Abstract
Neurologists, neurosurgeons, ENT and maxillofacial surgeons, ophthalmologists, and others often detect cranial nerve deficits in their patients but remain uncertain about the underlying cause. It is the radiologist’s task to identify the causative disease, including inflammatory, infectious, vascular, traumatic, tumoral, and neurodegenerative etiologies. To detect this pathology, the neuroradiologist or head and neck radiologist must have a detailed knowledge of the anatomy of the 12 cranial nerves and available MR techniques. Furthermore, selecting the optimal sequences significantly depends on access to the patient’s history, clinical and biological data. In this chapter, emphasis will be put on employing the certain imaging techniques best suited to detect pathologies on the different parts/segments of the cranial nerves: intraaxial, extraaxial intracranial, skull base, and extracranial.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- Cranial nerves
- Cranial nerve diseases
- Cranial nerve disorders
- Cranial nerve tumours, benign
- Cranial nerve tumours, malignant
- Perineural tumour spread
- Cranial nerve injuries
- Cranial nerve V
- Cranial nerve VII
- Magnetic resonance imaging
- Computed tomography
-
To understand that lesions can be found on the different anatomical segments of the cranial nerves: intraaxial–extraaxial–skull base–extracranial.
-
To be aware that the MR technique must be adapted for each of these anatomical segments to detect all pathologies.
-
To be familiar with the imaging appearance of the most frequent cranial nerve pathologies.
-
MR anatomy, from brainstem nuclei to extracranial cranial nerve segments, is fundamental to identify disease.
-
Available clinical history, clinical presentation, and laboratory tests are crucial to make the correct diagnosis on imaging.
-
MRI is the preferred technique to detect CN disorders.
-
To be aware of the latest MRI techniques to visualize cranial nerve anatomy and pathology.
1 Introduction
The anatomy of the 12 paired cranial nerves (CNs) is complex and their origin, in the brain (CN I and II) or the brainstem (CN III–XII) as well as further intracranial and extracranial courses must be known. Moreover, it is technically challenging to cover the complete courses of the different CNs during imaging as well as to choose the right sequences on magnetic resonance imaging (MRI).
There are a wide variety of diseases that can cause cranial nerve (CN) disorders and imaging is needed to depict the causative pathology, for therapy planning and to assess response. The clinical examination, medical history, laboratory, and neurophysiological tests will all aid the radiologist to select the correct imaging modality or technique and use the best adapted protocol.
The first goal of CN imaging is to find the exact location of the disease: intraaxial (within the brain or the brainstem), extraaxial intracranial (outside the brain but inside the skull), skull base (in foramina, fissures, or canals of the skull base), extracranial (outside the skull). The tumoral, inflammatory, infectious, traumatic or dysfunctional disorders occurring along the different CN segments differ. Therefore, once imaging can link the lesion to one of these segments, a more precise and refined differential diagnosis is possible.
In this chapter, the most frequent pathologies involving the different CNs will be discussed [1,2,3,4,5,6,7,8] with emphasis on the MR techniques that should be used to visualize these lesions at the different CN segments.
2 Anatomy
In most anatomy and clinical papers, 12 pairs of CNs are mentioned; however, CNs I and II are extensions of the brain and are therefore not true CNs. This also explains why schwannomas do not occur along the olfactory tract and bulb or on the optic nerve. Hence, only 10 pairs of real CNs exist, and these nerves III–XII have their nuclei and origin in the brainstem.
Both the olfactory (CN I) and optic nerve (CN II) become discernible at the basal forebrain and leave the anterior cranial fossa through the cribriform plate and optic canal, respectively. The ten other CNs originate from the brainstem: the oculomotor (CNIII) and trochlear (CN IV) nerves exit from the midbrain, the trigeminal nerve (CN V) from the pons, while the abducens (CN VI), facial (CN VII), and cochleovestibular (CN VIII) nerves leave the brainstem at the medullopontine sulcus. The glossopharyngeal (CN IX), vagus (CN X), accessory (CN XI), and hypoglossal (CN XII) nerves become apparent at the level of the medulla oblongata. Nerve XII is present anterior to the olivary bodies at the pre-olivary sulcus while nerves IX–XI are posterior to the olivary bodies at the post-olivary sulcus. Cranial nerves III–VI pass through the foramina/fissures of the middle cranial fossa. Cranial nerves VII–XII leave the posterior cranial fossa through the internal auditory canal (CN VII–VIII), jugular foramen (CN IX–XI), and hypoglossal canal (CN XII).
Therefore, the location of the causative lesion, in the anterior fossa close to CN I–II, middle cranial fossa close to CN III–VI, or posterior cranial fossa close to CN VII–XII, will correlate with the presenting cranial nerve symptoms. Furthermore, lesions on distal extracranial branches most frequently will result in specific CN deficits, while proximal intracranial lesions (e.g. the brainstem) can result in deficits of multiple CNs in combination with other central neurological symptoms.
In practice, the optimal imaging techniques must be used to investigate CN impairments caused by (1) intraaxial lesions, affecting the CN nuclei and “fascicular segment” or segment of the nerve inside the brainstem, (2) extraaxial intracranial lesions compromising the cisternal CN fibres, (3) skull base lesions involving the CN segment at the skull base foramina/fissures and canals, and (4) extracranial lesions affecting the CN segments in the head and neck.
Knowing the complex CN anatomy and function is mandatory to study CN disorders in an adapted manner (Table 12.1). More anatomical and functional CN details can be found in CN textbooks [3,4,5,6].
3 Imaging Technique
3.1 Imaging Technique: General Considerations
Computed tomography (CT) is valuable in the detection of bone lesions and calcifications. Strengths of CT are that it is fast, immediately available and that monitored/unstable patients can be examined in a non-magnetic safe environment. Therefore, CT is often the first technique used in trauma patients, patients with inflammation or infection/abscess and in patients with compromised airways.
MRI provides superior tissue contrast to noise and is the method of choice to investigate CN disorders. As already mentioned, MRI protocols must be adapted to the regional CN anatomy, based on the available clinical information. This allows selection of the optimal adapted sequences and field of view for this anatomical region [2, 8]. The use of intravenous contrast media must be justified and will depend on the clinical presentation, the initial imaging findings, and the potential lesions on the differential (Table 12.2).
Evaluation of the size and density/signal intensity of CNs is easiest when the affected nerve can be compared with the normal contralateral CN. This is best achieved on coronal images for CNs I–VI as these nerves run in a postero-anterior direction. The axial plane is best suited for CNs VII–VIII as these nerves run in a slightly oblique axial plane in posteromedial to anterolateral direction.
In many cases, nerve enhancement is the only imaging finding in cranial nerve disorders and consequently the use of intravenous gadolinium (Gd) contrast enhancement is highly recommended in almost all cases.
Phased array head coils are anatomically suited to image the 12 CNs in their course down to the level of the mandible and hyoid. Study of the lower cranial nerves in the infrahyoid neck or upper mediastinum (CN X) requires the use of an additional dedicated neck coil.
3.2 Imaging Technique: New Techniques
Over the years, new MRI techniques have been developed and many of these have proven utility in clinical CN imaging.
High-angular resolution diffusion weighted imaging (at least 32 directions) allows cranial nerve tractography based on diffusion tensor imaging. Postprocessing however is crucial and routine software provided by MR vendors will in most cases be insufficient for cranial nerve tractography. Even with the best available techniques and postprocessing, currently only the larger isolated cranial nerves, II, III, V, VI, VII, and VIII can be adequately studied [9] (Fig. 12.1a). Apart from studying the course of the cranial nerves, for instance, the relation of the facial nerve to an VIIIth nerve schwannoma or parotid tumour, global tractography is also efficient in mapping cranial nerve ischaemia [10]. Future faster imaging acquisition techniques and more refined postprocessing software will further elevate this CN imaging technique in routine clinical practice [9, 11,12,13].
New imaging techniques for cranial nerves (CNs): (a) Tractography of CNs III (white arrow), V (grey arrow), VII and VIII (black arrow) in a normal volunteer (courtesy of Dr. T. Jacquesson and A. Attayé, CHU Grenoble, France). (b) Contrast-enhanced axial 3D black blood image showing enhancement of the optic nerve sheath in the posterior half of the orbit (arrows) in a patient with optic perineuritis. (c) Coronal 3D cranial nerve imaging (3D CRANI) showing the normal anatomy of the extracranial CNs: inferior alveolar nerve in the mandible (white arrow), distal end of the lingual nerve inside the anterior 2/3 of the tongue (grey arrow), vagus nerve (grey arrowhead), accessory nerve (black arrowhead), and hypoglossal nerve (black arrow)
In recent years, 3D black blood (BB) MRI is increasingly used in the neuroradiological and Head and Neck fields. The major advantage of this technique is that the vessels remain dark on the contrast-enhanced images and therefore do not mask pathology. The general background tissue also remains hypointense, and therefore the sequence is very sensitive for enhancement (Fig. 12.1b). Hence, enhancing cranial nerve lesions are easier to depict and can be distinguished from surrounding vessels. Furthermore, it is a 3D T1 weighted (T1W) TSE technique, resulting in almost no susceptibility artifacts, important at the level of the skull base. As it is a 3D sequence, excellent multiplanar reconstructions can be made in any desired plane.
MR neurography (MRN) techniques were further optimized during recent years. They use a contrast-enhanced black blood (BB) 3D STIR TSE sequence preceded by an MSDE (motion-sensitized driven equilibrium) pulse in combination with a pseudo-steady-state sweep and compressed sensing [14, 15]. Compressed sensing was needed to acquire these high-resolution isotropic images in an acceptable time. This technique is very sensitive to detect neuritis, neuropathy, nerve transection, etc. of the extracranial segments of the CNs, pathologies that were often not detectable with standard sequences [16]. Furthermore, this allows visualization of the extracranial segments of the CNs, down to the level of the hyoid and tongue (Fig. 12.1c) [17]; however, higher resolution sequences and improved neck coils that are available today will be needed to follow these nerves in the infrahyoid neck and upper mediastinum.
4 Cranial Nerve Lesions
4.1 Intraaxial Cranial Nerve Lesions
The nuclei and fascicular segment of the CNs III–XII are located in the brainstem. Involvement of these intraaxial CN structures will result in complex clinical presentations, consisting of multiple CN impairments, hemiplegia, hemiparesis, internuclear ophthalmoplegia, extrapyramidal syndrome, awareness impairment, nausea, etc. Cranial nerves I and II also have their “intraaxial” tract/cortical areas; therefore, lesions affecting these structures will result in cranial nerve I and II deficits.
Lesions in the brainstem are best studied with selective T2 weighted (T2W) and Proton Density (PD) images or mFFE/Merge/Medic images. These images should be 3 mm or less to avoid partial volume effects which can limit visualization of lesions. In the acute setting, diffusion weighted images (DWI) should be added to exclude recent infarctions and unenhanced T1 weighted images (T1WI), magnetic resonance angiography (MRA), and susceptibility weighted images (SWI) are useful in trauma patients and patients with vascular malformations or ischaemic lesions. Gd-enhanced T1WI should be added when tumour or infection is suspected.
Stroke and demyelinating disease are the most frequent intraaxial causes of CN involvement.
4.1.1 Ischaemic Stroke
Occlusion of the basilar artery, its perforating arteries, the distal portion of the vertebral arteries and the posterior-inferior cerebellar arteries can result in brainstem stroke and neurologic deficits with secondary CN disorders.
Unenhanced CT and T1W, T2* or SWI images can be used to exclude haemorrhage. DWI, T2 FLAIR images and perfusion MR or CT can be used to confirm the acute nature of the stroke (Fig. 12.2a) and to detect a penumbra, indicating that viable brainstem tissue around the irreversibly damaged ischaemic core can be saved by intravenous thrombolysis [18]. Mechanical thrombectomy for vertebral and basilar artery occlusions is a promising approach with initial studies demonstrating the potential of this intervention to benefit these patients. Finally, CT angiography and MR angiography (MRA) can be used to confirm vessel occlusion or stenosis.
Intraaxial lesions with CN disorders: (a) DWI image with acute infarct at the site of the left nucleus of CN IV and the left medial longitudinal fasciculus (MLF) causing a right superior oblique muscle palsy and internuclear ophthalmoplegia (INO). (b) MS patient with right trigeminal neuralgia with demyelinating lesions on the fascicular segment of the right trigeminal nerve (white arrow) and in the sensory and motor nucleus (black arrow) seen as hyperintensities on T2W imaging. (c) Neuroborreliosis rhombencephalitis with diffuse high signal intensity changes on T2W imaging in a patient presenting with falls and VIIIth nerve (vertigo) symptoms. (d) Covid-19 patient presenting with right Vth nerve neuropathy and neuralgia showing enhancement along the cisternal (arrow) and fascicular segment and in the brainstem nuclei on contrast-enhanced T1W (courtesy Dr. G. Hespel, AZ Zeno, Knokke-Heist, Belgium). (e) FLAIR image showing a low-grade glioma of the brainstem in a patient presenting with a right facial nerve palsy due to involvement of the right nucleus and fascicular segment of this nerve. (f) Contrast-enhanced T1W showing lymphoma in the right pons, cerebellopontine angle, and interna auditory canal in a patient presenting with deafness and dysequilibrium (CN VIII) and a grade 2 facial nerve palsy (VII) due to involvement of the nuclei, fascicular, and cisternal segments of these nerves
The nuclei of CN III, IV, VI reside in proximity of the medial longitudinal fasciculus and therefore in case of stroke, the resulting nerve deficit is most often associated with internuclear ophthalmoplegia (Fig. 12.2a).
4.1.2 Demyelinating Disease
Multiple sclerosis (MS), neuromyelitis optica spectrum disorders (NMOSD) with anti-MOG or anti-AQP4 antibodies, etc. are a heterogeneous group of inflammatory disorders [19]. Lesions located in the cranial nerve nuclei or fascicular segments of the cranial nerves will cause related CN symptoms. The trigeminal nerve is the most frequently involved CN and trigeminal neuralgia (TN) is the most frequent symptom (Fig. 12.2b). Patients with MS have a 20-fold increased risk in developing TN, and it affects 1.9–4.9% of MS patients. Conversely, MS is detected in 2–4% of patients with TN [20]. MS lesions are best seen on T2 weighted images (T2WI) or PD images, and the diagnosis is often already established clinically or confirmed by the typical supratentorial, infratentorial or medullary location, and morphology of the lesions.
Central pontine myelinolysis is another demyelinating disease mostly affecting the central pons and occurring primarily in alcoholic or malnourished patients complicated by hyponatraemia. The rapid correction of hyponatraemia has been recognized as the cause of the demyelination. Patients present with subacute progressive quadriparesis with lower cranial nerve involvement. It is usually fatal but can be mitigated by gradual correction of the electrolyte disturbance.
4.1.3 Trauma
High velocity trauma or trauma with a major impact on the brain can cause diffuse axonal injuries secondary to structural neural shearing. These focal lesions are hyperintense on T2WI, hypointense on T2* images or SWI and can be hyperintense on unenhanced T1WI in the acute phase and result in CN impairment when located in CN nuclei or the fascicular course. Acceleration–deceleration trauma can also result in injury of the posterior midbrain due to impact with the tentorium, causing oedema or superficial haemorrhage with consequent cranial nerve III or IV involvement.
4.1.4 Vascular Malformations
Cavernous haemangiomas are the most frequent vascular malformations found in the brainstem. They are best detected on T2* images or SWI and have a popcorn-like hyperintense centre on unenhanced T1WI which can slightly enhance after Gd administration. They can suddenly increase in size with spontaneous bleeding resulting in localized haemorrhage. This can then result in cranial nerve impairment, often improving and eventually resolving as the haemorrhage resorbs. Fistulas and arteriovenous malformations are less frequent causes.
4.1.5 Infectious Diseases
Listeria rhombencephalitis is caused by the Listeria monocytogenes anaerobic bacterium. This septicaemia occurs after oral contamination of infected fresh products. It is the most frequent cause of rhombencephalitis, and patients develop a spectrum of symptoms related to the brainstem involvement. Multiple cranial nerve palsies occur in 75% of the patients. The lesions are best seen on MR and are hyperintense on T2 and FLAIR (Fig. 12.2c) with linear CN enhancement and heterogeneous (diffuse inflammation) or ring enhancement (abscess) on the contrast-enhanced T1WI. The survival is only 50% and depends on the timely use of antibiotics. The presence of small foci of diffusion restriction indicates a worse outcome.
Some viruses like the cytomegalovirus can manifest in immunocompromised patients and cause encephalitis and involvement of the CN nuclei. Other viruses like the herpes simplex, herpes zoster and corona (COVID 19) virus can have a neurotropic behaviour. They can follow the cranial nerves into the brainstem where they follow the fascicular segment and even the course of the nuclei. High signal intensity can be seen on T2WI and FLAIR images along these structures and enhancement is possible on the contrast-enhanced T1WI (Fig. 12.2d).
4.1.6 Tumours
Midline infiltrating glioma of the pons and other tumours that can infiltrate the brainstem like metastases, CNS lymphoma, ependymomas, and medulloblastomas can all cause cranial nerve deficits, especially when growth is rapid. The lesions have a high signal intensity on T2WI and FLAIR images and heterogenous enhancement on post-contrast T1WI, except for lymphoma which has a homogeneous enhancement (Fig. 12.2e, d).
4.2 Intracranial Extraaxial Cranial Nerve Lesions
The intracranial extraaxial segment or cisternal segment of the cranial nerves course between the brainstem and the skull base neuroforamina and fissures. They are surrounded by cerebrospinal fluid (CSF), and therefore submillimetric heavily T2WI are optimal to demonstrate the nerves as grey/black surrounded by high signal intensity white CSF. Submillimetric 3D-DRIVE/FIESTA/SPACE T2WI can be used for this purpose but their range is limited, and thus difficult to cover the desired field of view. The 3D balanced-FFE sequence can acquire submillimetric isotropic images with a high resolution and a large range, covering all the CNs in an acceptable acquisition time. This sequence is however more sensitive to banding artifacts and motion. The banding artifacts result in black lines running through the high signal intensity fluid of the orbits, semicircular canals, cochlea, and CSF surrounding the olfactory bulbs. Hence, these peripheral regions and structures are better examined with 3D TSE T2W sequences. Another drawback of the 3D b-FFE sequence is that the pulsation of the basilar artery can cause dephasing or loss of the high signal intensity in the CSF surrounding this artery and in turn will frequently cause non-visualization of the abducens nerve. Visualization of this nerve can be accomplished with 3D TSE T2WI. A recent improvement of 3D b-FFE T2W sequence to 3D b-FFE XD T2W sequence eliminates these banding artifacts and therefore this new sequence can be used in all areas, including olfactory bulbs, inner ear, orbits, and for the abducens nerve. Gadolinium-enhanced T1WI or black blood (BB) images are used to detect abnormal nerve enhancement and are the most sensitive images to detect pathology on the cisternal segment. However, it should be cautioned that 3D T1W gradient-echo sequences are less sensitive to gadolinium enhancement and that subtle/weak enhancement can be missed on these images. TSE, SE and BB sequences, 3D or 2D, are more sensitive for gadolinium enhancement with the BB sequence being the most sensitive.
Intracranial extraaxial CN lesions like nerve sheath tumours and neuritis can involve the CN itself, or these CNs can be compressed/displaced by skull base, meningeal or vascular lesions as well as even normal vascular structures. The resulting CN symptoms and the patient’s history are helpful to localize and determine size of lesions. In the event of negative imaging studies, CSF sampling via lumbar puncture is needed to further evaluate these patients. CT can be used in the emergency setting to exclude intracranial hypertension prior to lumbar puncture and can also be used to exclude bone metastases. However, in most cases MR is needed to further characterize CN lesions [2, 8, 21, 22].
4.2.1 Tumours/Cysts/Cyst-Like Lesions
4.2.1.1 Nerve Sheath Tumours
Schwannomas are the most frequent CN tumours and develop from the Schwann sheath of these nerves. Schwannomas of CN I and II do not exist as they are extensions of the brain, thus do not possess Schwann cells. However, the nerve fibres that connect the olfactory bulb with the olfactory mucosa in the upper nasal meatus have Schwann cells along their course below the cribriform plate. Schwannomas developing at this site are called “olfactory schwannomas”, but they do not develop from CN I itself. Schwannomas can occur on all other cranial nerves and are most frequent on the vestibular branches of CN VIII and CN V. They are rare on the pure motor CNs IV, VI, XI (Fig. 12.3a). Schwannomas can be found in isolation or can involve multiple CNs. In the latter case, this is often in the context of Neurofibromatosis type 2 or schwannomatosis. The genes associated with these disorders are located on chromosome 22 but in schwannomatosis, there is incomplete penetrance with lower risk of its transmission to the offspring. Furthermore, these patients with schwannomatosis do not typically develop vestibular schwannomas [23]. Schwannomas are sharply delineated and have a homogeneous enhancement on contrast-enhanced T1WI. However, cystic degeneration and haemorrhage can occur when they become larger. The haemorrhages are best recognized on T2* images or SWI. The most frequent location of schwannomas is on the vestibular nerves, at the site of the ganglion of Scarpa. This ganglion can routinely be seen as a nodular thickening on the superior vestibular nerve on high-resolution T2WI at 3T MRI. However, it is impossible to tell whether a normal ganglion or a schwannoma is causing this nodular thickening and hence the use of gadolinium is crucial to exclude an early schwannoma at this site. Sometimes it is difficult to recognize in which direction CN VII is displaced by the cochleovestibular schwannoma and in these cases, CN tractography can provide this crucial information to the surgeon (Fig. 12.3b).
Intracranial extraaxial CN lesions: (a) Heavily T2W DRIVE image showing a schwannoma in the ambient cistern on the course of the IVth nerve (arrow) in a patient with left superior oblique muscle palsy. (b) High-angular resolution DWI tractography confirming anterior displacement of the facial nerve (arrows) by a cochleovestibular schwannoma. (c) Left temporal glioblastoma, with perineural tumour spread along the optic chiasm (white arrow) and intracranial optic nerves (black arrows). In the past, perineural extension was not typically seen in the context of glioblastoma as survival was very short, however, is now increasingly depicted as novel therapies result in longer survival. (d) Axial contrast-enhanced T1W showing a recurrent sarcoid carcinomatous tumour of the left maxillary sinus with extension along the maxillary nerve in the parasellar region and into the brainstem (white arrowheads), also involving the cisternal segment of the trigeminal nerve (grey arrowhead) in a patient presenting with left CN V neuropathy and acute right hemiparesis. (e) Coronal T2 weighted DRIVE images showing lower signal intensity inside an epidermoid tumour in the left cerebellopontine angle compared with CSF. The patient presented with trigeminal neuropathy with the cisternal segment of the left trigeminal nerve laterally displaced and flattened (black arrow) compared to the normal contralateral nerve (white arrow). (f) Axial contrast-enhanced T1W in a patient presenting with multiple bilateral CN deficits. Enhancement of the lower cranial nerves on the right side (arrowhead) and multiple other CNs (not shown) was seen and were associated with leptomeningeal enhancement around the brainstem (arrows), pathognomonic for sarcoidosis. (g) Patient presenting with diplopia and ptosis following a trauma. Coronal contrast-enhanced T1W shows enhancement of the cisternal segment of the right oculomotor nerve 1 month after the trauma, representing post-traumatic enhancement caused by contusion and/or elongation of the nerve. (Courtesy Dr. D. Vanneste, Hospital Geel-Mol, Belgium)
Neurofibromas are less frequent encapsulated nerve sheath tumours. The major difference on imaging is that instead of a rounded morphology, they typically appear elongated in appearance, following the course of the nerves, and show no or only weak gadolinium enhancement. These nerve sheath tumours must be distinguished from other tumours. When solitary they must be differentiated from neuromas, which develop on the CNs secondary to a trauma or insult, and haemangiomas [21, 22, 24].
The most frequent causes of bilateral enhancement of multiple CNs are metastasis, lymphoma, and leukaemia. Unfortunately, they have overlapping imaging characteristics and thus, the clinical history, CSF sampling, biochemistry, further whole-body imaging and pathology are typically needed to narrow the diagnosis. Also, metastases from primary brain neoplasms like glioblastoma (Fig. 12.3c), medulloblastoma, ependymoma, and germinoma can be found on the CNs and finally perineural spread of head and neck tumours can reach the cisternal segment of the cranial nerves and can eventually reach the brainstem (Fig. 12.3d).
4.2.1.2 Meningiomas
Meningiomas are common tumours, can be isolated or multiple, and can displace and even follow CNs. They are isointense with grey matter on all MRI sequences and enhance homogeneously, and classically often have a dural tail enhancement. Olfactory groove meningiomas can cause olfactory symptoms like anosmia. Meningiomas of the planum sphenoidale frequently reach the optic nerves and can even follow these nerves in the optical canal and orbit, with visual impairment and potential eventual blindness as a result. Therefore, early diagnosis and treatment of meningiomas at this location is crucial. At the level of the internal auditory canal (IAC) and cerebellopontine angle (CPA), meningioma is the most common differential diagnosis for schwannoma. CT can help in the differential diagnosis by demonstrating the presence of calcifications and hyperostosis of the adjacent bone and even pneumosinus dilatans of the adjacent sinuses in the context of meningiomas, while schwannomas typically displace adjacent bone. On MRI, meningiomas can be distinguished from nerve sheath tumours due to broad base contact with the meninges, a course along the walls of the IAC rather than the nerves in the centre, and often a lateral border in the IAC running perpendicular to the VIIIth nerve, while schwannomas follow the course of the nerve. Petro clival meningiomas and posterior fossa meningiomas can also cause trigeminal and lower cranial nerve symptoms, and these meningiomas can also follow CN V3 and CNs IX, X, XI outside the skull although this occurs less frequent than for CN II.
4.2.1.3 Other Tumours, Cysts/Cyst-Like Lesions
Epidermoid cysts are well-defined lesions with inclusion of ectodermal epithelial elements, they can be thought of as “skin in the wrong place”. They are often an incidental finding but can cause CN symptoms when they become large. They are isodense with CSF on CT and isointense with CSF on most MR sequences and do not enhance. However, they have a typical hyperintensity on b-1000 DWI images and show diffusion restriction on the apparent diffusion coefficient (ADC) map. Submillimetric heavily T2W 3D gradient-echo images (e.g. balanced-FFE) are ideally suited to make the diagnosis and evaluate the exact extension of the lesions. On these images, the epidermoid has a low signal intensity and can easily be distinguished from CSF (Fig. 12.3e), which is not the case on heavily T2W TSE images. Treatment consists of surgical decompression.
Subarachnoid CSF encapsulation or cyst formation can also cause displacement of or compression on CNs. They are isointense to CSF on all sequences, including DWI and 3D T2W GE sequences. On heavily T2W 3D sequences, the typically thin wall of the cyst can be demonstrated, confirming the diagnosis, and resolving the cyst dimensions. Surgical cyst fenestration is performed in cases of causative CN or other neurological symptoms.
Pituitary adenomas and craniopharyngiomas can compress the optic chiasm and cause bitemporal hemianopsia. Rathke cleft cysts are most often an incidental finding but may rarely cause vision loss.
Pineal tumours and cysts can cause compression on the dorsal midbrain with a Parinaud syndrome as consequence. The syndrome consists of upgaze palsy, convergence retraction nystagmus, and pupillary hyporeflexia.
Dermoid cysts, lipomas, and neurenteric cysts less frequently cause CN disorders, but surgical decompression or partial resection can be considered for symptom management.
4.2.2 Vascular Diseases
The cisternal segment of the CNs pass through the CSF spaces around the brainstem, where they are in the close vicinity of the posterior circulation vessels, with a potential nerve–vessel conflict (NVC) as a result.
4.2.2.1 Neurovascular Compression Syndromes
Arteries and veins can directly compress and displace the cisternal segment of the CNs, resulting in a neurovascular compression syndrome (NVCS). Arteries elongate and become more tortuous as patients get older and this can increase compression. The relation between the anatomical NVC and the resulting NVCS is most reliable for conflicts with CN V—resulting in trigeminal neuralgia, CN VII—causing hemifacial spasm, CN VIII—provoking vestibular paroxysmia, and CN IX—generating glossopharyngeal neuralgia. Indeed, only a minority of neurovascular contacts are symptomatic and therefore the relationship with patients’ symptoms remains controversial. The challenge is to recognize which NVC could be symptomatic and in this context, four characteristics of the NVC should be considered. First, the NVC should be at the short 1–2 mm long vulnerable transition zone between the central myelin that originates from oligodendrocytes and covers the proximal intracisternal portion of the CN and the more distal peripheral myelin from Schwann cells. These transition zones are located 4 mm, 2 mm, 10 mm, and less than 2 mm distal to the location where CN V, CN VII, CN VIII, and CN IX leave the brainstem, respectively [25]. Second, venous conflicts exist but arterial conflicts result more frequently in a NVCS. Third, conflicting arteries crossing the CNs in a perpendicular fashion are more prone to provoke a NVCS. Fourth, displacement of the involved CN is probably the most important predictor of a clinically significant NVC.
MR is the method of choice to demonstrate these conflicts and unenhanced 3D TOF MRA images can visualize the arteries, heavily T2W TSE or GE images can demonstrate the nerves and post-contrast submillimetric 3D T1WI are able to depict the veins. Hence, all involved anatomical structures are visualized and fusion software with selective colour coding for each anatomical structure makes the diagnosis easier, especially after decompression surgery when a recurrent NVCS is suspected and the position of the interposed surgical material (e.g. Teflon) must be assessed.
4.2.2.2 Aneurysm and Arterial Dissection
In patients presenting with painful unilateral CNs, aneurysm and arterial dissection should be considered. Aneurysms on the medial wall of the internal carotid siphon, on the posterior communicating artery and proximal part of the posterior cerebral artery can push on the superior to superomedial border of the oculomotor nerve (CN III), resulting in complete intrinsic and extrinsic oculomotor nerve palsy. Pupillary function loss is seen in 14% of these patients and is explained by compression on the preganglionic parasympathetic pupillomotor fibres to the ciliary ganglion which are located on the superior medial surface of CN III. However, CN III palsy is in most cases limited to extrinsic oculomotor function which is caused by ischaemia of the central motor fibres. This is also the mechanism leading to diabetic ophthalmoparesis, counting for 25% of all ocular motor nerve palsies. Imaging remains negative in these cases and should therefore be judicious when the clinical context is obvious [26].
CTA and MRA are both able to visualize aneurysms and arterial dissections and FS T1W TSE images can also detect the high signal intensity of methaemoglobin in the wall of the artery in case of dissection. Black blood images with and without gadolinium are also very sensitive.
4.2.3 Infectious Diseases
Viral neuritis with enhancement of the cisternal segment of the CNs is most frequently seen along the cisternal segment of CN II, III, V, VI and is best depicted on contrast-enhanced coronal high-resolution T1WI. The enhancement of the cisternal segment of CN VII in case of Bell’s palsy is limited to the fundus of the IAC and is best seen on axial post-contrast T1WI. Additionally, in these patients the CSF around the facial nerve at the fundus of the IAC disappears, and this area becomes hypointense and blunted. However, the most important enhancement can be seen inside the facial nerve canal, and this will be discussed in Sect. 12.4.3 on the “skull base” segment/course of the CNs.
The main differential diagnosis is varicella zoster virus infection affecting the sensory fibres of both the cochleovestibular nerve and facial nerve causing sensorineural hearing loss and facial palsy. This is accompanied clinically by an external vesicular rash with burning ear pain, fever, vertigo, and nausea and is called “Ramsey Hunt syndrome”. The role of MR is to demonstrate CN VII and CN VIII enhancement in the fundus of the IAC to confirm the diagnosis, especially when the CN symptoms precede the other clinical symptoms, and the diagnosis is still uncertain.
As already mentioned, neurotropic viruses like herpes zoster and corona virus (COVID-19) can follow the cisternal segment of the CNs into the brainstem and even brainstem nuclei.
CN disorders may be the first signs of underlying meningeal disease. Often multiple CNs are involved on both sides, but it can also be an isolated nerve, for example, non-specific abducens palsy (CN VI). The meningeal enhancement is difficult to detect on 3D T1WI as all meninges show enhancement even in normal patients and is even more difficult to see on post-contrast CT. 3D FLAIR is more sensitive but today post-contrast 3D BB imaging is the sequence of choice. In normal patients, no meningeal enhancement is seen on these images, making it easy to identify abnormal meningeal enhancement in the case of meningitis. In leptomeningitis, the leptomeninges, on the surface of the brain and the brainstem, are thickened and enhancing. In pachymeningitis, the thickened enhancing meninges are contiguous to the skull. Pyogenes and tuberculous meningitis are two common causes of the brainstem and skull base leptomeningitis.
4.2.4 Non-infectious Inflammatory Diseases
Neurosarcoidosis is the most common cause of non-infectious leptomeningitis leading to CN disorders. All CNs can be involved but the most frequent affected nerve is the facial nerve, which can even be involved bilaterally. As mentioned, leptomeningeal enhancement is best detected on post-contrast 3D FLAIR and 3D BB images (Fig. 12.3f). Additionally, diabetes insipidus also causes thickening of the pituitary stalk and disappearance of the high signal intensity spot in the neurohypophysis. Non-infectious leptomeningitis can also be seen in Granulomatosis with Polyangiitis (PGA), formerly Wegener’s disease, and in Langerhans cell and non-Langerhans cell histiocytosis.
4.2.5 Trauma
The most frequently involved CN in trauma is CN I. Anosmia can occur after a frontal or occipital trauma or acceleration-deceleration trauma with contusion of the olfactory bulbs, best seen on coronal T2W TSE images, and olfactory fibre shearing at the level of the cribriform plate. Acceleration-deceleration trauma can also result in a fracture of a CN. The CNs with the longest cisternal segment, for example, CN IV, and those with a vulnerable anatomical location, for example, CN VI with a long course between pons and clivus, are most prone to injury. A fracture of the cisternal segment of a CN can be seen on submillimetric heavily T2W TSE images and sequelae of elongation of the CNs can sometimes be seen in the acute and subacute phase as CN enhancement on the coronal and/or axial contrast-enhanced T1WI (Fig. 12.3g). Further post-traumatic oedema of the brain can result in brain herniation and secondary CN disorders. CN III and CN IV can be involved in cases of transtentorial herniation of the internal temporal gyrus. The lower CNs IX–XI and CN XII can be involved in case of herniation of the cerebellar tonsils through the foramen magnum.
Repetitive trauma with bleeding can also result in meningeal superficial siderosis. This haemosiderin deposition occurs also on the CNs and can result in degeneration and disorders of the involved CN. CN VIII is most frequently involved with resulting sensorineural hearing loss. The haemosiderin deposit can be seen as a hypointense rim around the CN on T2* images or SWI and atrophy can be visualized on submillimetric heavily T2WI (e.g. DRIVE, b-FFE). Similar siderosis can also be caused by haemorrhagic surgery, subarachnoid haemorrhage, slow growing tumours and in cerebral amyloid angiopathy.
4.3 Skull Base Cranial Nerve Lesions
The CNs must pass through the skull base once they leave the intracranial CSF spaces. They can achieve this by running through foramina, fissures and canals, routes which are also used by traversing arteries and veins. In the parasellar region, CNs even first course through a venous space, the cavernous sinus, before traversing the skull base. These foramina, fissures and canals can be visualized on CT but the nerves, except for the olfactory bulb and optic nerve, cannot be visualized. Widening of the foramina, canals, and fissures or bone destruction are an indirect sign of CN involvement or pathology. MR is better suited to visualize the cranial nerves themselves in the foramina, fissures, and canals. They are visible on unenhanced T1WI with surrounding fat or fatty marrow in bone. However, many of the nerves and especially those running in the cavernous sinus, can only be depicted as dark spots surrounded by hyperintense enhancing veins on contrast-enhanced T1W images. Therefore, high-resolution imaging is critical to visualize many of these small CNs or CN branches. Contrast-enhanced 3D BB images are very sensitive for the detection of CN nerve enhancement in foramina, fissures, and nerve canals. Alternatively contrast-enhanced 3D T1WI (e.g. thrive, vibe, SPGR) with fat suppression can be used.
Lesions involving the optic canal, facial nerve canal, and hypoglossal canal will result in isolated disorders of CN II, CN VII, and CN XII. However, pathology at the level of the superior orbital fissure and cavernous sinus can affect multiple CNs (CNIII, IV, V, and VI), and the same is true for jugular foramen lesions that result in combined CN IX, X, and XI disorders.
Most of the causes that affect the intracranial extraaxial CN segments can also affect the skull base segments. To avoid repetition, the focus in this chapter will be on pathology specific to the skull base and the CNs at this site.
4.3.1 Trauma
CNs are very vulnerable for trauma in their course through the skull base. Sharp fracture edges, loose bone fragments, and bullet fragments in case of a gunshot trauma can damage the nerves inside their foramen, fissure, or canal. CN II inside the optic canal is most frequently involved followed by CN VII in the facial nerve canal, CN XII in the hypoglossal canal, and the lower cranial nerves at the level of the jugular foramen. CT with bone window setting is employed to detect fractures and demonstrate potential nerve conflicts, but only MR can confirm injury to the nerves themselves.
Acute and subacute contusion of the optic nerve can result in high signal intensity of the nerve on STIR or 3D FLAIR images and can show contrast enhancement on 3D BB images, while contrast-enhanced 3D T1WI is less sensitive. The smaller the calibre of the CNs, the more difficult it will become to see these relevant signal changes.
The tympanic segment and geniculate ganglion fossa are the most frequently fractured parts of the facial nerve canal. However, the nerve can also be contused without associated fracture, and this will cause swelling of the nerve. When this occurs in the labyrinthine segment of the facial nerve, where the nerve occupies 95% of the space inside the canal, nerve ischaemia, and necrosis can occur as the swollen nerve can completely occlude feeding vessels at this site. This can be detected as enhancement of the labyrinthine segment on 3D BB or 2D/3D T1WI in the acute and subacute phase. Depending on the severity and evolution of the facial nerve palsy as well as experience of the surgeon, nerve decompression at the labyrinthine segment can be considered a safe and effective management approach.
4.3.2 Neuritis
Peripheral facial nerve palsy or Bell’s palsy, caused by the herpes simplex virus, is one of the most frequent reasons to perform CN imaging. In most cases, the palsy spontaneously disappears in less than 2 months. Imaging is requested when the Bell’s palsy persists, recurs or in cases of atypical clinical presentation. Imaging can confirm the diagnosis when gadolinium enhancement is seen along the facial nerve at the fundus of the IAC or along the labyrinthine segment on thin post-contrast T1WI and 3D-FLAIR images. Enhancement at these locations is always abnormal. Enhancement of the geniculate ganglion, tympanic and mastoid segment of the facial nerve are unreliable as these nerve segments are surrounded by veins and arteries which of course also enhance in normal circumstances. This can be solved by using contrast-enhanced submillimetric 3D BB sequence as flow and enhancement inside the vessels are suppressed on these images, showing selectively the nerve enhancement in the geniculate ganglion, tympanic and mastoid nerve segments as well (Fig. 12.4a–c). Comparison with the contralateral nerve facilitates the diagnosis [5, 27, 28]. Neuritis with nodular enhancement in the geniculate ganglion must be differentiated from a facial nerve schwannoma and haemangioma. On CT, schwannomas enlarge the geniculate fossa while in haemangiomas, honeycomb calcifications are seen in the centre of the fossa. In cases of neuritis, the geniculate fossa retains its normal anatomical shape without any central calcifications.
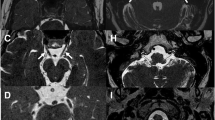
Skull base CN lesions: (a–c) Patient presenting with right Bell’s palsy assessed with contrast-enhanced 3D BB images. (a) Abnormal nerve enhancement can be seen at the fundus of the internal auditory canal, labyrinthine segment, and geniculate ganglion (white arrows). The normal tympanic segment of the left facial nerve is not enhancing and no vascular enhancement is seen on this axial BB image (grey arrow). (b) At a slightly lower level, the enhancing tympanic segment of the right CN VII is seen while the normal posterior part of the tympanic segment on the left side is not enhancing (arrows). (c) Reconstruction of the enhancing abnormal labyrinthine (white arrowhead), tympanic (grey arrowhead), and mastoid (black arrowhead) segment of the right facial nerve. (d, e) Chondrosarcoma of the petro-occipital fissure in a patient presenting with vertigo and lower cranial nerve deficits on the right side. Coronal (d) and axial (e) contrast-enhanced 3D BB images showing the enhancing mass with extension in the internal auditory canal (black arrows) and in the jugular foramen (white arrows). (f, g) Patient presenting with suspected Tolosa-Hunt syndrome but eventually diagnosed having IgG4 disease. Pre-therapy (f) and post-therapy (g) contrast-enhanced coronal high resolution T1W images. At presentation, the cavernous sinus was thickened and nerves V1 and V2 could no longer be distinguished (black arrowhead). Complete recovery after 4 weeks of steroid treatment with reappearance of the ophthalmic nerve (white arrowhead) and maxillary nerve (grey arrowhead)
Neuritis of CNs III, IV, VI, and V1 in the cavernous sinus are best seen on contrast-enhanced high-resolution coronal submillimetric T1WI. The in-plane resolution of these 2D images must be very high to identify these small nerves in the parasellar area. In this context, the slice thickness must be at least under 3 mm, without gap between the slices. Optimal visualization of these nerves and their enhancement, in cases of neuritis, is more confidently identified once the slice thickness is lower than 2.5 mm.
4.3.3 Skull Base Infections and Tumours
Unilateral involvement of several CNs is suggestive of skull base disease. CT and contrast-enhanced MR together with the clinical history and laboratory data are used to obtain the correct diagnosis. In case of osteomyelitis, the infectious cause must be sought in the paranasal sinuses, middle ear and/or mastoids with different CNs affected, depending on where the infection is located. Cranial nerve VI runs in Dorello’s canal passing through the venous basilar plexus behind the clivus. Aggressive fungal infections originating in the sphenoid sinus can destroy the posterior wall of the sinus and enter this plexus, thus provoking a unilateral abducens palsy. In this case, CN VI will enhance and no longer be visible as a black dot inside the enhancing basilar plexus on axial high-resolution post-contrast T1WI.
Skull base tumours can displace, compress, or encase CNs with fibrous dysplasia, chordoma, chondrosarcoma (Fig. 12.4d, e), and metastasis as the most frequent etiologies. A combination of T2W, unenhanced and contrast-enhanced T1W and DWI sequences help in the characterization of these lesions. Detailed anatomical delineation of the tumour is best obtained on contrast-enhanced 3D images and 3D T1W BB images, reconstructed in the axial, coronal, and sagittal planes.
Meningiomas can follow the CNs in their course through the skull base. They most frequently follow CN II, CN V3, and CN IX–XII. Most of these meningiomas originate in the posterior fossa and then follow the nerves more peripherally. Rarely, these neoplasms develop in the jugular foramen itself and additionally, are then difficult to distinguish from other calcified tumours like chondrosarcomas. The isointensity with grey matter, homogeneous enhancement, intact cortex of the jugular foramen walls, and dural tail enhancement all aid to facilitate the correct diagnosis.
Nonetheless, the most frequent lesions found in the jugular foramen are schwannomas of the lower CNs and paragangliomas with both presenting with dysfunction of the lower CNs [29]. Distinguishing between these on CT relies on the fact that schwannomas enlarge the foramen with intact cortical walls, while paragangliomas permeate into the bone and result in a moth-eaten appearance. Unenhanced MRA will show the feeding vessels inside the paragangliomas as high signal intensity spots, and these are absent in case of a schwannoma. Furthermore, a salt (hyperintensities on T1) and pepper (hypointensities on T2) appearance is characteristic for a paraganglioma.
Metastases can be found anywhere in the skull base and can cause CN dysfunction. A common location is the hypoglossal canal and the most frequent diagnosis in case of an isolated hypoglossal nerve palsy is a skull base metastasis.
4.3.4 Cavernous Sinus
Cranial nerves III, IV, and V1 are located in the wall of the cavernous sinus and CN VI is located deeper inside the cavernous sinus. Hence enhancing schwannomas and neuritis of these nerves can be found in the cavernous sinus. In this anatomical region, schwannomas most frequently involve the trigeminal nerve. Schwannomas in Meckel’s cave can become quite large and will then also extend towards the posterior fossa, giving them a classic dumbbell appearance. Schwannomas on the maxillary and mandibular nerves will eventually enlarge the round and oval foramen, respectively. Perineural tumour spread along the CNs and metastases in the cavernous sinus are important differential diagnoses when enhancing lesions or nerves are identified in this location.
Aneurysms of the parasellar ICA can also be responsible for palsies of CNs III, IV, V1, and VI. However, due to its location deep in the cavernous sinus, the abducens nerve is often the first to be affected by these aneurysms. The same is true for pituitary adenomas and craniopharyngiomas that extend in the parasellar region. Although the overall most frequently involved CN inside the cavernous sinus, regardless of the cause, is CN III followed by CN VI.
Idiopathic non-neoplastic non-infectious granulomatous inflammation of the cavernous sinus and orbital apex is called “Tolosa-Hunt Syndrome”. The patients present with periorbital and frontal pain and CNs II, III, IV, V1, and VI, can be involved. Several days of headache are followed by diplopia and ptosis, almost always unilateral. On contrast-enhanced coronal T1WI, strong enhancement of all structures inside the cavernous sinus including all CNs, and lateral bulging of the enlarged cavernous sinus, can be seen. The headache disappears typically over the course of days and the ophthalmoplegia within 2 weeks following corticosteroid treatment. Follow-up MR at 6 months will demonstrate a complete normalization of the cavernous sinus, confirming the diagnosis [30].
IgG4 is a rare autoimmune disease which can also involve the cavernous sinus and its cranial nerves in a similar way as Tolosa-Hunt syndrome (Fig. 12.4f, g). The combination with bilateral lacrimal gland, CN and especially infraorbital nerve, pituitary infundibulum, and salivary gland involvement leads to a preferred diagnosis of IgG4 [31].
4.4 Extracranial Cranial Nerve Lesions
Primary extracranial CN diseases are rare and most of the extracranial CN disorders are caused by lesions of the surrounding structures that may insult the nerves. Most often, the symptoms are unilateral.
CN I dysfunction caused by ethmoidal and nasal lesions will result in anosmia.
Orbital diseases can cause partial or complete monocular visual loss when the optic nerve (CN II) is involved. CN III, IV, and VI dysfunctions will lead to diplopia. Miosis and mydriasis occur when the inferior branch of CN III and its side branch with the ciliary ganglion are affected at the orbital apex.
Facial lesions can result in CN V neuropathy with unilateral hypoesthesia, numbness, or burning pain when extracranial branches of the trigeminal nerve are involved. These symptoms can be restricted to the territory of one branch, V1, V2, or V3, depending on the location of the lesions. Numbness, motor weakness, and progressive CN V symptoms are the most reliable clinical signs of a trigeminal lesion and frequently correlate with positive imaging findings; however, the more frequent non-specific facial pain usually does not have a culprit-associated lesion.
Isolated peripheral CN VII dysfunction, with intact lacrimal function and stapes reflex and taste in the anterior 2/3 of the tongue, may be provoked by parotid and peri mastoid lesions.
At the suprahyoid level, CNs IX–X course next to each other and are often injured together. Patients can then present with dysphagia, uvula deviation, absent gag reflex, hoarseness, vocal cord palsy, loss of taste to the posterior 1/3 of the tongue, otalgia, and tachy- or bradycardia. Inability to raise the arm and a shoulder drop indicate a CN XI palsy. Deviation of the tongue to the side of the lesion and tongue muscle atrophy are the signs of a CN XII palsy.
Only CN X continues at the infrahyoid level, and when injured at this level, endolaryngeal symptoms (hoarseness, vocal cord palsy, and taste loss in posterior 1/3 of the tongue) is found.
Muscle atrophy or dystrophy are helpful signs on imaging to confirm injury to motor CNs and should always be verified [32].
The method of choice to study extracranial nerves is MRI. For many years, high-resolution T2W, unenhanced T1W and fat-saturated Gd-enhanced T1W images were the primary sequences to visualize the extracranial nerves and to characterize associated lesions. Later, diffusion and perfusion MRI further advanced characterization of these lesions. However, many of the nerve branches and associated pathology remained below the limits of resolution. In recent years, MRN was optimized for CN imaging and slightly different techniques are used for MR systems of different vendors [14,15,16,17, 33]. This technique was described above in Sect. 12.3.2. In the infrahyoid neck, only part of the vagus nerve can be visualized with this technique. Yet CN X continues into the thorax and lesions along the course of the recurrent laryngeal branches, down to the clavicle on the right and down to the aorta-pulmonary window on the left. At this level, CT is the modality of choice as the neck and thorax can be studied together in a fast single scan with better visualization at the thoracic level in comparison with MR.
It is beyond the current scope to cover all extracranial pathology that can cause CN dysfunction, only the most frequent and important causes are highlighted.
4.4.1 Vascular Lesions
In the orbit, CN II dysfunction can be caused by cavernous haemangiomas and venous varices. Cavernous haemangiomas are round to ovoid sharply delineated homogeneous enhancing lesions that can compress the optic nerve. Venous varices can enhance, demonstrate flow voids as well as increase in size with prone positioning.
Cranial nerve IX–XII dysfunction can be caused by ICA dissection or aneurysm resulting in compression of the cranial nerves inside the carotid space. Damage of the lower CNs can also be iatrogenic during endarterectomy.
Finally, aortic arch aneurysms can narrow the aortic-pulmonic window with compression on the recurrent laryngeal nerve resulting in left vocal cord palsy [33].
4.4.2 Infectious Diseases
Aggressive bacterial and fungal infections of the sinuses and temporal bone can lead to extracranial CN involvement. Fungal infections can be recognized by their low signal intensity on T2WI while abscess formation in aggressive bacterial infections shows diffusion restriction on DWI. Aspergillus and especially mucormycosis can destroy the sinus walls thereby directly affecting the adjacent cranial nerves. Vulnerable locations are the frontal sinus (for CN V1), ethmoid and sphenoid sinus (CN II, III, IV, V1, V2, VI in the orbital apex and superior orbital fissure), and temporal bone (CN VII). MRI can visualize the thickened and enhancing cranial nerves while both CT and MRI can demonstrate late-stage infection surrounding and eventually encasing involved CNs.
Dental periapical and periodontal disease of the upper and lower jaw can result in V2 and V3 neuropathy, respectively. The resulting CN changes, oedema-demyelination-Wallerian degeneration, can only be visualized with new MRN techniques like 3D-CRANI and optimized 3D-FISP sequence. On these post-contrast images, the nerves are thickened, irregular, and have a high signal intensity compared to the normal contralateral nerves [15,16,17, 33]. These neuropathies could not be confirmed or visualized before the advent of these new MRN techniques and thus facilitates timely use of appropriate therapies (Fig. 12.5a).
Extracranial CN lesions: (a) Coronal contrast-enhanced 3D CRANI sequence with paracoronal MIP reconstruction in a patient presenting with numbness of the left chin and dysesthesia in the left inferior alveolar nerve territory following osteomyelitis of the left mandible. The left inferior alveolar nerve is thickened, irregular and hyperintense (arrow), compatible with neuropathy. (b, c) Contrast-enhanced 3D CRANI with coronal MIP reconstruction (b) and 3D MIP reconstruction with lateral view (c) in a patient with right Bell’s palsy. The hyperintense and thickened nerve branching inside the right parotid gland can be seen (black arrow) and even the peripheral hyperintense zygomatic branch (grey arrowhead), buccal branches (black arrowheads), mandibular branch (white arrowhead) and cervical branch (grey arrow) can be followed. (d, e) Axial (d) and paracoronal (e) contrast-enhanced 3D BB images of a left optic nerve meningioma. The tram track sign can be followed in detail from intracranial to the distal part of the left optic nerve. The coronal reconstruction shows that the meningioma surrounds the optic nerve over 270° (arrows)
Malignant otitis externa, a pseudomonas aeruginosa infection affecting immunocompromised or diabetic patients, can lead to CN VII dysfunction.
Osteomyelitis (Fig. 12.5a) and osteoradionecrosis can cause dysfunction of the lower CNs IX–XII at the level of the skull base and can irritate the inferior alveolar nerve, with resulting pain and numbness, at the level of the mandible. Both pathologies cause loss of the high signal intensity of the bone marrow on unenhanced T1WI and show bone marrow enhancement on the post-contrast T1WI. CT is best suited to distinguish both entities and can demonstrate the characteristic bone sequestration, lytic defects in the cortical bone and periosteal new bone formation in case of osteomyelitis. The resulting CN changes are in most cases only recognizable on MRN images.
Viral neuritis of extracranial CNs or of their branches was not resolvable on MR even a couple of years ago. Today, the new MRN sequences allow the visualization of the inflamed distal CN branches of the facial and trigeminal nerve (Fig. 12.5b, c).
4.4.3 Non-infectious Inflammatory Diseases
4.4.3.1 Demyelinating Diseases
Spontaneous vision loss in young and middle-aged adults is often due to optic neuritis, frequently in the context of multiple sclerosis (MS) and neuromyelitis optica spectrum disorders (NMOSD) with anti-AQP4 or anti-MOG antibodies. The optic nerve lesions are best identified on 3D FLAIR and T2 STIR images. In most cases, post-contrast T1WI are negative and when contrast is used the more sensitive 3D BB sequence should be used. MR imaging of the brain and spine can be used to confirm the diagnosis of MS and to distinguish the demyelinating disease subtypes [19]:
4.4.3.2 MS
-
(a)
Unilateral optic neuritis, short segment involving the middle portion of the nerve.
-
(b)
Scattered demyelinating lesions in the brain.
-
(c)
Lesions in the upper half of the spinal cord, lesions are shorter than two vertebral levels and involve less than 50% of the cord diameter.
4.4.3.3 Anti-AQP4+
-
(a)
Bilateral optic neuritis, long segment involving the posterior portion of the nerves with chiasmatic extension.
-
(b)
Predominantly periventricular demyelinating lesions.
-
(c)
Lesions in the upper half of the spinal cord, extending over more than three vertebral levels and more than 50% of the cord diameter.
4.4.3.4 Anti-MOG+
-
(a)
Bilateral optic neuritis, long segment involving the anterior portion of the nerves.
-
(b)
Brain lesions more frequently found in the basal ganglia, thalamus, and pons.
-
(c)
Lesions located in the lower half of the spinal cord, extending over more than three vertebral levels and more than 50% of the cord diameter.
Vision loss with optic nerve signal changes on MR can also be seen in case of inflammatory neuritis or ischaemia. The above-mentioned associated brain and spinal cord changes can help to distinguish these etiologies from demyelinating disease. The clinical history, biochemical data and follow-up are needed to distinguish the three entities when the brain and spine imaging are normal.
4.4.3.5 Granulomatous Diseases
In sarcoidosis, an inflammatory granulomatosis, optic nerve involvement occurs in 1–5% of the patients. The differential diagnosis, which includes optic nerve meningioma, can be difficult to elucidate but the MR demonstration of involvement of both optic nerves, complete optic nerve enhancement from globe to the chiasm, bilateral enlarged parotid and lacrimal glands, leptomeningeal enhancement and infundibular thickening all support the diagnosis of sarcoidosis.
Extracranial manifestations of granulomatosis with periangiitis, Langerhans cell, and non-Langerhans cell histiocytosis can also insult the optic nerves besides their orbital and nasosinusal involvement. The nearby maxillary nerve is also prone to be involved and intracranial extension along the involved nerves has been described [1, 2, 5, 7].
4.4.3.6 Graves’ Orbitopathy
Graves’ disease is an autoimmune condition of the thyroid involving the orbit in 25% of patients. The resulting ophthalmopathy is caused by extraocular muscle hypertrophy and adipogenesis leading to increased ocular pressure and proptosis, diplopia, and vision loss due to CN II compression and/or elongation.
4.4.3.7 Orbital Pseudotumor
Patients with orbital pseudotumor present with vison loss (CN II), ophthalmoplegia (CN III, IV, VI), sudden painful proptosis and uveitis, and retinal detachment. Infections and neoplasms must be excluded before this diagnosis can be made and rapid improvement with corticosteroid treatment can confirm the diagnosis. An ill-defined enhancing pseudo mass in the orbit, orbital apex, and superior/inferior orbital fissures can be seen on post-contrast FS T1W images. A useful imaging sign is that although the pseudo-mass can be large, the surrounding anatomical structures are not displaced accordingly.
4.4.4 Tumours
4.4.4.1 Primary Nerve Lesions
Esthesioneuroblastoma develops from the neurosensory receptor cells in the olfactory epithelium in the upper nasal meatus. They are typically centred on the anterior skull base, with often a dumbbell mass extending upward in the anterior fossa and downward in the nasal cavity, ethmoid and sphenoid sinuses. The extension of the mass, which can have cysts at the periphery, can best be delineated on MR. The destruction of the cribriform plate and anterior skull base is best depicted on CT. The intracranial component can involve CN I with anosmia as a result while the nasosinusal component causes nasal obstruction, rhinorrhoea, and epistaxis.
Optic nerve glioma, usually pilocytic astrocytoma, is the primary tumour of CN II and presents under the age of 20 years. On MRI and CT, these lesions follow the optic nerve in a fusiform way, cause kinking of the optic nerve, and may extend to the optic chiasm. On MRI, they have a typical high signal intensity on T2 and variable enhancement. Optic gliomas can be associated with neurofibromatosis I (NFI) and this is more likely with bilateral involvement, when they are not cyst-like, and do not extend to the optic chiasm, in contrast to the non-NFI-associated optic gliomas [34].
4.4.4.2 Nerve Sheath Tumours
The olfactory tracts and bulbs as well as the optic nerves are extensions of the brain and have no Schwann cells. However, the olfactory filia which connect the olfactory bulbs with the olfactory mucosa in the upper nasal meatus do have Schwann cells. Therefore, olfactory schwannomas exist but are not related to the olfactory tracts and bulbs themselves.
The intraorbital optic nerve has a meningeal sheath, and this explains the presence of meningiomas along CN II. Most of the meningiomas are isointense with grey matter, are fusiform, and enhance homogeneously with a “tram track” sign. This enhancement is best seen on contrast-enhanced 3D BB images as this sequence is more sensitive for contrast enhancement and less affected by susceptibility artifacts than post-contrast 3D T1WI (Fig. 12.5d, e).
All other CNs, except for CN VIII, have an extracranial course with a Schwann cell sheath on which schwannomas, neurofibromas, and rarely malignant tumours can arise. It is more likely to find schwannomas and neurofibromas on the extracranial end branches of CN V than on the short intraorbital branches of CN III, IV, and VI [32]. Regardless, intracranial CN schwannomas are far more frequent than extracranial CN schwannomas.
Nerve sheath tumours along the intraparotid branches of CN VII can occur but schwannomas/neurofibromas on the mastoid segment of the facial nerve with extension into the parotid gland are far more frequent.
Schwannomas can develop on the extracranial segment of all four lower cranial nerves but are most frequent on CN X. Extracranial schwannomas of CN XII can most often be followed into the hypoglossal canal and intracranial subarachnoid space. Extracranial nerve sheath tumours of cranial CNs IX and XI are rare.
On MRI, schwannomas are well-circumscribed, fusiform and have an intense enhancement. However, cystic, fatty, and haemorrhagic changes can occur resulting in an inhomogeneous lesion and/or inhomogeneous enhancement. Multiple extracranial CN schwannomas are most often found in patients with autosomal dominant neurofibromatosis type 2 (NF2), and bilateral vestibular schwannomas are even pathognomonic for NF2.
Extracranial CN neurofibromas are found in younger patients (20–30 years old), enhance weakly or not at all, and present as thickening of longer nerve segments. Nevertheless, they are sometimes difficult to distinguish from schwannomas. Most neurofibromas occur isolated, but the presence of multiple extracranial CN neurofibromas or a plexiform neurofibroma strongly suggests the diagnosis of NF1.
4.4.4.3 Secondary Nerve Involvement
4.4.4.3.1 Head and Neck Malignancies and Perineural Tumour Spread
All head and neck malignancies can displace or invade extracranial CNs. Squamous cell carcinomas, adenoid cystic carcinomas, adenocarcinoma, lymphomas, melanomas, retinoblastomas, esthesioneuroblastomas, rhabdomyosarcomas, malignant parotid gland tumours, thyroid malignancies, etc. can all affect the extracranial CNs, and which nerve is affected often depends on the typical location where some of these tumours arise. Tumoral infiltration of extracranial CNs is difficult to visualize although the use of diffusion tractography is promising for demonstrating nerve displacement and suggesting tumoral infiltration [11].
Adenoid cystic carcinoma, squamous cell carcinoma, and lymphoma are the most frequent malignant head and neck lesions with perineural spread although other malignant tumours also have the potential to follow the cranial nerves [35]. The most frequently involved nerves are V1 (skin and lacrimal malignancies), V2 (skin, oral and nasal cavity, and sinus malignancies), V3 (oral cavity-sublingual and submandibular gland and masticator space malignancies) [36], VII (parotid malignancies), and rarely CN XII.
Perineural spread can be seen as an abnormal enhancement and thickening of the involved nerves on post-contrast FS T1WI. Comparison with the contralateral nerve facilitates the diagnosis. It is crucial to detect intracranial CN extension as it limits therapeutic options, thereby avoiding potentially futile interventions, and results in a poorer prognosis.
CN V and VII have several connections which allow perineural tumoral spread along both nerves and their branches. The connection between the maxillary nerve (V2) and Vidian nerve (VII) at the level of the pterygopalatine fossa is most frequently involved. Hence, the pterygopalatine fossa should always be assessed in detail as involvement often heralds intracranial extension along these nerve branches.
4.4.4.3.2 Paragangliomas
The imaging characteristics of paragangliomas were already discussed in Sect. 12.4.3.3. Extracranially, they arise from glomus bodies located along the carotid bulb and vagus nerve inside the carotid space. Jugular foramen paragangliomas can also extend caudally in these carotid spaces where they can compress the four lower CNs. Intracranial extension should always be assessed prior to surgery.
4.4.4.3.3 Metastases
Hematogenous metastases to the head and neck region can involve all extracranial nerves with secondary CN deficits. Breast, kidney, lung, and prostate tumours as well as melanoma are the most frequent primary tumours that metastasize to the head and neck region. In the orbit, metastases from breast carcinoma are most frequent and involvement of CN II is more often caused by nerve compression by the orbital metastasis than by direct metastasis to the nerve itself. The extracranial CNs III–XII can be directly affected by all the above-mentioned metastases or indirectly by associated adenopathies. Metastatic extracranial CN involvement is best seen on post-contrast FS T1WI in the axial and coronal plane.
4.4.5 Trauma
Facial fractures can damage the extracranial CNs. The fractures and displaced bone fragments are best seen on CT, with contusion or shears, and oedema of the CNs best studied on MRI with 3D FLAIR and STIR images (Fig. 12.6a, b). One of the most frequently damaged nerves is the V2 branch. Its course along the floor of the orbit makes it vulnerable in cases of orbital floor, orbital blow out and tetrapod fractures. Also, the V1 branch can be damaged in cases of orbital roof fractures and the fractures can even reach the optic nerve (CN II) in the centre of the orbit. However, more frequently CN II involvement represents contusion (Fig. 12.6a, b) with nerve transection being relatively rare. Mandibular fractures can damage the V3 branch and/or the inferior alveolar nerve. CN disorders may also be iatrogenic and CN II, III, IV, and VI can be damaged during sinonasal and periorbital surgery. CN V3 can be injured during mandibular and tooth implant surgery while CN VII can be injured during parotid surgery, etc. One of the best-known iatrogenic CN traumas is contusion or transection of the lingual nerve, a branch from CN V3, during wisdom tooth extraction. Previously imaging was unable to demonstrate lingual nerve injury, but this is now possible with new dedicated MRN sequences (e.g. 3D CRANI) [37]. Lower cranial nerve deficits are most often caused by neck dissections or by surgery of the lower neck with recurrent laryngeal nerve damage and consequent vocal cord palsy one of the best-known examples [38]. Surgery can also cause scar formation around the extracranial CNs, replacing the usual fat around the nerves on unenhanced T1WI and enhancing in the early postsurgical period. Finally, neuromas can develop on extracranial CNs in cases of chronic trauma. Visualization of these neuromas on extracranial CNs was almost impossible before the advent of the dedicated MRN techniques like the 3D CRANI sequence (Fig. 12.6c, d).
Extracranial CN lesions: (a, b) Post-traumatic CN II contusion with visual loss. (a) Coronal contrast-enhanced high-resolution T1W image with fat suppression showing oedema of the optic nerve (arrow) and the oedematous changes of the optic nerve sheath and surrounding retro-ocular fat. (b) Axial 3D FLAIR image shows the extent of nerve contusion, reaching the optic canal (arrowheads); (c, d) Intensive care patient with left hypoglossal nerve palsy following a 3-month intubation. (c) Atrophy and fatty degeneration of the tongue muscles on the left side can be recognized on this axial T2W TSE image and confirms left hypoglossal nerve palsy. (d) Contrast-enhanced 3D CRANI image with parasagittal MIP reconstruction shows two neuromas on the inferior bend of the hypoglossal nerve (arrows) caused by a remote intubation trauma. For reference, the tongue (grey arrowhead) and region of the jugular foramen (white arrowhead) are depicted. (e, f) Patient presenting with a left recurrent laryngeal nerve palsy identified on contrast-enhanced CT. (e) Axial CT image shows the paramedian position of the left true vocal cord with a widened ventricle of Morgagni, in keeping with left vocal cord palsy (arrows). (f) Sagittal reconstruction demonstrates a large diaphragmatic herniation which causes upward displacement of the pulmonary arteries (black arrowheads) and closure of the aorta-pulmonic window (arrow) with subsequent compression and irritation of the recurrent laryngeal nerve branch resulting in the left vocal cord palsy. Aortic arch (grey arrowheads)
4.4.6 Upper Mediastinum
The vagus nerve and its left recurrent laryngeal branch can be followed down to the upper mediastinum. The left recurrent laryngeal nerve turns superiorly after crossing the aorto-pulmonary window. Mediastinitis and inflammatory adenopathies, tumoral adenopathies and tumours of the aerodigestive tract, upper mediastinum, lymphomas, etc. can therefore damage these nerves and cause CN X or recurrent laryngeal nerve deficits. All pathologies that result in narrowing of the aorto-pulmonary window can also compress the left recurrent laryngeal nerve and cause vocal cord palsy. Examples are aortic arch aneurysms, pulmonary hypertension, and massive diaphragmatic hernias (Fig. 12.6e, f).
4.5 Conclusion
Cranial nerve dysfunctions warn clinicians of pathology involving the face, skull base, or brain. Guided by medical history and clinical findings, imaging should be directed to the involved CN and to the right CN segment. An enormous variety of diseases can cause CN deficits; therefore, CT and MR are used to distinguish and characterize them. Aneurysms, dissections, skull base and skull lesions, fractures, and calcifications are best demonstrated by CT and CTA. Lesions of the CN themselves are best studied on MRI with new techniques like diffusion tractography, BB imaging, and 3D CRANI MRN serving to further strengthen MRI diagnostic authority.
Take-Home Messages
-
Master cranial nerve anatomy from the central nuclei to the peripheral branches.
-
Adapt imaging techniques to the clinical history and clinical findings, focusing on the right CN and CN segment.
-
Characterize causative lesions by using CT and/or MR, with the knowledge that different type of lesions affects the different CN segments.
-
Rule out intracranial lesions, aneurysms, and dissection that require specific treatment. Employ CTA and MRA to rule out painful vascular CN disorders.
-
Use the optimal adapted MR sequences such as heavy T2W, 3D FLAIR, and high-resolution T2W and T1W sequences, T1 without and with contrast and with fat saturation.
-
Consider DWI and the new DWI/DTI, 3D-BB, and 3D CRANI MRN techniques in appropriate cases.
Abbreviations
- ADC:
-
Apparent diffusion coefficient
- BB:
-
Black blood
- CN:
-
Cranial nerve
- CNs:
-
Cranial nerves
- CPA:
-
Cerebellopontine angle
- CSF:
-
Cerebrospinal fluid
- CT:
-
Computed tomography
- CTA:
-
Computed tomography angiography
- DWI:
-
Diffusion weighted images
- FS:
-
Fat-saturated
- IAC:
-
Internal auditory canal
- ICA:
-
Internal carotid artery
- MR:
-
Magnetic resonance
- MRA:
-
Magnetic resonance angiography
- MRN:
-
Magnetic resonance neurography
- MS:
-
Multiple sclerosis
- NF1:
-
Neurofibromatosis type 1
- NF2:
-
Neurofibromatosis type 2
- NMOSD:
-
Neuromyelitis optica spectrum disorders
- NVC:
-
Neurovascular conflict
- NVCS:
-
Neurovascular compression syndrome
- PD:
-
Proton density
- SWI:
-
Susceptibility weighted images
- T1W:
-
T1 weighted
- T1WI :
-
T1 weighted images
- T2W:
-
T2 weighted
- T2WI:
-
T2 weighted images
- TN:
-
Trigeminal neuralgia
- TOF:
-
Time of flight
- TZ:
-
Transition zone
References
Barkhof F, Jäger R, Thurnher M, Rovira A, editors. Clinical neuroradiology: the ESNR textbook. Cham: Springer; 2019. 2272 pp.
Casselman J, Mermuys K, Delanote J, Ghekiere J, Coenegrachts K. MRI of the cranial nerves—more than meets the eye: technical considerations and advanced anatomy. Neuroimaging Clin N Am. 2008;18:197–231, preceding x.
Chapman P, Harnsberger H, Vattoth S, editors. Imaging anatomy: head and neck. Philadelphia: Elsevier; 2019. 700 pp.
Harnsberger H. Cranial nerves. In: Harnsberger H, Osborn A, Macdonald A, Ross J, editors. Diagnostic and surgical imaging anatomy: brain, head and neck, spine. Salt Lake City: Amirsys; 2006. p. 174–259.
Koch B, Hamilton B, Hudgins P, Harnsberger H, editors. Diagnostic imaging: head and neck. 3rd ed. Philadelphia: Elsevier; 2017. 1352 pp.
Leblanc A, editor. Encephalo-peripheral nervous system: vascularisation, anatomy, imaging. Berlin: Springer; 2004. 420 pp.
Osborn A, Hedlund G, Salzman K, editors. Osborn’s brain. 2nd ed. Philadelphia: Elsevier; 2018. 1300 pp.
Romano N, Federici M, Castaldi A. Imaging of cranial nerves: a pictorial overview. Insights Imaging. 2019;10:33.
Jacquesson T, Cotton F, Attye A, Zaouche S, Tringali S, Bosc J, Robinson P, Jouanneau E, Frindel C. Probabilistic tractography to predict the position of cranial nerves displaced by skull base tumors: value for surgical strategy through a case series of 62 patients. Neurosurgery. 2019;85:E125–36.
Attye A, Jean C, Remond P, et al. Track-weighted imaging for neuroretina: evaluations in healthy volunteers and ischemic optic neuropathy. J Magn Reson Imaging. 2018;48:737.
Rouchy RC, Attye A, Medici M, Renard F, Kastler A, Grand S, Tropres I, Righini CA, Krainik A. Facial nerve tractography: a new tool for the detection of perineural spread in parotid cancers. Eur Radiol. 2018;28:3861–71.
Attye A, Karkas A, Tropres I, et al. Parotid gland tumours: MR tractography to assess contact with the facial nerve. Eur Radiol. 2016;26:2233–41.
Krainik A, Casselman JW. Imaging evaluation of patients with cranial nerve disorders. In: Hodler J, Kubik-Huch R, Von Schulthess G, editors. Diseases of the brain, head and neck, spine 2020–2023. Cham: IDKD Springer; 2020. p. 143–61. https://doi.org/10.1007/978-3-030-38490-6_12.
Klupp E, Cervantes B, Sollmann N, et al. Improved brachial plexus visualization using an adiabatic iMSDE-prepared stir 3D TSE. Clin Neuroradiol. 2019;29:631–8.
Van der Cruyssen F, Croonenborghs T-M, Hermans R, et al. 3D cranial nerve imaging, a novel MR neurography technique using black-blood STIR TSE with a pseudo steady-state sweep and motion-sensitized driven equilibrium pulse for the visualization of the extraforaminal cranial nerve branches. Am J Neuroradiol. 2021;42:578–80.
Van der Cruyssen F, Croonenborghs T-M, Renton T, et al. Magnetic resonance neurography of the head and neck: state of the art, anatomy, pathology, and future perspectives. Br J Radiol. 2021;94:20200798.
Casselman J, Van der Cruyssen F, Vanhove F, et al. 3D CRANI, a novel MR neurography sequence, can reliable visualise the extraforaminal cranial and occipital nerves. Eur Radiol. 2023;33:2861–70.
van der Zijden T, Mondelaers A, Yperzeele L, Voormolen M, Parizel P. Current concepts in imaging and endovascular treatment of acute ischemic stroke: implications for the clinician. Insights Imaging. 2019;10:64.
Dutra BG, da Rocha AJ, Nunes RH, Maia ACMJ. Neuromyelitis optica spectrum disorders: spectrum of MR imaging findings and their differential diagnosis. Radiographics. 2018;38:169–93.
Di Stefano G, Maarbjerg S, Truini A. Trigeminal neuralgia secondary to multiple sclerosis: from the clinical picture to the treatment options. J Headache Pain. 2019;20:20.
Bonneville F, Savatovsky J, Chiras J. Imaging of cerebellopontine angle lesions: an update. Part 1: enhancing extra-axial lesions. Eur Radiol. 2007;17:2472–82.
Bonneville F, Savatovsky J, Chiras J. Imaging of cerebellopontine angle lesions: an update. Part 2: intra-axial lesions, skull base lesions that may invade the CPA region, and non-enhancing extra-axial lesions. Eur Radiol. 2007;17:2908–20.
Radek M, Tomasik B, Wojdyn M, et al. Neurofibromatosis type 2 (NF2) or schwannomatosis? Case report study and diagnostic criteria. Neurol Neurochir Pol. 2016;50:215–9.
Krainik A, Cyna-Gorse F, Bouccara D, Cazals-Hatem D, Vilgrain V, Denys A, Rey A, Sterkers O, Menu Y. MRI of unusual lesions in the internal auditory canal. Neuroradiology. 2001;43:52–7.
Haller S, Etienne L, Kovari E, Varoquaux AD, Urbach H, Becker M. Imaging of neurovascular compression syndromes: trigeminal neuralgia, hemifacial spasm, vestibular paroxysmia, and glossopharyngeal neuralgia. AJNR Am J Neuroradiol. 2016;37:1384–92.
Adams ME, Linn J, Yousry I. Pathology of the ocular motor nerves III, IV, and VI. Neuroimaging Clin N Am. 2008;18:261–82, preceding x–x.
Kuya J, Kuya K, Shinohara Y, Kunimoto Y, Yazama H, Ogawa T, Takeuchi H. Usefulness of high-resolution 3D multi-sequences for peripheral facial palsy: differentiation between Bell’s palsy and Ramsay hunt syndrome. Otol Neurotol. 2017;38:1523–7.
Veillon F, Taboada LR, Eid MA, Riehm S, Debry C, Schultz P, Charpiot A. Pathology of the facial nerve. Neuroimaging Clin N Am. 2008;18:309–20, x.
Nery B, Fernandes Costa RA, Quaggio E, et al. Jugular foramen paragangliomas. In: Morgan LR, Sarica FB, editors. Brain and spinal tumors. Rijeka: IntechOpen; 2019. https://doi.org/10.5772/intechopen.84232.
Zurawski J, Akhondi H. Tolosa-hunt syndrome a rare cause of headache and ophthalmoplegia. Lancet. 2013;382:912.
Soussan JB, Deschamps R, Sadik JC, et al. Infraorbital nerve involvement on magnetic resonance imaging in European patients with IgG4-related ophthalmic disease: a specific sign. Eur Radiol. 2017;27:1335–43.
Smoker WR, Reede DL. Denervation atrophy of motor cranial nerves. Neuroimaging Clin N Am. 2008;18:387–411, xi.
Chhabra A, Bajaj G, Wadhwa V, et al. MR neurography evaluation of facial and neck pain: normal and abnormal craniospinal nerves below the skull base. Radiographics. 2018;38:1498–513. https://doi.org/10.1148/rg.2018170194.
Louis D, Ohgaki H, Wiestier O, Cavenee W, editors. WHO classification of tumors of the central nervous system. 4th ed. IARC: Lyon; 2016.
Maroldi R, Farina D, Borghesi A, Marconi A, Gatti E. Perineural tumor spread. Neuroimaging Clin N Am. 2008;18:413–429, xi.
Borges A, Casselman J. Imaging the trigeminal nerve. Eur J Radiol. 2010;74:323–40.
Bangia M, Ahmadzai I, Casselman J, et al. Accuracy of MR neurography as a diagnostic tool in detecting injuries to the lingual- and inferior alveolar nerve in patients with iatrogenic post-traumatic trigeminal neuropathy. Eur Radiol. 2023; https://doi.org/10.1007/s00330-023-10363-2.
Lee JH, Cheng KL, Choi YJ, Baek JH. High-resolution imaging of neural anatomy and pathology of the neck. Korean J Radiol. 2017;18:180–93.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2024 The Author(s)
About this chapter
Cite this chapter
Casselman, J.W., Krainik, A., Macdonald, I. (2024). Evaluation of Patients with Cranial Nerve Disorders. In: Hodler, J., Kubik-Huch, R.A., Roos, J.E. (eds) Diseases of the Brain, Head and Neck, Spine 2024-2027. IDKD Springer Series. Springer, Cham. https://doi.org/10.1007/978-3-031-50675-8_12
Download citation
DOI: https://doi.org/10.1007/978-3-031-50675-8_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-50674-1
Online ISBN: 978-3-031-50675-8
eBook Packages: MedicineMedicine (R0)