Abstract
Successful treatment of recalcitrant common hand and foot warts in a prospective randomized controlled blind trial using wIRA and PDT has been reported. In addition, in wound healing wIRA is mostly investigated in vitro based on the resolution of mechanical damage to confluent cell layers using the “scratch wound assay.” The latter enables the direct measurement of cell migration and regeneration of the cell layer. Preliminary studies for wIRA effects on wound closure in vitro have shown beneficial effects of single 10 min treatments. Although cellular processes induced and mediators involved still need to be elucidated, it is apparent that the observed clinical benefits of wIRA on wound healing can be investigated in vitro using adequate models and experimental settings. The next step is to employ 3D skin models for morphological investigations closely simulating in vivo conditions.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- wIRA (water-filtered infrared-A)
- Scratch wound assay
- 3D skin model
- Hand and foot warts
- Wound infection
- Wound healing
1 Clinical Effectiveness of wIRA in the Treatment of Warts
Water-filtered infrared-A (wIRA) irradiation is characterized by deep-reaching thermal effects with comparatively low level of heat-induced pain on the skin surface using typical irradiances (60–120 mW/cm2) [1, 2]. wIRA has been successfully employed in a broad range of areas including physiotherapy, sports medicine, internal medicine, pediatrics, as adjuvant therapy in radiation oncology, as well as in the treatment of chronic and acute wounds [3], and also for antimicrobial treatment ± photodynamic therapy (aPDT) [4, 5]. Previous studies have reported PDT to be efficient in warts [6, 7].
Warts are a common skin condition with an overall prevalence of 2.4–12.9% which are caused by the human papillomavirus (HPV) [8, 9]. Warts seriously impair quality of life due to possible functional impairment, pain, and unsightly appearance. As well as having a physical impact, the concern that warts might spread and/or lead to infections in other people has a negative psychological impact [9]. Although warts most commonly involve hands and feet, they can affect other areas of the skin including anogenital regions where they can manifest as sexually transmitted infections [8, 9]. Additional manifestations of HPV-associated diseases include several genital or upper respiratory/digestive malignancies such as cervical, vaginal, vulvar, penile, anal, and oropharyngeal cancers [8], the latter of which have been in the focus of most investigators in the HPV field [8]. In contrast, Fuchs et al. [4] have concentrated on the therapy of common warts (verrucae vulgares) and reported on the first prospective randomized controlled blind trial of PDT and wIRA in the treatment of recalcitrant common hand and foot warts. Although different therapeutic regimens for common warts have been described earlier, there is a lack of a single striking treatment strategy with high efficacy and little side-effects. Standard therapies such as cryotherapy or electrosurgery are invasive, cause burns, blisters, local irritation, itching, bleeding, infection, ulcers, and scarring, and/or are painful, because of which they are traumatizing for patients, especially for young children [4]. Although applying local hyperthermia (44 °C/30 min) has been successfully used for treating common and facial warts, side effects include burning sensations, blister formation, and subsequent hyperpigmentation [10]. No such side effects have been reported using a wIRA radiator (type 501; Hydrosun®, Müllhein, Germany) [4], most probably because IR-A components, which would typically cause unwanted thermal stress and a stinging and burning sensation in the skin by interactions with water molecules, are reduced by a water filter [11]. A combination of wIRA and 5-ALA based PDT has been used for treating actinic keratosis and basal cell carcinoma [5] and some patients with HPV-induced palmar and plantar warts [4]. PDT involves the excitation of a photosensitizer with VIS of 380–780 nm and the subsequent interaction of this with cellular lipids and proteins, either without oxygen (photooxidative reaction type I) or with oxygen (photooxidative reaction type II) [12]. 5-ALA is endogenously transformed into the photosensitizer, protoporphyrin IX by proliferating cells in the skin [6, 12]. The study by Fuchs et al. [4] showed that wIRA irradiation, either with or without 5-ALA-based PDT, significantly reduced recalcitrant foot and hand warts. Furthermore, wIRA distinctly increased the percentage of cleared warts compared to patients receiving the standard treatment scheme (including keratolysis and curettage as pre-treatment and retinoic acid ointment as post-treatment) alone, as well as completely curing some patients. Importantly, no scars or skin side effects were observed, and patients reported no disturbance of function after treatment [4]. Both, thermal and non-thermal effects may explain the wIRA effect. The increase in tissue temperature directly inactivates the thermolabile human papillomaviruses. Indeed, temperature rises above 42 °C have been shown to induce changes in the apolipoprotein B mRNA-editing catalytic polypeptide (APOBEC) 3 proteins, which are potent viral DNA mutators and feature broad antiviral activity [13]. wIRA hyperthermia might also indirectly activate tissue metabolism and may have immunomodulatory effects such as improving the local immune competence of the patient. Non-thermal effects of infrared radiation such as direct stimulation of cells [14], induction of cell growth towards infrared sources [15], and influences on cellular components, such as cytochrome c [16], have also been reported.
2 In Vivo and In Vitro Antibacterial Effects of wIRA
The emergence of antibiotic-resistant gram-positive and gram-negative bacteria is considered a global health problem due to the diminishing availability of antibiotics to treat these infections. Nonchemical treatments for infectious diseases using strategies such as local wIRA hyperthermia are being explored [17], as various bacterial species display thermo-sensitivity [18]. The effectiveness of wIRA treatment on infections with Chlamydia pecorum and Chlamydia trachomatis has been demonstrated in vitro using animal and human cell culture models [17]. Heat treatment has further been proven to be beneficial for Leishmania-induced skin lesions and Mycobacterium ulcerans (reviewed in [17]). wIRA irradiation in antimicrobial photodynamic therapy (aPDT) combined with toluidine blue as photosensitizer has been reported to be successful against the oral bacteria associated with the development of periodontitis, Streptococcus mutans, and Enterococcus faecalis [19]. Another wIRA study investigating the effect of PDT using the photosensitizer chlorine e6 on periodontal pathogens and subgingival biofilms in situ has demonstrated a distinct reduction of bacteria and oral biofilms [20]. Furthermore, wIRA irradiation alone has been shown to have beneficial effects on wound infections after abdominal surgery [21].
3 Treatment of Wounds and Wound Infections with wIRA
Several physical procedures are currently promoted as an “enhancer” of the treatment of wound infections, including cold atmospheric plasma, electrostimulation, laser therapy and extracorporeal shock wave therapy, and wIRA irradiation [22]. It is important that a distinction is made as to whether the antimicrobial effect is through killing bacteria and/or achieved by promotion of wound healing. Elimination of bacteria in the infected wound can support favorable outcomes, as is seen with a classic antibiosis [22]. A possible, endogenous PDT-like effect has been discussed for wIRA, since VIS and wIRA irradiation could interact with endogenous protoporphyrin IX or protoporphyrin IX of bacteria, and therefore could additionally support wound healing by evoking antibacterial effects [1]. However, direct antimicrobial effects by wIRA on non-thermosensitive bacteria have not yet been reported [23]. Hence, it is more likely that wIRA exerts its beneficial effects in wound infections by promoting the factors that are decisive for healing (e.g., tissue perfusion) and combating germs (e.g., increase in phagocytosis) in the wound environment [22]. Indeed, it has been reported that wIRA irradiation leads to an increase in local temperature [21, 24], in tissue blood flow [24] and in oxygen partial pressure [21]. These effects substantially support the healing process, especially in chronic wounds which are typically ischemic, hypoxic, and hypothermic [25]. wIRA also has non-thermal effects which are based on direct stimulation of cells and cellular structures by IR-irradiation. These effects comprise stimulation of wound repair [26], cell protection events [27], target-oriented growth of neurons [15], and possible effects on pain receptors [21]. Consequently, inflammation, pain, and the required dose of pain medication are reduced [2]. Overall, wIRA irradiation has a positive impact on wound healing, shortens the time to complete wound closure, and thereby can curtail hospitalization [23].
4 Investigation of wIRA Effects Using In Vitro Models
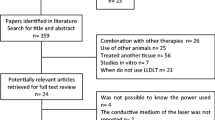
Wound healing is a complex process which involves different epidermal and dermal cell types, as well as leukocytes, all of which are coordinated by cytokines and growth factors. The primary focus is on fibroblasts, as they are involved in the production of extracellular matrix, and thus rebuild new tissue in the wound area [26], and keratinocytes which participate in the inflammatory reaction and ultimately close the injured area by epithelization [28]. Given the positive effects on wound healing by VIS-therapy (visible light-therapy), it is of interest to investigate the effects of VIS-therapy on cell viability and cell proliferation during wound healing, and also on cell migration. Zöller et al. [29] have treated foreskin and keloid fibroblasts with convective heat and/or wIRA to assess the potential of these as treatments for keloids and hypertrophic scars. They found a temperature-dependent induction of a spherical cell shape, a reduction of collagen type-I synthesis, and decreased TGF-β1 secretion in the fibroblasts. Although wIRA irradiation had no influence on MMP-1, it restored original cell morphology in foreskin fibroblasts and collagen type-I synthesis, and TGF-β1 secretion in keloid fibroblasts [29]. Knels et al. [30] evaluated wIRA for the treatment of oxidative stress in cells which is found in elderly or diabetic patients. For this, they exposed fibroblast cultures to glyoxal to induce glycation of proteins and lipids to mimic oxidative stress and determined their rescue from apoptotic cell death by wIRA. They found that wIRA irradiation diminished the effects of glyoxal-induced stress, such as ROS-production, translocation of phosphatidylserine, and DNA-fragmentation, which are considered main events of cell apoptosis, while being well tolerated by the cultured fibroblasts [30]. Wound healing is mostly investigated in vitro based on the direct measurement of cell migration and regeneration of the cell layer after mechanical damage to confluent cell layers (scratch wound assay) [31] (Fig.17.1). Cells that have been successfully used in this assay include HaCaT keratinocyte cells, primary epidermal keratinocytes, and primary dermal fibroblasts. Preliminary studies into wIRA effects on wound closure in vitro have shown distinct differences in responses of a wounded HaCaT keratinocyte monolayer after a 10-min treatment compared to the untreated control and heat treatment alone (Fig. 17.1). Cell migration started earlier in wIRA-irradiated cells (Fig. 17.1, middle column) in contrast to untreated cells (Fig. 17.1, left column), whereas heating cells for 10 min in order to induce the same temperature rise in the cells as induced by the wIRA irradiation delayed the healing process (Fig. 17.1, right column). Although, cellular processes induced and mediators involved remain to be elucidated, it is apparent that the observed clinical benefits of wIRA on wound healing can be investigated in vitro using adequate models and experimental settings, thereby allowing further clarification of the underlying biological effects. Several researchers have stressed that temperature changes need to be strictly controlled in vitro in order to distinguish between thermal and non-thermal effects of wIRA [32, 33]. In contrast to skin models or patient’s skin in vivo, in cell culture models there is only one cell monolayer and the protective epidermis or temperature control by blood circulation is missing [31, 32]. To evaluate exclusively non-thermal effects of wIRA irradiation, it is necessary to keep the temperature constant during the experiment [32, 33]. Accordingly, Jung et al. [34] tested the effects of wIRA on the generation of reactive oxygen species (ROS) in human dermal fibroblasts. They showed that ROS formation is heat-dependent and not induced by the irradiation alone as long as the temperature was kept constant. Temperature measurements were performed directly on the cell layers with thin thermocouples (type K, TC Direct, Mönchengladbach, Germany) to establish an in vivo like experimental set-up. For the wIRA treatment in the wound healing assays, cell dishes were exposed to different experimental conditions (Fig. 17.2a–c). The results were compared to the temperature curve during a local wIRA irradiation for 10 min on the forearm of a volunteer (Fig. 17.2d). A temperature rise from 34 °C to 42 °C at a skin depth of 1 mm was observed. The cells on the heating plate experienced a drastic increase in temperature since the surface of the plate is additionally heated by wIRA irradiation. In contrast, the temperature in the water bath with constant water exchange could be effectively controlled during the wIRA irradiation [33]. The increase in temperature when using a water bath without water exchange was comparable to the locally treated forearm of the volunteer, thereby confirming in vitro experiments on wound healing effects under in vivo-like conditions. However, in this experimental set-up, it is imperative to include control experiments which simulate increases in temperature to distinguish between effects caused by the wIRA treatment and pure warming of the sample, as they might occur during a clinical application of infrared A irradiation. In this way, it is possible to analyze more complex systems such as tissue models consisting of different layers of different cell types. In these samples, warming due to wIRA absorption cannot be avoided or reliably excluded by cooling [32]. Such an experimental regime is a pre-requisite for morphological investigations in 3D cell cultures to ensure close simulation of the in vivo conditions. It is known that cell behavior in 2D systems is different from that in their natural 3D environment in vivo. For instance, fibroblasts very quickly reach confluence in monolayers due to the high proliferation rate, and they show a biosynthetic capacity that does not correspond to the situation in vivo. In 3D collagen gels, fibroblasts show a lower biosynthetic activity and have a regulated growth and degree of differentiation that imitates the in vivo situation. Thus, 3D cell cultures represent an intermediate between 2D monolayer cultures and pre-clinical animal models and are already a viable alternative to animal experiments in some areas of application. Full (3D) skin models are used to test the cytotoxic effects of substances or treatments, as well as their influence on the cellular behavior. Reconstructed human epidermis (RHE) models are often utilized for this purpose and misleadingly referred to as skin models. Although these RHE models show a 3D structure of the epidermis of keratinocytes, they lack a dermal component, and therefore a corresponding interaction with local fibroblasts. 3D skin models consisting of a collagen matrix populated with primary human fibroblasts as the dermis and a completely differentiated epidermis made of primary human keratinocytes are also referred to as “full skin models.” Preliminary experiments have shown that wIRA treatment has no negative effects on the morphology in a 3D skin model (Fig. 17.3). In the epidermis, the undifferentiated basal keratinocytes express the keratins 5 (ck5) and 14 (ck14), whereas the cells in the upper epidermis switch to the expression of the keratin pair 1/10 (ck10) specific for differentiation [35]. Keratins are the main structural proteins in epithelial cells, in which they form a cytoplasmic network of 10–12 nm thick intermediate filaments [36]. Markers for the terminal differentiation of the keratinocytes to corneocytes (horn cells) of the stratum corneum are involucrin (IVL), a soluble precursor protein of the horny cell layer, and filaggrin (FLG), the aggregation protein of the keratin filaments in the horny cell layer [37, 38]. Changes in the composition and expression of such structural proteins have been associated with various skin diseases. Fibroblasts in the dermis can be detected by staining the cytoskeletal protein vimentin (VIM), a type-III intermediate filament protein. The detection of proliferating cells is possible using the marker Ki67 [39].
Regeneration of the cell layer in the scratch wound assay with human HaCaT keratinocytes (1) untreated, (2) irradiated with wIRA for 10 min and (3) exposed to comparable temperatures heating (without wIRA irradiation). Images were obtained using the JuLI™ Br Live Cell Analyzer (Peqlab, Erlangen, Germany)
Experimental set-ups for wIRA application on cell layers in vitro: (a) with the cell dishes either placed on a heating plate, (b) in water bath I with a slow water exchange, and (c) in water bath II without water exchange. Results were compared to the local wIRA irradiation for 10 min on the forearm of a volunteer (d). Temperature measurements were performed directly above the cell layers with thin thermocouples (type K, TC Direct, Mönchengladbach, Germany)
References
von Felbert V, Schumann H, Mercer JB, et al. Therapy of chronic wounds with water-filtered infrared-A (wIRA). GMS Krankenhhyg Interdiszip. 2008;2(2):Doc52.
Hartel M, Illing P, Mercer JB, et al. Therapy of acute wounds with water-filtered infrared-A (wIRA). GMS Krankenhhyg Interdiszip. 2007;2(2):Doc53.
Hoffmann G. Klinische Anwendungen von wassergefiltertem Infrarot A (wIRA) – eine Übersicht. Phys Med Rehab Kuror. 2017;27:265–74.
Fuchs SM, Fluhr JW, Bankova L, et al. Photodynamic therapy (PDT) and waterfiltered infrared a (wIRA) in patients with recalcitrant common hand and foot warts. Ger Med Sci. 2004;2:Doc08.
Foss P. Einsatz eines patentierten, wassergefilterten Infrarot-A Strahlers (Hydrosun) zur photodynamischen Therapie aktinischer Dyskeratosen der Gesichts- und Kopfhaut. Z naturheilkundl Onkologie krit Komplementärmed. 2003;6(11):26–8.
Fabbrocini G, Di Costanzo MP, Riccardo AM, et al. Photodynamic therapy with topical delta-aminolaevulinic acid for the treatment of plantar warts. J Photochem Photobiol B. 2001;61(1–2):30–4.
Stender IM, Na R, Fogh H, et al. Photodynamic therapy with 5-aminolaevulinic acid or placebo for recalcitrant foot and hand warts: randomised double-blind trial. Lancet. 2000;355(9208):963–6.
Piguet V. Heat-induced editing of HPV genes to clear mucocutaneous warts? J Invest Dermatol. 2017;137(4):796–7.
Kyriakis K, Pagana G, Michailides C, et al. Lifetime prevalence fluctuations of common and plane viral warts. J Eur Acad Dermatol Venereol. 2007;21(2):260–2.
Hu L, Qi R, Hong Y, et al. One stone, two birds: managing multiple common warts on hands and face by local hyperthermia. Dermatol Ther. 2015;28(1):32–5.
Winkel R, Hoffmann G, Hoffmann R. Wassergefiltertes Infrarot A (wIRA) hilft Wunden heilen. Chirurg. 2014;85(11):980–92.
Wolf P. Photodynamic therapy in dermatology: state of the art. J Eur Acad Dermatol Venereol. 2001;15(6):508–9.
Yang Y, Wang H, Zhang X, et al. Heat increases the editing efficiency of human papillomavirus E2 gene by inducing upregulation of APOBEC3A and 3G. J Invest Dermatol. 2017;137(4):810–8.
Albrecht-Buehler G. Surface extensions of 3T3 cells towards distant infrared light sources. J Cell Biol. 1991;114(3):493–502.
Ehrlicher A, Betz T, Stuhrmann B, et al. Guiding neuronal growth with light. Proc Natl Acad Sci USA. 2002;99(25):16024–8.
Karu T. Primary and secondary mechanisms of action of visible to near-IR radiation on cells. J Photochem Photobiol B. 1999;49(1):1–17.
Borel N, Sauer-Durand AM, Hartel M, et al. wIRA: hyperthermia as a treatment option for intracellular bacteria, with special focus on Chlamydiae and mycobacteria. Int J Hyperthermia. 2020;37(1):373–83.
Gazel D, Yılmaz M. Are infectious diseases and microbiology new fields for thermal therapy research? Int J Hyperthermia. 2018;34(7):918–24.
Al-Ahmad A, Tennert C, Karygianni L, et al. Antimicrobial photodynamic therapy using visible light plus water-filtered infrared-A (wIRA). J Med Microbiol. 2013;62(Pt 3):467–73.
Al-Ahmad A, Walankiewicz A, Hellwig E, et al. Photoinactivation using visible light plus water-iltered infrared-A (Vis+wIRA) and chlorine e6 (Ce6) eradicates planktonic periodontal pathogens and subgingival biofilms. Front Microbiol. 2016;7:1900.
Hartel M, Hoffmann G, Wente MN, et al. Randomized clinical trial of the influence of local water-filtered infrared A irradiation on wound healing after abdominal surgery. Br J Surg. 2006;93(8):952–60.
Daeschlein G, Lutze S, Arnold A, et al. Stellenwert moderner physikalischer Behandlungsverfahren bei infizierten und kolonisierten Wunden in der Dermatologie. Hautarzt. 2014;65(11):949–59.
Daeschlein G, Alborova J, Patzelt A, et al. Kinetics of physiological skin flora in a suction blister wound model on healthy subjects after treatment with water-filtered infrared-A radiation. Skin Pharmacol Physiol. 2012;25(2):73–7.
Mercer JB, Nielsen SP, Hoffmann G. Improvement of wound healing by water-filtered infrared-A (wIRA) in patients with chronic venous stasis ulcers of the lower legs including evaluation using infrared thermography. Ger. Med Sci. 2008;6:Doc11.
Schreml S, Szeimies RM, Prantl L, et al. Oxygen in acute and chronic wound healing. Br J Dermatol. 2010;163(2):257–68.
Danno K, Mori N, Toda K, et al. Near-infrared irradiation stimulates cutaneous wound repair: laboratory experiments on possible mechanisms. Photodermatol Photoimmunol Photomed. 2001;17(6):261–5.
Applegate LA, Scaletta C, Panizzon R, et al. Induction of the putative protective protein ferritin by infrared radiation: implications in skin repair. Int J Mol Med. 2000;5(3):247–51.
Suter MM, Schulze K, Bergman W, et al. The keratinocyte in epidermal renewal and defence. Vet Dermatol. 2009;20(5–6):515–32.
Zöller N, König A, Butting M, et al. Water-filtered near-infrared influences collagen synthesis of keloid-fibroblasts in contrast to normal foreskin fibroblasts. J Photochem Photobiol B. 2016;163:194–202.
Knels L, Valtink M, Piazena H, et al. Effects of narrow-band IR-A and of water-filtered infrared A on fibroblasts. Photochem Photobiol. 2016;92(3):475–87.
Büth H, Buttigieg PL, Ostafe R, et al. Cathepsin B is essential for regeneration of scratch-wounded normal human epidermal keratinocytes. Eur J Cell Biol. 2007;86(11–12):747–61.
Jung T, Grune T. Experimental basis for discriminating between thermal and athermal effects of water-filtered infrared A irradiation. Ann N Y Acad Sci. 2012;1259:33–8.
Jung T, Höhn A, Lau AM, et al. An experimental setup for the measurement of nonthermal effects during water-filtered infrared A-irradiation of mammalian cell cultures. Photochem Photobiol. 2012;88(2):371–80.
Jung T, Höhn A, Piazena H, et al. Effects of water-filtered infrared A irradiation on human fibroblasts. Free Radic Biol Med. 2010;48(1):153–60.
Uitto J, Richard G, McGrath JA. Diseases of epidermal keratins and their linker proteins. Exp Cell Res. 2007;313:1995–2009.
Gu LH, Coulombe PA. Keratin function in skin epithelia: a broadening palette with surprising shades. Curr Opin Cell Biol. 2007;19:13–23.
Kezic S, Jakasa I. Filaggrin and skin barrier function. Curr Probl Dermatol. 2016;49:1–7.
Proksch E, Brandner JM, Jensen JM. The skin: an indispensable barrier. Exp Dermatol. 2008;17:1063–72.
Bacchi CE, Gown AM. Detection of cell proliferation in tissue sections. Braz J Med Biol Res. 1993;26:677–87.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2022 The Author(s)
About this chapter
Cite this chapter
Wiegand, C., Tittelbach, J., Hipler, U.C., Elsner, P. (2022). Water-Filtered Infrared A Irradiation: From Observations in Clinical Studies to Complex In Vitro Models. In: Vaupel, P. (eds) Water-filtered Infrared A (wIRA) Irradiation. Springer, Cham. https://doi.org/10.1007/978-3-030-92880-3_17
Download citation
DOI: https://doi.org/10.1007/978-3-030-92880-3_17
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-92879-7
Online ISBN: 978-3-030-92880-3
eBook Packages: MedicineMedicine (R0)