Abstract
The outcome of patients with large B cell lymphoma (LBCL) who did not respond to a classical immunochemotherapy regimen at any time or relapsed within 1 year following chemoimmunotherapy is poor. The Scholar-One-Study showed long-term event-free survival for less than 20% of these patients (Crump et al. 2017). The introduction of chimeric antigen receptor T cell therapy (CAR-T) is a substantial advancement for these patients, offering long-term remission and a curative prospect for 30 to 40% of patients (summarized in Table 12.1), (Abramson et al. 2020; Neelapu et al. 2017; Schuster et al. 2019b). To date, in Europe, two products (axicabtagene ciloleucel and tisagenlecleucel) have been licenced by the European Medical Agency, and a third product (lisocabtagene maraleucel) will become available in 2021. All these products are licenced for patients who have failed at least two prior lines of systemic therapy. This initially defines, however broad, a range of possible situations in which the application of CART is indicated. The following considerations may help to further define the patient population that should be offered CAR-T cells as the next line of treatment. Studies addressing the potential benefit of CAR-T cells compared to high-dose chemotherapy and autologous stem cell transplantation for second-line treatment of LBCL have been fully recruited, but the results are still pending.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
The outcome of patients with large B cell lymphoma (LBCL) who did not respond to a classical immunochemotherapy regimen at any time or relapsed within 1 year following chemoimmunotherapy is poor. The Scholar-One-Study showed long-term event-free survival for less than 20% of these patients (Crump et al. 2017). The introduction of chimeric antigen receptor T cell therapy (CAR-T) is a substantial advancement for these patients, offering long-term remission and a curative prospect for 30 to 40% of patients (summarized in Table 12.1), (Abramson et al. 2020; Neelapu et al. 2017; Schuster et al. 2019b). To date, in Europe, two products (axicabtagene ciloleucel and tisagenlecleucel) have been licenced by the European Medical Agency, and a third product (lisocabtagene maraleucel) will become available in 2022. All these products are licenced for patients who have failed at least two prior lines of systemic therapy. This initially defines, however broad, a range of possible situations in which the application of CART is indicated. The following considerations may help to further define the patient population that should be offered CAR-T cells as the next line of treatment. Recently the results of three randomized phase III clinical studies comparing CD19-CART with standard of Care in transplant eligible patients were reported. The BELINDA-Trial using Tisa-cel did not reach its primary endpoint EFS (Bishop et al. 2021). Two of the studies, ZUMA-7 using the construct Axi-cel and TRANSFORM using Liso-cel were positive for their primary endpoint EFS as well as for the key secondary endpoints PFS and ORR (Kamdar et al. 2021; Locke et al. 2021). In both studies a strong numerical trend towards a positive result regarding OS was observed with Hazard ratios of 0.72 and 0.51, respectively. TRANSFORM had a short median observation time so the results regarding OS were immature. In both studies showed significant advantages in quality of life for CART therapy over ASCT. Anti-CD19 CART therapy with one of these compounds should be considered standard of care in transplant-eligible patients as second line therapy in R/R LBCL.
Patient Population to Consider: Lymphoma-Specific Aspects
Treatment History
Depending on clinical risk factors, between 5 and 50% of LBCL patients may fail standard first-line immunochemotherapy (Coiffier et al. 2010; Cunningham et al. 2013; Pfreundschuh et al. 2011; Schmitz et al. 2012). Overall, 30–40% of patients will need salvage treatment. Patients eligible for high-dose chemotherapy currently receive a platinum-containing salvage protocol, followed by high-dose chemotherapy and autologous stem cell transplantation (autoSCT). In short, the remission rate varies between 35 and 50%, and with another approximately 50% failure rate after autoSCT, the overall long-term event-free survival rate is in the range of 25%. Thus, approximately 75% of younger patients with relapsed/refractory aggressive B cell lymphoma are theoretically eligible for CAR-T cell therapy. All young, fit patients without remission after salvage therapy in second-line situations should be considered for CAR-T cell therapy.
Elderly patients with relapsed or refractory LBCL have poor results with second-line therapy. An analysis of the secondary overall survival of patients in a large randomized first-line study revealed that patients with primary refractory disease never achieved long-term remission, and the median overall survival was less than 6 months (Glass et al. 2017). In 20–30% of patients, induction of remission is possible with platinum- or bendamustine-containing regimens, such as R-gemcitabine-oxaliplatin; however, due to the lack of effective consolidative therapy, the long-term outcome was poor in all series (Dhanapal et al. 2017; Franch-Sarto et al. 2019). In the three pivotal CD19 CAR-T trials, 23–42% of patients were ≥65 years old, and there are currently no indications that the efficacy of CAR-T cells in terms of remission rate and progression-free survival is inferior for elderly patients (Neelapu, Schuster, Abramson). In a real-world series, the percentage of elderly patients was higher, and there was some evidence of increased toxicity, especially neurotoxicity, but the efficacy appeared to be at last equal (Pasquini CIBMTR, Nastoupil).
Therefore, the option of CAR-T cell therapy must be discussed for most transplant ineligible but fit patients with relapsed or refractory aggressive B cell lymphoma after 2 prior lines of systemic therapy.
Remission Status and Tumour Bulk Prior to CAR-T Cell Infusion
CAR-T cells have been evaluated in patients with refractory and early relapsed disease. In pivotal studies of the three licenced CAR-T products, the fraction of refractory patients varied between 52 and 79%. Being refractory to the last line of chemotherapy was not a significant prognostic factor in these studies. Therefore, in contrast to autologous or allogeneic SCT, being in remission is not a prerequisite for the application of CAR-T therapy. However, pivotal clinical studies and the first real-world evidence reports identify high tumour volume, reflected by the sum of product diameters (SPD) or simply an elevated LDH, prior to lymphodepleting therapy as a significant negative prognostic factor for the ongoing complete response rate or PFS (Nastoupil et al. 2020), with a hazard ratio of 3.0. In addition, patients with rapidly progressing disease often do not respond to attempts at bridging therapy, and the need for systemic bridging therapy is a negative predictor for response and survival.
When discussing the value of CAR-T cell therapy for an individual patient, this parameter—disease control prior to CAR-T cell infusion—must be considered. However, this parameter also has an impact on the results of any alternative treatment, and at which point CAR-T cell therapy cannot achieve long-term remission and should not be offered is still a matter of debate.
Histology
The majority of patients in ZUMA-1, JULIET, and TRANSCEND had DLBCL (76%, 80% and 64%); transformed FL was present in 16–22% of cases, and only a small number of patients with PMBCL (8% in ZUMA-1 and 6% in TRANSCEND) were included. Data on DH/TH lymphoma were not available for all patients. There were no significant differences in response rates or PFS in specific subgroups.
Patient Population to Consider: Patient-Specific Aspects
CAR-T cell therapy can lead to unusual and sometimes severe acute toxicities, with cytokine release syndrome (CRS) and immune effector cell-associated neurotoxicity (ICANS) being the most important. These toxicities typically occur between Day 2 and Day 10 after infusion and may persist for several days to weeks. Treatment-related mortality is a rare event, and in most cases, the toxicity is reversible. Other important side effects include severe neutropenia, which may last for several weeks or months, long-term B cell depletion, and hypogammaglobulinaemia, which is an on-target off-tumour toxicity. Compared to the morbidity and mortality associated with other treatment modalities applied in this situation, such as allogeneic SCT, the impact of CAR-T cell-associated toxicity on the overall outcome is moderate. It has been claimed that the good results of CAR-T therapy in terms of toxicity are due to the strict eligibility criteria of the pivotal studies, but recent analyses of data from real-world application of CAR-T therapy showed that efficacy and toxicity were similar, even if elderly and more comorbid patients were treated (Nastoupil et al. 2020). The risk factors for TRM after CAR-T cell therapy are not well defined, and conclusions from other treatment options might be difficult to transfer to CAR-T cell therapy. The best approximation might be the use of the high-dose chemotherapy comorbidity index and its results for patients undergoing autologous SCT. In such an analysis, the HDT-correlated NRM ranged from 3.3 to 7.7% (Berro et al. 2017) after 1 year, which is in line with what has been observed after CAR-T cell therapy (therapy-related mortality <5%).
Alternative Treatments
In the past, allogeneic stem cell transplantation was the only option for consolidation in chemorefractory patients after additional salvage therapy. Recently, antibody–drug conjugates and bispecific antibodies have shown interesting results in the patient population discussed here. Polatuzumab vedotin, the first drug in these groups, has been licenced in Europe and the USA. Many other drugs may enter the arena in the near future. Integration of CAR-T cell therapy with these new treatment options will be a major task in the future.
-
Allogeneic stem cell transplantation
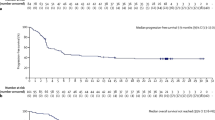
In the past, alloSCT has mostly been used in patients who relapse after autologous stem cell transplantation, and data have been reported from international registries (Fenske et al. 2016; van Kampen et al. 2011). One prospective clinical trial in patients with high-risk aggressive lymphoma showed a PFS and OS of 39% and 40%, respectively, after 4 years (Glass et al. 2014). Taking the potential bias of indirect comparison of treatment results between studies and registry data into account, it can be grossly stated that in many series of allogeneic stem cell transplantation, the overall results in terms of progression-free survival may be comparable to that of CAR-T therapy; however, the balance between the antilymphoma effect and toxicity is dramatically different from that of CAR-T therapy. Treatment-related mortality and morbidity are dramatically higher after allogeneic stem cell transplantation in any age group of patients. Thus, currently, even in patients eligible for alloSCT, CAR-T cells should be offered first. Allogeneic SCT remains a treatment modality that should be considered in patients failing CART therapy, provided they respond to salvage treatment.
-
Antibody drug conjugates
Polatuzumab vedotin is the first ADC that has been licenced for transplant-ineligible patients with DLBCL after failure of at least one prior therapy. In the pivotal randomized phase II study (Sehn et al. 2020a) and the recently reported expansion cohort (Sehn et al. 2020b), the patient population treated was comparable to the populations in most of the CAR-T cell studies. The best overall response rate was 57.9%, with a CR rate of 52.6%. Some of the responses seem to be ongoing after the end of treatment. With the limited number of patients and the limited observation time, it can be estimated that approximately 15–20% of patients might be in ongoing remission after 2 years. Thus, the potential to serve as a curative treatment is small if it exists at all, and a longer follow-up time and validation in other prospective clinical trials are warranted. ADCs, such as polatuzumab vedotin, might be good candidates for achieving control of the disease prior to CAR-T cell application in a so-called bridging approach. Polatuzumab is licenced in combination with bendamustine, a drug with exceptionally high T cell toxicity. The application of bendamustine should be avoided prior to apheresis of autologous T cells for CAR-T cell production.
-
Bispecific antibodies
A number of bispecific, T cell-engaging antibodies using the CD20 antigen as a lymphoma-specific target and CD3 as a T cell binding site have been reported with very encouraging results (Table 12.2) (Bannerji et al. 2020; Hutchings et al. 2020a,b; Schuster et al. 2019a). The response rates are high for some of the agents, and the toxicity is quite limited. However, the observation time is still short, and data on PFS are not yet available. There is an indication that the DOR of patients achieving CR is particularly good thus far and in the same range as that observed in trials of CAR-T cells. Bispecific antibodies may have the potential to induce long-lasting remissions without further consolidation, but this treatment is often given until progression or toxicity occurs. Once available in routine practice, their differential indication for treatment compared to CAR-T cells will become an important clinical challenge and should preferably be investigated in head-to-head clinical trials.
Key Points
-
Patients with LBCL, including transformed FL and PMBCL, should be considered for CD19 CAR-T cell therapy in cases of relapsed/refractory disease after ≥2 lines of systemic therapy.
-
There is no upper age limit, but patients should fulfil eligibility criteria in terms of fitness, cardiac function, and other organ functions.
-
Patients with high LDH and rapidly progressing disease are less likely to benefit.
References
Abramson JS, Palomba ML, Gordon LI, Lunning MA, Wang M, Arnason J, et al. Lisocabtagene maraleucel for patients with relapsed or refractory large B-cell lymphomas (TRANSCEND NHL 001): a multicentre seamless design study. Lancet. 2020;396:839–52.
Bannerji R, Allan JN, Arnason JE, Brown JR, Advani R, Ansell SM, et al. Odronextamab (REGN1979), a human CD20 x CD3 bispecific antibody, induces durable, complete responses in patients with highly refractory B-cell non-Hodgkin lymphoma, including patients refractory to CAR-T therapy. Blood. 2020;136:42–3.
Berro M, Arbelbide JA, Rivas MM, Basquiera AL, Ferini G, Vitriu A, et al. Hematopoietic cell transplantation-specific comorbidity index predicts morbidity and mortality in autologous stem cell transplantation. Biol Blood Marrow Transplant. 2017;23:1646–50.
Bishop MR, Dickinson M, Purtill D, Barba P, Santoro A, Hamad N, et al. Second-Line tisagenlecleucel or standard care in aggressive B-Cell lymphoma. N Engl J Med. 2021. Dec 14, Online ahead of print.
Coiffier B, Thieblemont C, Van Den Neste E, Lepeu G, Plantier I, Castaigne S, et al. Long-term outcome of patients in the LNH-98.5 trial, the first randomized study comparing rituximab-CHOP to standard CHOP chemotherapy in DLBCL patients: a study by the Groupe d’Etudes des Lymphomes de l’Adulte. Blood. 2010;116:2040–5.
Crump M, Kuruvilla J, Couban S, Macdonald DA, Kukreti V, Kouroukis CT, et al. Randomized comparison of gemcitabine, dexamethasone, and cisplatin versus dexamethasone, cytarabine, and cisplatin chemotherapy before autologous stem-cell transplantation for relapsed and refractory aggressive lymphomas: NCIC-CTG LY.12. J Clin Oncol. 2014;32:3490–6.
Crump M, Neelapu SS, Farooq U, Van Den Neste E, Kuruvilla J, Westin J, et al. Outcomes in refractory diffuse large B-cell lymphoma: results from the international SCHOLAR-1 study. Blood. 2017;130:1800–8.
Cunningham D, Hawkes EA, Jack A, Qian W, Smith P, Mouncey P, et al. Rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisolone in patients with newly diagnosed diffuse large B-cell non-Hodgkin lymphoma: a phase 3 comparison of dose intensification with 14-day versus 21-day cycles. Lancet. 2013;381:1817–26.
Dhanapal V, Gunasekara M, Lianwea C, Marcus R, De Lord C, Bowcock S, et al. Outcome for patients with relapsed/refractory aggressive lymphoma treated with gemcitabine and oxaliplatin with or without rituximab; a retrospective, multicentre study. Leuk Lymphoma. 2017;58:1–9.
Fenske TS, Ahn KW, Graff TM, DiGilio A, Bashir Q, Kamble RT, et al. Allogeneic transplantation provides durable remission in a subset of DLBCL patients relapsing after autologous transplantation. Br J Haematol. 2016;174:235–48.
Franch-Sarto M, Sorigue M, Lopez L, Moreno M, Ribera JM, Sancho JM. Overall survival in patients with relapsed/refractory high grade B-cell lymphomas treated with gemcitabine, oxaliplatin with or without rituximab. Leuk Lymphoma. 2019;60:3324–6.
Gisselbrecht C, Glass B, Mounier N, Singh GD, Linch DC, Trneny M, et al. Salvage regimens with autologous transplantation for relapsed large B-cell lymphoma in the rituximab era. J Clin Oncol. 2010;28:4184–90.
Glass B, Hasenkamp J, Wulf G, Dreger P, Pfreundschuh M, Gramatzki M, et al. Rituximab after lymphoma-directed conditioning and allogeneic stem-cell transplantation for relapsed and refractory aggressive non-Hodgkin lymphoma (DSHNHL R3): an open-label, randomised, phase 2 trial. Lancet Oncol. 2014;15:757–66.
Glass B, Dohm AJ, Truemper LH, Pfreundschuh M, Bleckmann A, Wulf GG, et al. Refractory or relapsed aggressive B-cell lymphoma failing (R)-CHOP: an analysis of patients treated on the RICOVER-60 trial. Ann Oncol. 2017;28:3058–64.
Hutchings M, Carlo-Stella C, Bachy E, Offner FC, Morschhauser F, Crump M, et al. Glofitamab step-up dosing induces high response rates in patients with hard-to-treat refractory or relapsed non-Hodgkin lymphoma. Blood. 2020a;136:46–8.
Hutchings M, Mous R, Clausen MR, Johnson P, Linton KM, Chamuleau MED, et al. Subcutaneous Epcoritamab induces complete responses with an encouraging safety profile across relapsed/refractory B-cell non-Hodgkin lymphoma subtypes, including patients with prior CAR-T therapy: updated dose escalation data. Blood. 2020b;136:45–6.
van Imhoff GW, McMillan A, Matasar MJ, Radford J, Ardeshna KM, Kuliczkowski K, et al. Ofatumumab versus rituximab salvage chemoimmunotherapy in relapsed or refractory diffuse large B-cell lymphoma: the ORCHARRD Study. J Clin Oncol. 2017;35:544.
Kamdar M, Solomon SR, Arnason JE, Johnston PB, Glass B, Bachanova V, et al. Lisocabtagene Maraleucel (liso-cel), a CD19-Directed Chimeric Antigen Receptor (CAR) T Cell Therapy, Versus Standard of Care (SOC) with Salvage Chemotherapy (CT) Followed By Autologous Stem Cell Transplantation (ASCT) As Second-Line (2L) Treatment in Patients (Pts) with Relapsed or Refractory (R/R) Large B-Cell Lymphoma (LBCL): Results from the Randomized Phase 3 Transform Study. Blood. 2021;138:91–91.
van Kampen RJ, Canals C, Schouten HC, Nagler A, Thomson KJ, Vernant JP, et al. Allogeneic stem-cell transplantation as salvage therapy for patients with diffuse large B-cell non-Hodgkin’s lymphoma relapsing after an autologous stem-cell transplantation: an analysis of the European Group for Blood and Marrow Transplantation Registry. J Clin Oncol. 2011;29:1342–8.
Locke FL, Miklos DB, Jacobson CA, Perales MA, Kersten MJ, Oluwole OO, et al. Axicabtagene ciloleucel as second-line therapy for large B-Cell lymphoma. N Engl J Med. 2021. 14 Dec, Online ahead of print.
Nastoupil LJ, Jain MD, Feng L, Spiegel JY, Ghobadi A, Lin Y, et al. Standard-of-care Axicabtagene Ciloleucel for relapsed or refractory large B-cell lymphoma: results from the US Lymphoma CAR-T Consortium. J Clin Oncol. 2020;38:3119–28.
Neelapu SS, Locke FL, Bartlett NL, Lekakis LJ, Miklos DB, Jacobson CA, et al. Axicabtagene Ciloleucel CAR-T cell therapy in refractory large B-cell lymphoma. N Engl J Med. 2017;377:2531–44.
Pfreundschuh M, Kuhnt E, Trumper L, Osterborg A, Trneny M, Shepherd L, et al. CHOP-like chemotherapy with or without rituximab in young patients with good-prognosis diffuse large-B-cell lymphoma: 6-year results of an open-label randomised study of the MabThera International Trial (MInT) Group. Lancet Oncol. 2011;12:1013–22.
Schmitz N, Nickelsen M, Ziepert M, Haenel M, Borchmann P, Schmidt C, et al. Conventional chemotherapy (CHOEP-14) with rituximab or high-dose chemotherapy (MegaCHOEP) with rituximab for young, high-risk patients with aggressive B-cell lymphoma: an open-label, randomised, phase 3 trial (DSHNHL 2002-1). Lancet Oncol. 2012;13:1250.
Schuster SJ, Bartlett NL, Assouline S, Yoon SS, Bosch F, Sehn LH, et al. Mosunetuzumab induces complete remissions in poor prognosis non-Hodgkin lymphoma patients, including those who are resistant to or relapsing after chimeric antigen receptor T-cell (CAR-T) therapies, and is active in treatment through multiple lines. Blood. 2019a;134:6.
Schuster SJ, Bishop MR, Tam CS, Waller EK, Borchmann P, McGuirk JP, et al. Tisagenlecleucel in adult relapsed or refractory diffuse large B-cell lymphoma. N Engl J Med. 2019b;380:45–56.
Sehn LH, Herrera AF, Flowers CR, Kamdar MK, McMillan A, Hertzberg M, et al. Polatuzumab vedotin in relapsed or refractory diffuse large B-cell lymphoma. J Clin Oncol. 2020a;38:155–65.
Sehn LH, Hertzberg M, Opat S, Herrera AF, Assouline SE, Flowers C, et al. Polatuzumab vedotin plus bendamustine and rituximab in relapsed/refractory diffuse large B-cell lymphoma: updated results of a phase Ib/II randomized study and preliminary results of a single-arm extension. Blood. 2020b;136:17–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2022 The Author(s)
About this chapter
Cite this chapter
Glass, B., Kersten, M.J. (2022). Diffuse Large B Cell Lymphoma and Primary Mediastinal Lymphoma. In: Kröger, N., Gribben, J., Chabannon, C., Yakoub-Agha, I., Einsele, H. (eds) The EBMT/EHA CAR-T Cell Handbook. Springer, Cham. https://doi.org/10.1007/978-3-030-94353-0_12
Download citation
DOI: https://doi.org/10.1007/978-3-030-94353-0_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-94352-3
Online ISBN: 978-3-030-94353-0
eBook Packages: MedicineMedicine (R0)