Abstract
Contact-free temperature determination is based on the measurements of electromagnetic radiation. The corresponding physical laws are related to the properties of black bodies. This background allows for the development of thermometric and thermographic systems for remote temperature measurements. Precise absolute temperature data, required in hyperthermia, do not only depend on the technical quality of the systems (hardware and software) and their calibration, but also depend on accurate determination of the emissivity of human skin. Pyrometers are restricted to temperature measurements within a small area (measurement spot), while thermographic cameras allow measurements across a relatively large region on the target area in real time. The subdivision of the IR image into spatially separated pixels allows access to temperature data of small areas on the skin and thus combines thermometry and thermography. Quality assurance standards of the European Society of Hyperthermic Oncology for water-filtered IR-A-hyperthermia (wIRA-HT) are met, except for the accuracy of the absolute temperature. Since the relation between the temperatures at the skin surface and in deeper tissue layers, considering irradiation and heating time, in wIRA-HT can be assessed, the temperature needed for efficient thermal treatment of superficial tumors within superficial tissue layers can therefore be achieved in a controlled manner.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- Water-filtered infrared A (wIRA)
- IR thermometry
- IR thermography
- Superficial hyperthermia
- Contact-free hyperthermia
- ESHO guidelines
1 Introduction
As the success of locoregional hyperthermia is crucially dependent on the temperature attained in the tissue, e.g., in superficial tumors, reliable temperature measurements are mandatory. The approach for measuring temperature depends on how hyperthermia is performed. In microwave hyperthermia, the skin surface is not directly accessible as a water bolus is used to transfer heat from the microwave applicator to the patient. In this case, thermometry probes are inserted within catheters that are placed in the target region, or a sensor array is pulled through a fixed trajectory during treatment to improve spatial temperature resolution. As recently reported, a 56-sensor thermal monitoring sheet, which is placed on the skin of the patient and provides a spatial temperature resolution of 20 × 25 mm, has been developed [1].
Hyperthermia with water-filtered infrared-A irradiation (wIRA-HT) allows contact-free heating of the tissue and thus also contact-free temperature measurements at the skin surface. This provides the option to use both thermometric and thermographic systems. Although thermometric systems are limited to temperature measurements within a relatively small measuring spot, the latter have the advantage that thermal variations or heat patterns across a surface can be depicted in a visual image and can be controlled. The spatial temperature resolution is <1 mm. For precise temperature measurements with these systems, some parameters need to be considered. Among these, and probably the most important one, is the emissivity of the patient’s skin being irradiated. Although IR temperature measurements are basically related to the skin surface of the patient, these data can be used to estimate temperatures in underlying tissue layers and thereby prevent overheating and replace invasive temperature measurements.
2 Physical Background of Contact-Free Temperature Measurements
2.1 Basic Laws and Parameters
Any material with a temperature above the absolute zero point (0 K, -273.15°C resp.) emits and absorbs electromagnetic radiation, the nature of which strongly depends on its composition and its surface properties, and its description may require complex physical formulae. For simplification, it has proven to be helpful in practice to use an idealized body for which the radiation laws are precisely known and adapt them to those of real bodies [2]. The idealized body is called black body or black body radiator, which absorbs all incident electromagnetic radiation of all wavelengths and emits it again in a characteristic spectrum, which is only dependent on its temperature, whereas real bodies, called gray bodies, emit less radiation than absorbed.
A helpful parameter, which combines the properties of a black body with those of a gray body, is the emissivity, defined as follows:
Since a black body emits the entire incident radiation again, ε(λ, T) = 1, the emissivity of a real body is <1. Further parameters are defined accordingly.
Because of the conservation of energy
These are the laws and parameters on which all systems are based and which are used for measuring temperature using infrared radiation, e.g., IR cameras and IR thermometers (pyrometers).
Wien’s displacement law can be used to find the optimal range of wavelengths for temperature measurements. Figure 4.1 shows that the wavelengths of the maxima of the curves, indicating maximal spectral radiant exitance, are shifted to smaller wavelengths as temperature increases. This is mathematically expressed by Wien’s displacement law:
where λmax= maximum wavelength [m], b = 2.898 · 10−3 [mK] Wien’s displacement constant, and T = absolute temperature [K].
Spectral radiant exitance of a black body as a function of wavelength for temperatures of 100 °C (1), 37 °C (2), and 0 °C (3). According to Wien’s displacement law, the maxima of the spectral exitance are at 7.766 μm (100 °C), at 9.435 μm (34 °C), and at 10.609 μm (0 °C). Integration of the spectral data over the wavelengths results in radiant exitance values of ≈316 Wm−2 (100 °C), ≈505 Wm−2, and ≈316 Wm−2 (0 °C) in accordance with data calculated by using the Stefan–Boltzmann’s law (see Eq. 4.8)
According to this law, the wavelength of electromagnetic radiation emitted by human skin surface with a temperature of 34 °C, at which the maximum of spectral radiant exitance is reached, is at about 9.435 μm (infrared-C range (3–1000 μm)), as shown in Fig. 4.1. The radiant exitance M, emitted from a black body, as a function of its temperature, is described by Stefan–Boltzmann’s law:
where σ = 5.67 · 10−8 Wm−2 ·K−4 (Stefan–Boltzmann constant) and T = absolute temperature [K].
Manufacturers of IR systems supply the basic formulae required for measurements with their systems in a general form, as they are interested in applications in many fields [2,3,4]. Therefore, these formulae need to be adapted to a specific metrological situation. In the following, the arrangement for wIRA-HT in the clinical setting is taken as the basis and the general formulae are adjusted accordingly (Fig. 4.2).
Scheme for measurement of skin surface temperature during wIRA-hyperthermia using an IR camera or a pyrometer. T0 = temperature of the skin area of the patient that is irradiated, TP = temperature within the measurement section, TU = temperature of the environment, ε = emissivity of the patient’s skin, ρ = reflectance of human skin, τP = transmission of the measurement section
wIRA irradiation (780–1400 nm) is partially absorbed by the patient’s skin and partially reflected and remitted into the measurement section, i.e., the space between the patient and the IR system. This directly reflected, and remitted radiation is not perceived by the IR system because its maximal wavelength is at 1.4 μm and the lens of these systems transmits only radiation with wavelengths >7.5 μm. Radiation from objects at room temperature (21 °C), reflected by the patient, is measured, because the wavelength of this radiation is about 10 μm according to Wien’s displacement law.
2.2 Derivation of the Basic Equation for Temperature Measurement
Assuming human skin would have the properties of a black body, the radiation emitted by the patient could be defined as ΦS(T0). However, as skin is a gray body, it is reduced to Φε = ε · ΦS(T0). Thermal radiation also reaches the patient from the environment and is partially absorbed, contributing to the heating of the patient, and partially reflected. The total radiant power from the environment is assumed to be ΦTU. A portion of this, Φρ = ρ · Φ(TU), is reflected and enters the measurement section. The total radiant power, ε · Φ(T0) + ρ · Φ(TU), entering the measuring section, is attenuated by the transmittance τP of the section. It remains
The measurement section with the temperature TP can also emit radiation Φ(TP). As there is no reflection (ρ = 0), the additional radiant power is (1 − τP)Φ(TP), taking into consideration:
For temperature measurement, the following radiant power is available:
Because of ε + ρ = 1 and ρ = 1 − ε, the formula can be modified to:
This quantity is measured by the IR system, i.e., transferred into an electrical signal. The parameter required is the temperature T0. Since there is basically no direct measurement of the temperature, the signal needs to be assigned to temperature values in the IR system, taking into consideration that the temperatures in the formulae presented above are absolute temperatures.
Related to (4.12), the following parameters have to be taken into account in order to calculate the patient’s skin surface temperature: τp, ε, TU, and Tp .
The transparency of the air in the measurement section, τp, depends on the wavelength. Within the region of 8–14 μm, the transparency is constant and high. Since IR measurement systems register wavelengths between 7.5 and 13 μm, one can assume that the radiation from the patient is not influenced by the measurement section.
Because of Φ(TP) = 0 and τP = 1, the formula for Φ(T0) is reduced to
where Ф−1 is the inverse function of Φ(T0).
Emissivity ε of the patient’s skin and the temperature of the environment, TU, are the key parameters. TU is the mean temperature of the inner surface of the half-sphere around the patient, and it is not the temperature of the ambient air. It is almost impossible to completely eliminate the contribution from the materials/persons surrounding the optical path and the detector. However, due to the relatively high emissivity of the skin, this contribution is low. The emissivity of the patient is the crucial parameter and depends on tissue properties (e.g., normal tissue, tumor tissue) and the skin condition. The emissivity of the skin must be determined and set in the IR system before each measurement (see below).
2.3 Determining the Emissivity of Human Skin
2.3.1 Reference Temperature
The temperature at a certain point in the target area is measured by a contact thermometer and thereafter at the same place with an IR measurement system. The emission coefficient displayed in the IR measurement system is then adjusted accordingly, until the temperature of the contact thermometer is reached. However, the use of contact thermometers is not practical in cases of ulceration or wet skin surfaces due to the following issues: (a) feedback effect of the contact thermometer on the skin, (b) heat transfer between skin and the contact thermometer, and (c) heat transfer between the contact thermometer and its environment [5].
2.3.2 Reference Emissivity
There are materials whose emissivity is known (i.e., lacquer or foil). Such a material must be applied to the skin as a reference area. The emissivity in the IR measurement system is set accordingly. When the reference area has reached the temperature of the skin, the temperature can be measured with the IR measurement system. After that, the temperature is measured at a different spot on the skin and the emissivity in the IR measurement system is adjusted until the same temperature is reached. The displayed emissivity value is the emissivity of the skin.
2.3.3 The Use of a Black Body to Measure Skin Temperature
As mentioned above, the emissivity of a black body is 1. The temperature of commercially available black bodies can be reliably set to different temperatures. To calibrate an IR measurement system, the emissivity in the instrument is set to 1 and the system is focused on the reference area of the black body—it should display the same temperature. If not, an internal adjustment of the instruments is necessary. In case of matching, the emissivity in the instrument is set to 0.98, which is generally accepted for healthy skin, and 0.87 for tumor tissue. The general problem is that this could not be the “true” emissivity of the skin.
3 The Thermographic Camera (Syn.: Infrared Camera, Thermal Imaging Camera, Thermal Imager)
3.1 Basic Mode of Operation
An IR camera is similar to a common digital video camera. Instead of visible radiation (400–700 nm), the thermographic camera creates an image using infrared radiation (1–14 μm). In the medical field, a range between 8 μm and 14 μm is preferred as explained above. The IR camera consists of a lens that focuses IR onto a focal plane array (FPA) detector, the “heart” of the camera. This detector transforms infrared radiation into an electrical signal and is designed as a chip with microbolometers (resistance thermometers), which are arranged in an array of lines and columns. In this way, the entire thermographic image is subdivided into separated pixels, which allow for access to the respective signals (temperatures). The levels of the measurement signal are assigned to colors for better discrimination of the temperature values (Fig. 4.3).
3.2 Performance Criteria
3.2.1 The Spectral Region
As mentioned above, the wavelength of radiation from human skin at a temperature of 37 °C, at which maximal irradiation is reached, is at 9.344 μm. To capture all electromagnetic radiation emitted by a patient, the lens of the camera must be transparent for this wavelength, and the whole spectrum that is transmitted should be small to block interfering radiation from the environment.
3.2.2 Thermal Resolution, Relative and Absolute Accuracy
Small differences in temperature can be lost due to noise in the detector signal. As a measure of a camera’s capacity to differentiate small temperature differences, the noise equivalent temperature difference (NETD) describes the change in temperature, which is equivalent to the effective noise of the system. It can be referred to as the minimal resolvable temperature change. This value only reflects the relative accuracy of the system, not the absolute accuracy. Usually, NETD values are between <30 mK and <40 mK. According to the ESHO Quality Guidelines, the value for IR systems should be <50 mK [6].
The value for absolute accuracy, as specified by the manufacturers, is commonly ±2 K or 2% of the reading. This information is the result of a widely used uncertainty analysis technique called root sum of squares and considers partial errors for each variable in the temperature measurement Eq. (4.13) (e.g., emissivity and reflected radiation from the environment), the camera response, and the accuracy of the calibration tool used. The total uncertainty UT then is calculated according to the error propagation law:
where ΔT1, ΔT1, ΔT1…are the single errors of the parameters mentioned above [7].
Whereas NETD is essentially a question of technology, absolute accuracy is a basic problem of the uncertainty of absolute temperature measurements, enhanced by the uncertainty of the emissivity. This is crucial for hyperthermia applications. If 42 °C is measured during hyperthermia treatment instead of the real temperature T = 44 °C, then tissue damage can occur. The only practical way for reliable absolute temperature measurements is for the manufacturer and the operator to calibrate the system as carefully as possible. Uncertainties in the heating concept are to be considered. The ESHO Quality Assurance Guidelines [6] require the precision of the temperature measurement to be 0.1 °C, which can hardly be reached, especially since emissivity is associated with it.
3.2.3 Geometric Resolution (Syn.: Optical Resolution, Spatial Resolution)
The geometric resolution indicates the size of the smallest detail (area) on the skin surface, which is visible in the IR image. It can be interpreted as the smallest area on the skin surface related to a single bolometer (pixel) of the camera detector, which can be detected at a set distance, providing temperature data, relevant for the detection of hot spots in, above, and around scars or the separation of two structures close together. This resolution is determined by the number of pixels per area unit on the camera detector and depends on the lens used. Calculation of the resolution is based on the parameter field of view, which is the largest area the camera can capture at a set distance and is typically characterized by the vertical and horizontal angle under which the area appears from the camera detector. Since this value is very important, its calculation will be shown using an example.
Camera: optris PI 400 (MTS Messtechnik Schaffhausen, Stein am Rhein, Switzerland), number of pixels on the camera chip: 382 (horizontal) x 288 (vertical), focal length of the lens: 15 mm, horizontal view angle αh: 38°, and vertical view angle αv: 29° (data supplied by the camera manufacturer).
The horizontal viewing angle can be expressed as \( {\alpha}_h=2\cdotp \mathit{\arctan}\left(\frac{h}{2\cdotp f}\right) \). According to Fig. 4.4, the following relationships apply:
where g = object distance and b = half the object width.
Calculation of the geometric resolution of thermographic cameras [8]
The width of the area on the skin surface is 2b, and the distance between the IR camera and the patient is g = 34 cm. Then, the width of the area on the patient is
With 382 horizontal pixels, the smallest width that can be detected is \( \frac{23.4\ \mathrm{cm}}{382}=0.6\ \mathrm{mm} \). Since the pixels are squared, the smallest area on the skin surface, which can be captured, thus is 0.6 mm × 0.6 mm.
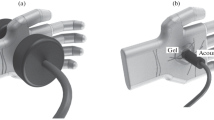
4 Pyrometer (IR Thermometer): Basic Mode of Operation
Compared to IR cameras, IR thermometers are simpler in design, but based on the same physical background, as described above. These thermometers can be characterized as remote thermometers. A lens captures the IR radiation from a measurement spot on the target surface and focuses it onto a detector (see Fig. 4.5). It is important that the emitting area is equal or larger than the measurement spot defined by the system. Different methods are used to mark this spot on the target surface, and these are preferably based on laser technology. For example, a crosshair is projected onto the surface with the size of the measurement spot. As with cameras, the emissivity must be entered [9].
5 Special Situations
5.1 Curved Surfaces
Two problems arise at curved skin surfaces: (a) wIRA-irradiation—and thus also tissue heating—is reduced by the cosine of the angle between the direction of the radiation and the surface normal, and (b) the area of this less heated surface onto the pixels of the camera is not completely imaged and leads to reduced temperature values (Fig. 4.6).
Reduced heating of the tissue at curved skin surfaces (a). Incomplete projection of a curved skin area onto the detector array of a thermographic camera (b) [8]
5.2 Optional Interventions During wIRA-HT
In wIRA-HT, the skin surface remains accessible for interventions. This allows for power deposition modulations by placing shielding sheets on the irradiated area to completely block non-target tissues and for modulations of the temperature measurement procedures. In the cases of ulcerated lesions or wound secretion, heat loss by evaporation can reduce the critical target region below the therapeutically required temperatures. In this case, covering with transparent grease or foils enables more uniform heating (see Fig. 4.7a).
Interventions during wIRA-HT. (a) Ulcerated recurrent breast cancer. The nodular tumors are fibrin-coated and permanently produce wound secretion. (b1) Due to evaporation, moist surfaces can cool the tissue below the therapeutically relevant temperature level (blue colour). (b2) Covering these areas with a thin film of greasy ointment (Bepanthen™) reduces evaporation. (b3) A more homogeneous heating is achieved. (c1) A hotspot (white arrow) outside the target area may disturb temperature control. (c2) The region is covered with opaque material (green arrow). (c3) The influence of the hot spot is prevented. Consequently, a hotspot within the target region (white arrow), where it needs to be recorded, is indicated
During wIRA-HT in the clinical setting, the highest temperature values (hot spots) within the entire irradiated area are registered automatically and are used for irradiation control to avoid tissue damage. In this case, hot spots outside the target area can be covered with opaque material to eliminate their influence, as shown in Fig. 4.7b.
6 Use of Thermographic Cameras for Temperature Measurements on Phantoms
The quality assurance standards of ESHO for water-filtered IR-A hyperthermia require measurements on phantoms [10]. The use of infrared thermography in superficial hyperthermia quality assurance, including measurements on phantoms, has been reported in detail [11]. Currently, there is no recipe for tissue-equivalent phantom materials that adequately consider absorption, scattering, and refraction of IR irradiation in tissues. Even were such a material to be identified, individual patient-related factors influencing heating need to be considered. Thus, the value of phantoms and the significance of measurements made on them must be viewed critically.
7 Relationship Between Temperatures Assessed at the Skin Surface and in Deeper Tissue Layers
In hyperthermia, it is crucial to reach the temperatures required to achieve therapeutic effects (39–43 °C). In the clinical setting, this means that (tumor) tissue temperatures at preset depths must reach predefined levels. IR-based temperature measurements can only measure the temperature at the skin surface, and thus, the question arises, whether there are any relationships between the surface temperature and the temperatures in deeper tissue layers. Recent in vivo studies on piglets have shown that maximum tissue temperatures exceeded corresponding temperatures on the skin surface by 1–2 K during wIRA-hyperthermia ([12], Fig. 4.1). Similar relations were found in vivo during wIRA exposure of human abdominal wall and lumbar region (Fig. 4.8). These data can be used for approximate estimations of maximum tissue temperatures if the temperature at the skin surface is monitored during wIRA-hyperthermia.
8 Conclusions
In wIRA-HT, contact-free heating enables remote temperature assessments by IR-based devices. The relationship between skin temperatures and temperatures in deeper tissue layers can be used to estimate and control the temperatures in tumors that are needed for therapeutic effects. Since the measurements are contact-free, in the clinical setting physicians can modulate/block heating at locations where it is not needed (e.g., in scar tissues, which tend to become hot spots), with opaque foils. Wet body surfaces can be covered with transparent material to reduce cooling by evaporation. Using software, mean temperature values related to definable areas can be provided and temperature data of individual spots can be displayed. Basically, there is high potential for image analysis to control and interpret the dynamic temperature distribution during heating.
References
Bakker A, Zweije R, Kok HP, et al. Clinical feasibility of a high-resolution thermal monitoring sheet for superficial hyperthermia in breast cancer patients. Cancers. 2020;12:3644.
Griesinger A. Einführung in die Theorie und Praxis der Infrarot-Thermografie. Dresden: InfraTec GmbH; 2004.
Clayton RK. Schulungsunterlagen, Einführung in Theorie und Praxis der Infrarot-Thermografie. 1 Physikalische Grundlagen. Dresden: InfraTec GmbH; 2012.
Trankler H-R, Reindl LM. Grundlagen der berührungslosen Temperaturmessung. Berlin: Optris GmbH; 2019.
MacRae BA, Annaheim S, Spengler CM, Rossi RM. Skin temperature measurement using contact thermometry: a systematic review of setup variables and their effects on measured values. Front Physiol. 2018;9:20180130. https://doi.org/10.3389/fphys.2018.00029.
Trefna HD, Creeze H, Schmidt M, et al. Quality assurance guidelines for superficial hyperthermia clinical trials: I Clinical requirements. Int J Hyperthermia. 2017;33:471–82.
Messgenauigkeit und -unsicherheit von Infrarotkameras einfach erklärt, FLIR Nürnberg, Germany; 2016.
Schimweg T. Thermographische Temperaturanalyse in Erwärmungsprozessen. Infrared temperature solutions (IST): Fachberichte. Keller HCW; 2017.
Infrarot Thermometer Ratgeber. Wie funktioniert ein Infrarot Thermometer (Pyrometer).
Trefna HD, Creeze H, Schmidt M, et al. Quality assurance guidelines for superficial hyperthermia clinical trials: II. Technical requirements for heating devices. Strahlenther Onkol. 2017;193:351–66.
Müller J. Infrared thermography in superficial hyperthermia quality assurance. Master thesis, Faculty of Physics. Division of Medical Radiation Physics, Department of Radiation Oncology, University Medical Center, Friedrich-Alexander-University Erlangen-Nuremberg; 2015.
Piazena H, Müller W, Pendl W, et al. Thermal field formation during wIRA-hyperthermia: temperature measurements in skin and subcutis of piglets as a basis for thermotherapy of superficial tumors and local skin infections caused by thermosensitive microbial pathogens. Int J Hyperthermia 2019;36:938–52.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2022 The Author(s)
About this chapter
Cite this chapter
Müller, W., Piazena, H., Thomsen, A.R., Vaupel, P. (2022). Thermography and Thermometry in wIRA-Hyperthermia. In: Vaupel, P. (eds) Water-filtered Infrared A (wIRA) Irradiation. Springer, Cham. https://doi.org/10.1007/978-3-030-92880-3_4
Download citation
DOI: https://doi.org/10.1007/978-3-030-92880-3_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-92879-7
Online ISBN: 978-3-030-92880-3
eBook Packages: MedicineMedicine (R0)