Abstract
Death is common in the ICU often preceded by withdrawal of life-sustaining interventions. Therefore, health care professionals working in critical care should be experts in patient-family-centred care: this should include evaluating individuals for the potential of organ and tissue donation, and ensuring that the option of organ and tissue donation (OTD) is presented to patients or families. Organ donation is possible after either neurological determination of death (often colloquially known as brain death) or determination of death by cardiocirculatory criteria. Tissue donation is possible in many individuals, and like organ donation, may improve quality of life (e.g. cornea transplant), and saves lives (e.g. allogenic skin donation for use in major thermal injuries). This paper discusses aspects of OTD in the ICU highlighting some issues of importance for the health care professional.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Wunsch H. The outbreak that invented intensive care. Nature. 2020. https://www.nature-com/articles/d41586-020-01019-y. Accessed 29 April 2021.
Woodard SC. The story of the mobile army surgical hospital. Military Med. 2003;168:503–13.
Kelly FE, Fong K, Hirsch N, Nolan JP. Intensive care medicine is 60 years old: the history and future of the intensive care unit. Clin Med (London). 2014;14:376–9.
Sprung CL, Truog RD, Curtis JR, et al. Seeking worldwide professional consensus on the principles of end-of-life care for the critically ill. Am J Respir Crit Care Med. 2014;190:855–66.
Heyland DK, Lavery JV, Tranmer JE, Shortt SE, Taylor SJ. Dying in Canada: is it an institutionalized, technologically supported experience? J Palliat Care. 2000;16(Suppl):S10–6.
Azoulay E, Chevret S, Leleu G, et al. Half the families of intensive care unit patients experience inadequate communication with physicians. Crit Care Med. 2000;28:3044–9.
Prendergast TJ, Claessens MT, Luce JM. A national survey of end-of-life care for critically ill patients. Am J Resp Crit Care Med. 1998;158:1163–7.
Solverson KJ, Roze des Ordons AL, Doig CJ. Withholding and withdrawing life support: difficult decisions around care at the end of life. Can J Anaesth. 2017;65:9–13.
Roze des Ordons AL, MacIsaac L, Everson J, Hui J, Ellaway RH. A pattern of compassion in intensive care and palliative care contexts. BMC Palliat Care. 2019;18:15. https://doi.org/10.1186/s12904-019-0402-0.
Berlinger N, Jennings B, Wolf SM. The hastings center guidelines for decisions on life-sustaining treatment and care near the end of life: revised and expanded second edition. Oxford, UK: Oxford University Press; 2013.
Bandrauk N, Downar J. Paunovic B on behalf of the Canadian Critical Care Society Ethics Committee. Withholding and withdrawing of life-sustaining treatment: the Canadian Critical Care Society position paper. Can J Anaesth. 2018;65:105–22.
Frank C, Heyland DK, Chen B, Farquhar D, Myers K, Iwaasa K. Determining resuscitation preferences of elderly inpatients: a review of the literature. CMAJ. 2003;169:795–9.
Torke AM, Sachs GA, Helft PR, et al. Scope and outcomes of surrogate decision making among hospitalized older adults. JAMA Intern Med. 2014;174:370–7.
Brown SM, Rozenblum R, Aboumatar H, et al. Defining patient and family engagement in the intensive care unit. Am J Respir Crit Care Med. 2015;191:358–60.
Abbott KH, Sago JG, Breen CM, Abernathy AP, Tulsky JA. Families looking back: one year after discussion of withdrawal or withholding of life-sustaining support. Crit Care Med. 2001;29:197–201.
Schuster RA, Hong SY, Arnold RM, White DB. Investigating conflicts in ICUs—is the clinicians’ perspective enough? Crit Care Med. 2014;42:328–35.
Roze des Ordons A, Kassam A, Simon J. Goals of care conversations teaching in residency—a cross-sectional survey of postgraduate program directors. BMC Med Educ. 2017;17:6. https://doi.org/10.1186/s12909-016-0839-2.
Bush SH, Roze des Ordons A, Chary S, Boyle AB. The development and validation of updated palliative and end-of-life care competencies for medical undergraduates in Canada. J Palliat Med. 2019;22:1498–500.
Roze des Ordons AL, Doig CJ, Couillard P, Lord J. From communication skills to skillful communication: a longitudinal curriculum for critical care medicine fellows. Acad Med. 2017;92:501–5.
Wessman BT, Sona C, Schallom M. Improving caregivers’ perceptions regarding patient goals of care/end-of-life issues for the multidisciplinary critical care team. J Int Care Med. 2017;32:68–76.
Heyland DK, Cook DJ, Rocker GM, et al. Decision-making in the ICU: perspectives of the substitute decision-maker. Int Care Med. 2003;29:75–82.
Heyland DK, Tranmer J, O’Callaghan CJ, Gafni A. The seriously ill hospitalized patient: preferred role in end-of-life decision making? J Crit Care. 2003;18:3–10.
Davidson JE, Aslakson RA, Long AC, et al. Guidelines for family-centred care in the neonatal, pediatric, and adult ICU. Crit Care Med. 2017;45:103–28.
Seaman JB, Arnold RM, Scheunemann LP, et al. An integrated framework for effective and efficient communication with families in the adult intensive care unit. Ann Am Thorac Soc. 2017;14:1015–20.
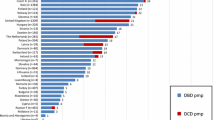
Kramer AH, Baht R, Doig CJ. Time trends in organ donation after neurologic determination of death: a cohort study. CMAJ Open. 2017:5. https://doi.org/10.9778/cmajo.20160093.
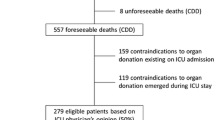
Kramer AH, Hornby K, Doig CJ, et al. Deceased organ donation potential in Canada: a review of consecutive deaths in Alberta. Can J Anaesth. 2019;66:1347–55.
Ad Hoc Committee of the Harvard Medical School. A definition of irreversible coma. JAMA. 1968;205:337–40.
Greer DM, Shemie SD, Lewis A, et al. Determination of brain death/death by neurologic criteria. The World Brain Death Project. JAMA. 2020;324:1078–97.
Lewis A, Bakkar A, Kreiger-Benson E, et al. Determination of death by neurologic criteria around the world. Neurology. 2020;95:e299–309.
Wahlster S, Wijdicks EFM, Patel PV, et al. Brain death declaration: practices and perceptions worldwide. Neurology. 2015;84:1870–9.
Wijdicks EF. Brain death worldwide: accepted fact, but no global consensus in diagnostic criteria. Neurology. 2002;58:20–5.
Citerio G, Cypel M, Dobb GJ, et al. Organ donation in adults: a critical care perspective. Int Care Med. 2016;42:305–15.
Kramer AH. Ancillary testing in brain death. Semin Neurol. 2015;35:125–38.
Kentish-Barnes N, Siminoff LA, Walker W, et al. A narrative review of family members’ experience of organ donation request after brain death in the critical care setting. Int Care Med. 2019;45:331–42.
Zheng K, Sutherland S, Cardinal P, et al. Patient-centered and family-centered care of critically ill patients who are potential organ donors: a qualitative study protocol of family member perspectives. BMJ Open. 2020;10:e037527. https://doi.org/10.1136/bmjopen-2020-037527.
Morgan SE, Harrison TR, Afifi WA, Long SD, Stephenson MT. In their own words: the reasons why people will (not) sign an organ donor card. Health Communication. 2008;23:23–33.
Whyte KP, Selinger E, Caplan AL, Sadowski J. Nudge, nudge or shove, shove—the right way for nudges to increase the supply of donated cadaver organs. Am J Bioethics. 12:32–9.
Potts M, Verheijde JL, Rady MY. When a nudge becomes a shove. Am J Bioethics. 2012;12:40–2.
Manzari ZS, Mohammadi E, Heydari A, Sharbaf HRA, Azizi JM, Khaleghi E. Exploring families’ experiences of an organ donation request after brain death. Nurs Ethics. 2012;19:654–65.
Al-Khafaji A, Murugan R, Kellum JA. What’s new in organ donation: better care of the dead for the living. Int Care Med. 2013;39:2031–3.
Singbartl K, Murugan R, Kaynar AM, et al. Intensivist-led management of brain-dead donors is associated with an increase in organ recovery for transplantation. Am J Transplant. 2011;11:1517–21.
Shemie SD, Ross H, Pagliarello J, et al. Organ donor management in Canada: recommendations of the forum on medical management to optimize donor organ potential. CMAJ. 2006;174:S13–32.
Ball IM, Hornby L, Rochwerg B, et al. Management of the neurologically deceased organ donor: A Canadian clinical practice guideline. CMAJ. 2020;192:E361–9.
Kotloff RM, Blosser S, Fulda GJ, et al. Management of the potential organ donor in the ICU: Society of Critical Care Medicine/American College of Chest Physicians/Association of Organ Procurement Organizations Consensus Statement. Crit Care Med. 2015;43:1291–325.
Pandit RA, Zirpe KG, Gurav SK, et al. Management of potential organ donor: Indian Society of Critical Care Medicine: position statement. Indian J Crit Care Med. 2017;21:303–16.
GRADE; www.gradeworkinggroup.org
Smith M, Dominguez-Gil B, Greer DM, Manara AR, Souter MJ. Organ donation after circulatory death: current status and future potential. Int Care Med. 2019;45:310–21.
Ethical, psychosocial, and public policy implications of procuring organs from non-heart-beating cadavers. Arnold RM, Youngner SJ, guest editors. Kennedy Institute of Ethics Journal Volume 3, 1993. Johns Hopkins University Press, Baltimore.
Shemie S, Baker AJ, Knoll G, et al. Donation after cardiocirculatory death in Canada. CMAJ. 2006;175:S1–24.
van Haren FMP, Carter A, Cavazzoni E, et al. Conflicts of interest in the context of end of life care for potential organ donors in Australia. J Crit Care. 2020;59:166–71.
Bastami S, Matthes O, Krones T, Biller-Andorno N. Systematic review of attitudes toward donation after cardiac death among health care providers and the general public. Crit Care Med. 2013;41:897–905.
Turgeon AF, Lauzier F, Simard JF, et al. Mortality associated with withdrawal of life-sustaining therapy for patients with severe traumatic brain injury: a Canadian multicentre cohort study. CMAJ. 2011;183:1581–8.
Cook DJ, Guyatt GH, Jaeschke R, et al. Determinants in Canadian health care workers of the decision to withdraw life support from the critically ill. JAMA. 1995;273:703–8.
Woodruff MFA. Ethical problems in organ transplantation. BMJ. 1964:1457–60.
Healey A, Hartwick M, Downar J, et al. Improving quality of withdrawal of life-sustaining measures in organ donation: a framework and implementation toolkit. Can J Anaesth. 2020;67:1549–56.
Gries CJ, White DB, Truog RD, et al. Ethical and policy considerations in organ donation after circulatory determination of death. Am J Resp Crit Care Med. 2013;188:103–9.
Cooper J. Organs and organisations: situating ethics in organ donation after circulatory death in the UK. Soc Sci Med. 2018;209:104–10.
Robertson J. The dead donor rule. Hast Center Rep. 1999;29:6–14.
Dhanani S, Hornby L, van Beinum A, et al. Resumption of cardiac activity after withdrawal of life-sustaining measures. New Engl J Med. 2021;384:345–52.
Rady MY, Verheijde JL. Scientific and ethical challenges in end-of-life organ donation. Crit Care Med. 2015;43:e526.
Joffe A. Are recent defences of the brain death concept adequate? Bioethics. 2010;24:47–53.
Joffe A. Confusion about brain death. Nat Rev Neurosci. 2006;7:590. https://doi.org/10.1038/nrn1789-c1.
Glannon W. The moral insignificance of death in organ donation. Camb Q Healthc Ethics. 2013;22:192–202.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Doig, C.J., Solverson, K.J. (2023). End-of-Life Care, Including the Role of Intensive Care in Tissue and Organ Donation. In: Coccolini, F., Catena, F. (eds) Textbook of Emergency General Surgery. Springer, Cham. https://doi.org/10.1007/978-3-031-22599-4_34
Download citation
DOI: https://doi.org/10.1007/978-3-031-22599-4_34
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-22598-7
Online ISBN: 978-3-031-22599-4
eBook Packages: MedicineMedicine (R0)