surgery in the treatment of severe acute pancreatitis complicated by abdominal compartment syndrome. World J Emerg Med 6:23. doi:10.5847/wjem.j.1920-8642.2015.01.004
Radenkovic DV, Bajec D, Ivancevic N et al (2010) Decompressive laparotomy with temporary abdominal closure versus percutaneous puncture with placement of abdominal catheter in patients with abdominal compartment syndrome during acute pancreatitis: background and design of multicenter, randomised, controlled study. BMC Surg 10:22. doi:10.1186/1471-2482-10-22
De Waele JJ, Ejike JC, Leppäniemi A et al (2015) Intra-abdominal hypertension and abdominal compartment syndrome in pancreatitis, paediatrics, and trauma. Anaesthesiol Intensive Ther 47:219–227. doi:10.5603/AIT.a2015.0027
Pearl J, Price R, Richardson W, Fanelli R (2011) Guidelines for diagnosis, treatment, and use of laparoscopy for surgical problems during pregnancy. Surg Endosc 25:3479–3492. doi:10.1007/s00464-011-1927-3
Polydorou A, Karapanos K, Vezakis A et al (2012) A multimodal approach to acute biliary pancreatitis during pregnancy: a case series. Surg Laparosc Endosc Percutan Tech 22:429–432
Chan CHY, Enns RA (2012) ERCP in the management of choledocholithiasis in pregnancy. Curr Gastroenterol Rep 14:504–510. doi:10.1007/s11894-012-0294-0
Othman MO, Stone E, Hashimi M, Parasher G (2012) Conservative management of cholelithiasis and its complications in pregnancy is associated with recurrent symptoms and more emergency department visits. Gastrointest Endosc 76:564–569. doi:10.1016/j.gie.2012.04.475
Ducarme G, Maire F, Chatel P et al (2013) Acute pancreatitis during pregnancy: a review. J Perinatol 34:87–94
Veerappan A, Gawron AJ, Soper NJ, Keswani RN (2013) Delaying cholecystectomy for complicated gallstone disease in pregnancy is associated with recurrent postpartum symptoms. J Gastrointest Surg 17:1953–1959. doi:10.1007/s11605-013-2330-2
Qihui C, Xiping Z, Xianfeng D (2012) Clinical study on acute pancreatitis in pregnancy in 26 cases. Gastroenterol Res Pract 2012:1–5. doi:10.1155/2012/271925
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Campli, M., Cerioli, A., Leppäniemi, A., Arezzo, A., Bergamini, C. (2016). Acute Pancreatitis. In: Agresta, F., Campanile, F., Anania, G., Bergamini, C. (eds) Emergency Laparoscopy. Springer, Cham. https://doi.org/10.1007/978-3-319-29620-3_3
Download citation
DOI: https://doi.org/10.1007/978-3-319-29620-3_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-29618-0
Online ISBN: 978-3-319-29620-3
eBook Packages: MedicineMedicine (R0)