Abstract
A short introduction to the use of whole-body hyperthermia (WBH) in oncology is provided. The main focus is on fever-range whole-body hyperthermia (FRWBH), since various preclinical studies have shown promising results using this approach. However, FRWBH has not been comprehensively investigated in clinical oncology trials. Having provided an overview on the methods to induce WBH, we will summarize preclinical and clinical data on the mode of action of FRWBH. The latter treatment positively affects the tumor micromilieu, especially by decreasing tumor hypoxia. It has the potential to enhance tumor-directed immune reactions and has proven anti-depressive and potential analgesic effects in patients without cancer. These pleiotropic effects align with good tolerability and high acceptability by patients. Given the available evidence, we argue that FRWBH should be investigated as an adjunct to modern cancer treatments in controlled clinical trials.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- Whole-body hyperthermia
- Fever-range hyperthermia
- Oncological hyperthermia
- Immunotherapy
- Tumor micromilieu
1 Introduction
A key property of malignant tissue is its potential to metastasize. The major obstacle to obtain long-term curation in cancer entities with the highest incidence of metastasis such as breast, prostate, colorectal, and lung is distant metastases. Approximately 90% of cancer-related deaths are due to metastatic disease. Metastases can occur synchronously at the time of tumor diagnosis or metachronously, i.e., during follow-up after initial treatment with curative intent. Hyperthermia (HT) is well known to enhance the therapeutic ratio of radiotherapy and chemotherapy. The term “hyperthermia” is often not clearly defined. The most frequently applied capacitive or radiative hyperthermia devices aim for a local or locoregional improvement of tumor control and potentially also a moderate decrease of metachronous distant metastases by stopping the formation of metastases at its source. In contrast, whole-body hyperthermia (WBH) aims to increase the temperature within the whole organism. Consequently, this mode of action could improve locoregional and also systemic therapies. Three levels of WBH can be distinguished, depending on the targeted body core temperature: mild WBH temperatures below 38.5 °C, moderate WBH temperatures between 38.5 and 40.5 °C, which is also denoted as fever-range WBH (FRWBH), and extreme WBH temperatures above 40.5 °C.
Out of the plethora of investigated agents, platin derivates, especially cisplatin, are the most comprehensively studied chemotherapeutic agents regarding thermo-enhancement. Urano et al. were able to show that thermal enhancement can already be observed with slight temperature increases up to 39 °C, but that a much stronger thermal enhancement ratio (TER) was observed with temperatures above 41 °C [1]. This was the rationale to implement WBH into early clinical trials in which an enhanced cytotoxic effect against distant metastases was envisaged. Since most trials focused on TER, the aim was to achieve body core temperatures as high as clinically achievable. Therefore, most clinical trials on WBH investigated extreme WBH, i.e., with targeted body core temperatures of 41–41.5 °C. However, extreme WBH is difficult to apply, bears important risks, and is quite expensive. Patients need to be sedated and often even ventilated. Close, invasive cardiovascular monitoring and narcosis must be performed by experienced anesthesiologists. At the same time, patients with cancer often present with poor general health and relevant cardiovascular comorbidities. Extreme WBH has therefore only been investigated in non-randomized phase I or phase II clinical trials and does not appear to deliver practice-changing results. Lassche et al. summarized the available evidence for this kind of treatment in a recent review and concluded that “...as modern oncology offers many less invasive treatments options, it is unlikely WBH will ever find its way in routine clinical care” [2].
Given these data, extreme WBH currently does not seem to have a major role in oncology. However, FRWBH might be an attractive adjunct to modern oncological treatment strategies as this kind of treatment is usually well tolerated. In the following, we will therefore mainly focus on FRWBH, since preclinical studies and early clinical trials in oncology and in non-oncological diseases showed promising results for this approach.
2 Techniques for Whole-Body Hyperthermia (WBH)
Various methods can be used to induce WBH in patients. Some authors argue that fever induction by mistletoe can also be regarded as a method to induce fever-like temperatures. However, an important difference between inducing WBH by technical devices and mistletoe is that the latter induces endogenous fever, whereas externally induced WBH induces the body to activate a plethora of processes to maintain homeostasis. These two approaches should therefore have distinctly different effects on organ-specific perfusion rates.
There are three frequently applied methods to induce WBH by medical devices, the most common of which being used currently is water-filtered Infrared-A irradiation (wIRA) (see Chap. 11, this book).
3 Effects of Fever-Range WBH
FRWBH has highly pleiotropic effects, many aspects of which, especially those relating to the tumor microenvironment (TME) and the immune system, are tightly interwoven. This might also be the case for its psychological effects and the influence of these on immune function. Nonetheless, for didactical reasons, we propose the following subdivision for the FRWBH effects.
3.1 Effects on the Tumor Microenvironment (TME)
FRWBH has been studied in various preclinical models. The laboratories of Elizabeth Repasky and Sharon Evans in Buffalo, NY (USA), have provided substantial data on the mechanisms of FRWBH in preclinical oncology models. They showed that FRWBH reduced the interstitial fluid pressure within an established head and neck squamous cell carcinoma (HNSCC) and in a patient-derived xenograft model. The reduced interstitial fluid pressure is followed by an increased tumor perfusion and thus oxygen supply, and consecutively reduced tumor hypoxia. Since tumor hypoxia is a well-known negative prognostic factor in oncology, especially given its ability to confer resistance to radiotherapy, FRWBH increased the efficacy of radiotherapy in vivo [3]. The same effect could be demonstrated in vivo using murine models of colon cancer and melanoma. The decreases in interstitial fluid pressure and tumor hypoxia were relatively long-lasting and were still apparent 24 hours after the application of FRWBH [4]. Another group was able to show that local heating with mild temperatures decreases tumor hypoxia in a murine breast cancer model, as measured by dedicated small animal positron emission tomography (PET) scans [5]. However, it is difficult to draw a conclusion for the impact of FRWBH from this study since the influence on perfusion is probably very different for local or whole-body heating. Nonetheless, the effect of FRWBH on tumor perfusion has been shown in a case report of a patient with a huge (14 cm) head and neck squamous cell carcinoma lymph node metastasis of an unknown primary. The patient was treated within a prospective pilot trial of FRWBH (Clinicaltrials.gov ID: NCT0189677) and received curatively intended definitive chemoradiation. Additional computed tomography (CT) scans to assess tumor perfusion were performed and showed a pronounced increase in tumor perfusion immediately after FRWBH which remained on a higher level for 5 days following FRWBH treatment [6]. The patient showed rapid tumor shrinkage and remained locoregionally controlled at the last follow-up visit 2 years after the end of treatment. One limitation of this case, besides being only one case, is that tissue immunohistochemistry (IHC) revealed cells with positive p16 staining. p16 is a surrogate for human papillomavirus (HPV)-induced HNSCC. These tumors present relatively favorable outcome, even in locally advanced stages, especially due to their high sensitivity to radiation. Therefore, it cannot be ruled out that the observed effect is, at least partly, tumor-specific and not related to FRWBH.
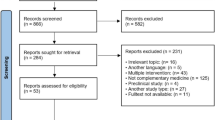
Although HPV-associated HNSCCs have relatively good prognosis even in locally advanced stages, the opposite holds true for HPV-negative HNSCC that recur after initial radiotherapy/chemoradiation. In this setting, re-irradiation is a frequently chosen approach, but is usually only able to achieve short-term palliation since the re-irradiation dose is limited due to prior dose exposure of surrounding at-risk organs and due to the usually high radioresistance of recurrent tumors. This was the rationale to initiate a prospective trial on re-irradiation of locally recurrent HNSCC in combination with FRWBH (Clinicaltrials.gov ID: NCT03547388). The trial included sophisticated hypoxia-PET examinations and perfusion imaging by magnetic resonance imaging (MRI). The intention was to repeat hypoxia-PET-MRI during treatment to provide clinical data on the anti-hypoxia effect of FRWBH. The trial recruited all 10 planned patients, eight of which had additional PET and seven additional MRI imaging. Surprisingly, baseline examinations revealed an absence of PET-detectable hypoxia and very heterogeneous blood flow behavior in recurrent tumors [7]. Figure 8.1 shows representative patient examples. Therefore, no conclusions on the effect of FRWBH on tumor hypoxia and perfusion could be drawn in this cohort. Nonetheless, in an exploratory analysis, patients who received at least three FRWBH treatments concomitant with re-irradiation showed a potential improvement of locoregional tumor control [8].
Example of three patients treated with FRWBH plus re-irradiation for recurrent head and neck squamous cell carcinomas. FDG-PET CT (upper row) shows high glucose uptake of all tumors, while MRI (middle row) and hypoxia-related PET (lower row) do not show relevant tumor hypoxia or perfusion restriction. Image taken from [7]
3.2 Effects on the Immune System
Temperature is a key element for the immune system of vertebrates, and a large amount of preclinical data have shown the importance of HT and FRBWH on anti-tumor immunology. HT enhances both cellular and humoral immune responses by several mechanisms. It increases natural killer (NK) cell function, the trafficking of cytotoxic T cells to tumors, the functional activity of macrophages and dendritic cells (DCs), and the production of pro-inflammatory cytokines. The data are comprehensively summarized in two review articles [9, 10]. Various groups have been able to demonstrate that FRWBH positively influences immune responsiveness, especially in cancer. Preclinical in vivo studies by the group of Joan Bull in Houston, TX (USA), were able to show that fever-range hyperthermia has the potential to foster anti-tumor immune responses without increasing normal tissue toxicity—short-term extreme WBH caused severe damage to normal tissue [11]. This led to a first clinical trial to investigate the efficacy of combining cytostatic agents plus interferon-alpha with FRWBH in patients with different metastatic diseases [12]. This trial was performed in the pre-immune checkpoint era, and this approach was unfortunately not pursued despite promising results regarding response rate and patient-reported quality of life. A recent retrospective analysis of 131 patients with stage IV solid cancers that had failed to respond to all conventional therapies and were treated with checkpoint inhibition and FRWBH has shown that the treatment was well tolerated, and response and progression-free survival rates were very promising, especially considering the unfavorable prognosis of the patient cohorts. However, one important limitation is the magnitude of interventions within these patients: Patients did not receive standard doses of checkpoint inhibition, only low-dose ipilimumab (CTLA-4, 0.3 mg/kg instead of 1.0 mg/kg). In addition, several other co-interventions were performed: additional locoregional HT and also interleukin 2 administration [13]. Although this hampers any conclusions on the potential use of each single intervention, it does highlight the potential to improve current immunotherapeutic approaches.
Prospective trials that combine immunotherapy with HT are therefore warranted. With respect to combining immunotherapy and HT, currently three studies have investigated this combination. Two studies are non-randomized trials undertaken in China that have used the Thermotron RF-8EX capacitive hyperthermia device. Both studies combine checkpoint inhibition, cellular immunotherapy, and HT in either mesothelioma or various abdominal/pelvic malignancies (Clinicaltrials.gov ID: NCT03757858 and NCT03393858). Another non-randomized phase-Ib/II clinical study in France has investigated intraperitoneal checkpoint inhibition in combination with hyperthermic intraperitoneal chemotherapy in patients with advanced ovarian carcinoma (Clinicaltrials.gov ID: NCT03959761). So far, no clinical trial on combining checkpoint inhibition and FRWBH has been started.
3.3 Psychoneurological Effects
In the non-oncology setting, a small, randomized, double-blind study in patients with major depressive symptoms revealed a long-lasting anti-depressive effect of single-session FRWBH compared with sham HT in the control [14]. This positive trial increased interest in FRWBH in the psychiatry community, and several ongoing trials are investigating the use of FRWBH for treating depressive disorders, some of which are combining FRWBH with pharmacological treatment. Since depressive symptoms are prevalent among cancer patients, this might be an additional important benefit of FRWBH in the oncology setting. In this regard, it has been shown that an effective decrease of depressive symptoms was associated with improved survival in patients with metastatic breast cancer [15].
FRWBH also appears to have positive effects on nociception—the neural processes of encoding and processing noxious stimuli. A small randomized clinical trial has shown FRWBH to significantly alleviate nonspecific lumbar back pain in patients receiving multimodal pain therapy [16]. Two other studies, one of them randomized, have also shown the potential of FRWBH to improve symptoms of fibromyalgia [17, 18]. Since pain is a frequent symptom of advanced-stage cancer, this might be another desirable effect of FRWBH in the oncology setting (see Chap. 11, this book).
3.4 Other Effects Possibly Relevant in Oncology
An interesting preclinical study in mice revealed the potential of FRWBH to ameliorate severe neutropenia and induce a more rapid recovery from neutropenia after total body irradiation compared to control mice [19]. This is a very encouraging finding given that neutropenia is one of the most frequently observed severe side effects of chemotherapy and chemoradiation which is potentially life-threatening and hampers the administration of additional cycles of chemotherapy. However, this finding has not yet been corroborated in clinical trials.
Although FRWBH is also very likely to have a strong impact on the composition of the gut microbiome [20] which is known to influence therapeutic response to conventional cancer therapy and immunotherapy, preclinical and clinical data in this area are currently lacking. Figure 8.2 summarizes the pleiotropic effects of FRWBH in the oncology setting.
4 Conclusions
We are currently witnessing dramatic changes in the paradigms for the treatment of cancer. Although radiotherapy has always been regarded as a local treatment that aims to kill all viable tumor cells within the irradiated target volume, the advent of novel immunotherapies has somewhat shifted this paradigm. Abscopal radiation responses, i.e., responses outside the irradiated field, and radiation-induced boosting of immunotherapy by generating neoantigens are gaining interest and have led to several ongoing clinical trials that pursue this unconventional radiotherapy approach. The same might be the case with (whole-body) hyperthermia. In 1987, van der Zee summarized the knowledge of that time as follows: “In view of the fact that immunological factors in tumor therapy do not play a significant role..., it is likely that the elevated temperatures have been instrumental” [21]. This reflects the strong impact of hyperthermia on classical TER of cytostatic drugs and radiotherapy in the past. Nowadays, we know that immunological factors play a pivotal role in oncology and it is noteworthy to mention that the pioneers of preclinical FRWBH were immunologists or oncologists having a strong focus on tumor immunology.
Abbreviations
- CT:
-
Computed tomography
- FRWBH:
-
Fever-range whole-body hyperthermia
- HNSCC:
-
Head and neck squamous cell carcinomas
- HPV:
-
Human papillomavirus
- HT:
-
Hyperthermia
- MRI:
-
Magnetic resonance imaging
- PET:
-
Positron emission tomography
- TER:
-
Thermal enhancement ratio
- WBH:
-
Whole-body hyperthermia
References
Urano M, Kahn J, Kenton LA. The effect of cis-diamminedichloroplatinum(II) treatment at elevated temperatures on murine fibrosarcoma, FSa-II. Int J Hyperthermia. 1990;6:563–70.
Lassche G, Crezee J, van Herpen CML. Whole-body hyperthermia in combination with systemic therapy in advanced solid malignancies. Crit Rev Oncol Hematol. 2019;139:67–74.
Winslow TB, Eranki A, Ullas S, et al. A pilot study of the effects of mild systemic heating on human head and neck tumour xenografts: analysis of tumour perfusion, interstitial fluid pressure, hypoxia and efficacy of radiation therapy. Int J Hyperthermia. 2015;31:693–701.
Sen A, Capitano ML, Spernyak JA, et al. Mild elevation of body temperature reduces tumor interstitial fluid pressure and hypoxia and enhances efficacy of radiotherapy in murine tumor models. Cancer Res. 2011;71:3872–80.
Myerson RJ, Singh AK, Bigott HM, et al. Monitoring the effect of mild hyperthermia on tumour hypoxia by Cu-ATSM PET scanning. Int J Hyperthermia. 2006;22:93–115.
Rich LJ, Winslow TB, Alberico RA, et al. Enhanced tumour perfusion following treatment with water-filtered IR-A radiation to the thorax in a patient with head and neck cancer. Int J Hyperthermia. 2016;32:539–42.
Rogasch J, Beck M, Stromberger C, et al. PET measured hypoxia and MRI parameters in re-irradiated head and neck squamous cell carcinomas: findings of a prospective pilot study. F1000Res. 2021;9:1350.
Zschaeck S, Weingärtner J, Ghadjar P, et al. Fever range whole body hyperthermia for re-irradiation of head and neck squamous cell carcinomas: final results of a prospective study. Oral Oncol. 2021 May;116:105240. https://doi.org/10.1016/j.oraloncology.2021.105240.
Repasky EA, Evans SS, Dewhirst MW. Temperature matters! And why it should matter to tumor immunologists. Cancer Immunol Res. 2013;1:210–6.
Evans SS, Repasky EA, Fisher DT. Fever and the thermal regulation of immunity: the immune system feels the heat. Nat Rev Immunol. 2015;15:335–49.
Sakaguchi Y, Makino M, Kaneko T, et al. Therapeutic efficacy of long duration-low temperature whole body hyperthermia when combined with tumor necrosis factor and carboplatin in rats. Cancer Res. 1994;54:2223–7.
Bull JMC, Scott GL, Strebel FR, et al. Fever-range whole-body thermal therapy combined with cisplatin, gemcitabine, and daily interferon-alpha: a description of a phase I-II protocol. Int J Hyperthermia. 2008;24:649–62.
Kleef R, Nagy R, Baierl A, et al. Low-dose ipilimumab plus nivolumab combined with IL-2 and hyperthermia in cancer patients with advanced disease: exploratory findings of a case series of 131 stage IV cancers - a retrospective study of a single institution. Cancer Immunol Immunother. 2020;70(5):1393–403.
Janssen CW, Lowry CA, Mehl MR, et al. Whole-body hyperthermia for the treatment of major depressive disorder: a randomized clinical trial. JAMA Psychiatry. 2016;73:789–95.
Giese-Davis J, Collie K, Rancourt KMS, et al. Decrease in depression symptoms is associated with longer survival in patients with metastatic breast cancer: a secondary analysis. J Clin Oncol. 2011;29:413–20.
Ettrich U, Konrad B, Prate K, et al. Mild whole body hyperthermia in combination with inpatient multimodal oriented pain therapy: evaluation in patients with chronic unspecific lumbar back pain. Orthopade. 2014;43:165–74.
Romeyke T, Scheuer HC, Stummer H. Fibromyalgia with severe forms of progression in a multidisciplinary therapy setting with emphasis on hyperthermia therapy-a prospective controlled study. Clin Interv Aging. 2015;10:69–79.
Brockow T, Wagner A, Franke A, et al. A randomized controlled trial on the effectiveness of mild water-filtered near infrared whole-body hyperthermia as an adjunct to a standard multimodal rehabilitation in the treatment of fibromyalgia. Clin J Pain. 2007;23:67–75.
Capitano ML, Nemeth MJ, Mace TA, et al. Elevating body temperature enhances hematopoiesis and neutrophil recovery after total body irradiation in an IL-1-, IL-17-, and G-CSF-dependent manner. Blood. 2012;120:2600–9.
Hylander BL, Repasky EA. Temperature as a modulator of the gut microbiome: what are the implications and opportunities for thermal medicine? Int J Hyperthermia. 2019;36:83–9.
Field SB, Franconi C, editors. Physics and technology of hyperthermia. Amsterdam: Springer; 1987.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2022 The Author(s)
About this chapter
Cite this chapter
Zschaeck, S., Beck, M. (2022). Whole-Body Hyperthermia in Oncology: Renaissance in the Immunotherapy Era?. In: Vaupel, P. (eds) Water-filtered Infrared A (wIRA) Irradiation. Springer, Cham. https://doi.org/10.1007/978-3-030-92880-3_8
Download citation
DOI: https://doi.org/10.1007/978-3-030-92880-3_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-92879-7
Online ISBN: 978-3-030-92880-3
eBook Packages: MedicineMedicine (R0)