Abstract
An exponential increase in products containing titanium dioxide nanomaterials (TiO2), in agriculture, food and feed industry, lead to increased oral exposure to these nanomaterials (NMs). Thus, the gastrointestinal tract (GIT) emerges as a possible route of exposure that may drive systemic exposure, if the intestinal barrier is surpassed. NMs have been suggested to produce adverse outcomes, such as genotoxic effects, that are associated with increased risk of cancer, leading to a concern for public health. However, to date, the differences in the physicochemical characteristics of the NMs studied and other variables in the test systems have generated contradictory results in the literature. Processes like human digestion may change the NMs characteristics, inducing unexpected toxic effects in the intestine. Using TiO2 as case-study, this chapter provides a review of the works addressing the interactions of NMs with biological systems in the context of intestinal tract and digestion processes, at cellular and molecular level. The knowledge gaps identified suggest that the incorporation of a simulated digestion process for in vitro studies has the potential to improve the model for elucidating key events elicited by these NMs, advancing the nanosafety studies towards the development of an adverse outcome pathway for intestinal effects.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
1 Nanomaterials in Food and Feed
Nanomaterials (NMs) and nanoparticles (NPs) show specific physicochemical properties (e.g., dimension, surface area area and functionalization) that provide advantageous mechanical, optical and electrical characteristics [1]. Nanotechnology is one of the recognized key enabling technologies due to its potential to improve the quality and performance of many types of products and processes, thus being widely applied in several industries, namely in the food industry, including food processing and packaging, and animal feed [2, 3] (Fig. 10.1). However, the exponential development of NMs contrasts with lacking conclusive risk assessment regarding the human health and the environment, causing concerns for public health [1].
In the food sector, NMs can be used as food additive to enhance product characteristics (e.g., texture, flavour and colour), improve the food stability during processing and storage or increasing nutritional value of food products [3, 4]. Several food additives have been recently identified to be NMs or as having a substantial fraction of the constituting particles in the nano range, with TiO2 being one of the most applied in food products [3]. TiO2 is used as food additive to augment the white colour of some products, such as dairy products, pastries, candies, sweets and chewing gums. In addition to being used as pigment, TiO2 can also be used to improve the flavor of non-white foods like vegetables, nuts, soups, sauces (e.g., mustard) and to clear beverages (beer, cider and wine) [5, 6]. Another important NM applied in food as an additive is silicon dioxide (SiO2, E551). This NM is used to clear beer and wines (prevent the turbidity of beverages) and as an anticaking and anticlumping agent [7].
Both NMs (TiO2 and SiO2), as well as nanosized magnesium oxide (MgO, E530) can be used in edible coatings to provide moisture or oxygen barrier and/or enhance sensory perceptions (e.g., flavor), thereby improving the product shelf life [4].
Furthermore, some NMs can improve the nutritional value of food, including animal feed products, via nanoencapsulation and nanoemulsions of supplements. Encapsulation of a compound (e.g., vitamins and flavonoids) in a nano sized vehicle confers protection against degradation and improves stability and solubility, thus leading to an increased bioavailability and a more efficient delivery to cells and tissues [3, 8]). As a component of numerous enzymes and hormones, zinc is essential for vital physiological functions in humans and, therefore, is common to add zinc oxide (ZnO) NMs as a source of in food supplements [9]. In the animal feed sector, the size reduction of selenium to nano range can increase the nutrient absorption in sheep, improving feed digestion [10]. Also, it is claimed that the addition of silver NPs (AgNPs) to drinking water can replace the use of antibiotics in chickens and pigs, improve digestion of feed and reduce the aflatoxin toxicity, which is very important since mycotoxins represent a worldwide problem for farmers [11,12,13]. In fact, Ag NPs are widely used for the disinfection of water, as well as TiO2 to decompose organic and inorganic contaminants in water [14].
NMs may also be applied in food contact materials (FCM), i.e., materials that directly contact with food products during manufacturing, transportation and storage [2]. Some examples are food packaging, cooking materials equipment, storing boxes, crockery and coatings of machines and surfaces [3]. Conversely, the application of NMs in FCM appears to have a promising future, since their incorporation can prevent microbial growth, reduce weight, increase heat resistance, increase mechanical strength and improve barrier against gases, UV radiation and moisture of the packaging. All of these features contribute positively to maintain the quality and safety of the food, increasing its shelf life [15].
Due to their antimicrobial properties against a broad range of microorganisms (e.g., viruses, bacteria, fungi), AgNPs are the most common NMs added to food packaging [3, 16]. In Europe (EU), these particles are not approved for use in plastic materials, since they can migrate to the food [17]. Chitosan, zinc oxide (ZnO), magnesium oxide (MgO) are candidates also to be used in FCM to prevent the appearance of pathogens in food [18, 19], however they are not allowed yet in EU. The incorporation of NMs, such as nanocellulose in FCM might improve the mechanical and thermal properties of the materials, namely the ones consisting in biodegradable polymers, since due to their natural origin these polymers tend to present poor barriers [20]. A summary of present, as well as future, applications of nanomaterials in food production, that may cause either direct or indirect consumer exposure, can be found in [21].
More recently, the utilization of (nano)biosensors in FCM has become a popular trend that is commonly known as “active packaging” and/or “smart packaging” [2]. The incorporation of nanobiosensors allows the detection of pesticides, pathogens, toxins and the monitoring of pH, oxygen (O2) and temperature, thereby delivering information of food quality in real time [2, 22,23,24]. Recently, Sahoo et al. [22] work reported that ZnO quantum dots (QDs) could detect several pesticides due to their high affinity for the Cl groups present in the pesticides. At the same time, ZnO QDs could photocatalyze the pesticides during the interaction [22]. Through color change, nanobiosensors based on TiO2 or nanocrystalline tin(IV) oxide (SnO2) can indicate O2, gases and pH changes or even the metabolites formation upon microbiological growth [3].
Currently, many of these applications in food and feed are already being commercialized and other are in development expecting to reach the market in a near future (summarized in Fig. 10.2). In this context, the human exposure to NMs may occur directly via ingestion of products containing NMs [21]. Conversely, it can occur indirectly, after the ingestion of foods contaminated with NMs that had been released from food-contact materials (FCM), or used as feed additives or nanopesticides. These different cases are addressed in the EFSA guideline for nanospecific risk assessment [25]. Although nanotechnology offers a broad range of promising and innovative applications, it also presents new risks. Therefore, it is becoming increasingly important to assess the potential risks of NMs in human health.
2 Human Exposure to Titanium Dioxide Nanomaterials (TiO2) in Food and Food Chain
Since TiO2 can improve the color, texture, flavor and stability of many food products, nutritional supplements and pharmaceutical formulations, it is one of the most used NMs in the food sector. E171, the European designation for food-grade TiO2, is a food additive and colorant approved by the European Union in 1969 [26, 27], in which, “approximately, 30% of its particles are less than 100 nm in diameter”[28]. The size range where most particle lie is ca. 40–250 nm [29]. The percentage by number of constituent particles smaller than 30 nm has been determined to be ≤1% in samples of E171, either pristine or extracted from foods [28]. It might be applied as a pigment/food colorant to whiten and improve the opacity of skim milk, ice creams, coffee creams, sauces, pastries and candies, while also being capable of enhancing the flavor of processed food items and to clear distinct beverages [5, 6, 30, 31]. TiO2 can also be utilized as an anticaking agent in granular and powdered foods [5, 32]. Sweets and candies (e.g. chewing gum, chocolate and products with white icing) contain the largest content of TiO2 in their composition amongst the available food products: 0.01–1 mg per serving [5]. This led to the estimation of consumption of 0.2–1 mg/kg/day of TiO2 by the average adult [5]. Some of the lesser relevant examples of its oral intake are mainly associated with the accidental ingestion of toothpaste and lipstick [6, 33]. In this sense, others estimate that most humans follow a West European diet and used toothpaste, that may imply an oral intake of 0.06–5.5 mg TiO2/kg body weight/day [33,34,35]. In a very recent report, EFSA Panel estimated, for several population groups (infants, toddlers, children, adolescents, adults and the elderly), the chronic dietary exposure to E171. It was concluded that in the scenario assessment of maximum level exposure, the mean exposure to E171 varied from 0.06 mg/kg bw/day in infants to 12.8 mg/kg bw/day in toddlers [28].
Nanosized TiO2 also exhibits increased UV-blocking properties, in a different form associated to a transparent appearance, with particles entirely <100 nm, and this form is used in UV filters, which are advantageous for its incorporation in food packaging and storage [32]. Due to the emerging number of applications of TiO2 in the food sector, there is a higher potential of oral intake of food products. In addition, the use of TiO2 in pharmaceutical sector, or cosmetics such as toothpaste and lipstick, can also result in the ingestion of nanosized TiO2, although these are outside the regulation of the food sector.
As a matter of fact, in a study using human volunteers with a normal intestinal permeability, it was shown that a fraction of pharmaceutical or food-grade TiO2 can be directly absorbed into the bloodstream in its particulate form, after its oral administration (100 mg, in this case) [36]. The same authors also suggested that there are, probably, two distinct particle uptake pathways in the human gut, one in the proximal small intestine and another in the distal small intestine [36]. To quantify the human exposure and uptake of TiO2 and to unravel the responsible mechanisms, further quantitative measurements were suggested to be needed [36]. Also, Böckmann et al. [37] reported the absorption of capsules or anatase powder containing TiO2 from the gastrointestinal tract (GIT) into the bloodstream, following oral administration. More recently, it was reported the accumulation of both titanium (Ti) and TiO2 in the human liver and spleen analyzed post-mortem, in which more than 24% of the particles were at the nanoscale (< 100 nm) [38]. This means that the daily oral exposure to TiO2 particles found in consumer and food products can lead to bioaccumulation upon human oral intake [38].
As a consequence, the oral ingestion/intake of TiO2 might constitute an emerging risk for human health, which implies a need to perform the safety assessment of these NMs in order to understand the biological effects and toxicity regarding their consumption. Despite TiO2 is one of the most commonly applied NMs in food sector, the majority of the (nano)toxicological studies focus on non-oral routes of exposure (i.e. inhalation and dermal contact). The available data regarding toxicokinetics upon oral exposure is still very limited and, therefore, it’s crucial to study the possible toxic effects of these NMs [30, 31, 39, 40]. A key study demonstrated the absorption and deposition of E171 in rodents upon repeated oral exposure, where the accumulation of E171 in the liver and intestine of mice was observed, at a dose comparable to human exposure levels [41]. The inflammation in the intestine and stomach of the exposed mice, as well as increased superoxide production upon E171 treatment, highlighted the need for considering human health risks as a result of dietary exposure to the food-grade TiO2 [41].
3 Safety Assessment of Ingested TiO2 – The View from a Regulatory Perspective
TiO2 have been classified as possibly carcinogenic to humans (IARC, group 2B) [42], based on studies on animals exposed by inhalation, and also as a potential occupational carcinogen (NIOSH, 2011). As for cosmetics, the Scientific Commission for Consumer Health (SCCS) has declared that its use does not harbour increased health risks, as long as the TiO2 containing products are applied on intact skin [43]. In 2019, the European Parliament and the Council on cosmetic products published an amendment to the Regulation (EC) No 1223/2009 in accordance with the opinion of the Standing Committee on Cosmetic Products, warning that it must not to be used on the lips (Official Journal of the European Union, 2019).
Up to date, no consensus exist on the use of TiO2 as a food additive. The Food and Drug Administration (FDA) categorizes TiO2 as “Generally Recognized as Safe” (GRAS) and allows products not to exceed more than 1% TiO2 in weight (https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfCFR/CFRSearch.cfm?fr=73.575, accessed 24/09/2020). In spite the European Union (EU) had approved the use of food-grade TiO2 or E171 as a Group II food color at quantum satis, that is, it can be applied to products “at a level not higher than is necessary to achieve the intended purpose”. (European Commission, 2008), very recently this risk assessment has been revisited by EFSA. As of 6th May 2021, EFSA updated its safety assessment concerning E171, concluding that it can no longer be considered as safe when used as a food additive [28]. This is line with decisions from other regulatory bodies such as the French Agency for Food, Environmental and Occupational Health and Safety (ANSES), that imposed in France the ban of its use in food, since January 2020 [44], highlighting the need of further studies to characterize the potential health effects related to ingestion of E171. The latest EFSA report, describes the re-assessment of the toxicological data according to the requirements specified in the 2018 EFSA Guidance on nanotechnology [28]. The Panel concluded that the available data did not suggest adverse effects with either E171 up to a dose of 1000 mg/kg bw per day or with TiO2 (<30 nm) up to 100 mg/kg bw per day. Furthermore, it was considered that studies found in the literature on reproductive and developmental toxicity of E171 or neurotoxicity were not reliable and that the studies on immunotoxicity and inflammation were inconsistent. A new reproduction toxicity one-generation study was performed and did not reveal general toxicity, nor effect on thyroid or sex hormone levels, reproductive function and fertility nor pre- and postnatal development. A slight effect was observed in immunotoxicity, with no dose-response, while the effect of E171 in producing aberrant crypt foci described in Bettini et al. [45] was not replicated in other studies. Noteworthy, the Panel concluded that “TiO2 particles have the potential to induce DNA strand breaks and chromosomal damage, but not gene mutations, and a concern for genotoxicity of TiO2 particles cannot be ruled out” [28]. The up to date evidence, along with all the uncertainties, further highlight the need for accurate risk assessment of TiO2 that can be ingested and affect human health.
4 Nano-Bio Interactions of Ingested Nanoparticles
The mechanisms of toxicity of NMs following oral exposure and ingestion have been poorly characterized, although changes in the secondary properties of NMs may occur in view of their dynamic behavior under physiological conditions, and a global network of cellular and molecular pathways are likely to be impacted upon such exposure. The reports concerning the toxicity of NMs are often contradictory as a result of poorly characterized formulations and exposure conditions. Our previous work has suggested that the primary physicochemical descriptors of NMs may not be the most adequate to foresee their toxicological behavior [46]. In fact, changes in cellular environment, such as the culture medium, may affect the outcome of toxicity assays [46, 47]. It was shown in vitro that the same TiO2 test material, prepared with standardized dispersion protocols, yields different outcomes in blood or respiratory cells, alongside with the use of distinct cell culture conditions, that have different effects in secondary characteristics of the NMs, leading to discrepant observations [46].
When ingested, the interaction between TiO2 and the organic biomolecules in food and in the gastrointestinal fluids is unavoidable. Under these circumstances, the physicochemical properties of the particles may change, as well as the experimental outcome [48]. NMs may agglomerate/aggregate, react or bind to other components of food/feed, solubilize upon reaction with digestion fluids, or can even be excreted from the body [49]. Due to the plethora of possible transformations, NMs may not be available in free particulate forms, and their translocation across the GIT may be influenced as well as their cytotoxic and genotoxic outcomes [50]. For example, very recently, Zhang et al. [49] reported that the potential toxicity of TiO2 can be reduced by the presence of a food matrix. Another study investigated the dissolution behavior of NMs under the influence of the GIT context, by using simple acidic and neutral solutions, showing that an important characteristic that influences TiO2 solubility is the crystal form [51]. In that work, all the TiO2 forms dissolved very slowly at both pHs, but a greater solubility was observed for nano-anatase compared to nano-rutile at neutral pH [51].
In vivo studies may provide more realistic approaches concerning the modifications that NMs may suffer in the digestion process. In spite some in vivo studies in rats addressed the biodistribution, elimination and toxicity of ingested NMs [52,53,54], the impact on the GIT should be re-considered in view of the major differences that exist between humans and rats, regarding the physiology and nutrient uptake of the GIT [55]. Considering these limitations, simulated digestion models that are available can provide an interesting tool for investigating the digestion of food contaminants [56] and eventually NMs [30], thus providing an in vitro improved alternative to animal models. One of such models has undergone international harmonization, particularly the standardized INFOGEST in vitro digestion method [57, 58]. This method simulates the physiological conditions, including the pH, time duration, enzymes activity, and composition of simulated digestive fluids of the upper GIT, including the several digestion stages: oral, gastric and small intestinal [57]. Briefly, the process involves three successive digestive phases: oral, gastric and intestinal. The oral phase includes exposure of the compound to simulated salivary fluid and amylase enzyme, followed by the addition of simulated gastric fluid and gastric enzymes (pepsin and gastric lipase). In the intestinal phase, simulated intestinal fluid, bile salts and pancreatin enzyme are added and, after incubation, an enzyme inhibitor, such as 4-(2-aminoethyl) benzenesulfonyl fluoride hydrochloride (Pefabloc) is used to stop enzymatic reactions). Our previous results using this model showed that one anatase/rutile TiO2 mixture submitted to simulated in vitro digestion (NM-105), toxicity occurred after exposure of HT29-MTX-E12 intestinal cells, and was more pronounced as compared to undigested NMs, together with with subtle decreases in the hydrodynamic size of the NM in cell moiety [59].
Other simulated digestion models have been described in the literature, but are not usually applied to NMs. The dissolution, biodurability and persistence of several NMs in individual simulated gastrointestinal fluids (saliva, gastric and intestinal) were recently studied in a physiologically relevant digestion cascade (including saliva -gastric - intestinal), and TiO2 was found to be the most biodurable and persistent NM [55]. The biopersistence and lack of dissolution during digestion is consistent with the TiO2 observed in the final product of digestion performed using standardized INFOGEST in vitro digestion method, detected in nano form and agglomerated nanoclusters [59]. In other work, a detailed characterization of size, size distribution, morphology and the pH and their changes with the digestive medium showed increasing agglomerate size over time and during the gastrointestinal tract cascade [55]. Using different TiO2, our recent work did not show major differences in agglomerates’ size for two TiO2 (NM-102, NM-103 provided by the Joint Research Centre, Ispra, Italy) in the end of the standardized INFOGEST in vitro digestion method, but found smaller agglomerate’s size for one TiO2 (NM-105) [59]. This finding may favor the view of an influence of the NM crystal phase and properties in their biopersistence, previously referred [50]. It is therefore foreseen that the addition to the test system of a diversity of individual factors/components during treatment, the exposure approach, and the selected cell model may lead to in vivo-like conditions, better representing intestine for nanosafety research [60].
5 Cellular Effects and Underlying Mechanisms of Action of TiO2 in the Intestine
Following ingestion, NMs may move through the upper GIT, reaching the colon. The potentially adverse effects of ingested TiO2 may therefore occur within the site of NMs absorption (intestine), as well as in other organs in the body after absorption like the liver and spleen, the sites of NM metabolism and detoxification [61]. Upon reaching the intestinal cells, TiO2 can exert a direct damage on the GIT structures. Recent in vitro and in vivo studies have shown that TiO2 can damage intestinal microvilli and tight junctions and interact with the epithelium of the small intestine, disturbing digestion/absorption of food, eventually leading to deficiencies of macro- and microelements in the organism [62,63,64,65]. The disruption of the brush border in human intestinal Caco-2 cells exposed to food grade TiO2 was already described in vitro [62]. In a model of Caco-2/HT29-MTX cells, TiO2 NMs decreased the number of microvilli, reducing the surface area available for absorption of nutrients, Fe and Zn, capture of fatty acids and inhibitor of apoptosis protein activity [63]. In the same cell model, in the presence of TiO2 there were alterations in glucose uptake/transport, caused by intestinal microvilli damage, [65]. As suggested by ICP-MS data, the TiO2 penetrated intestinal mucosa and, in male rats, one dose increased height and width of villi, while there was dose-related increase in density of goblet cells, not seen on female rats [66]. Brun et al. showed that the agglomerates of TiO2 crossed the regular epithelium of the ileum, altered its permeability and persisted in gut cells, where they could induce chronic damage [67]. A higher accumulation of TiO2 was seen in Goblet cells and M-cells, as compared to enterocytes, and tight junction remodelling was promoted through deregulation of genes encoding for proteins involved in epithelial structure maintenance [67]. In Caco-2 cells, Koeneman et al. showed that uncoated TiO2 can translocate through epithelial lining (at low levels) by transcytosis and lead to sub-lethal effects as microvilli reorganization and changes on the apical surface of the epithelium and calcium level, without disrupting junctional complexes [64]. Further recent evidence shows that the in vitro exposure of Caco-2 cells to TiO2, disturbed the tight junctions-permeability barrier with an effect detectable after 4 h of incubation and extensive effects on barrier integrity at 24 h, indicating that nano-sized TiO2 particles exert harmful effects on the intestinal epithelium layer [68]. On the contrary, an in vitro study using a co-culture of human enterocytes (Caco-2 cells) and M-cells, provided evidence for the lack of translocation of TiO2 across the gut epithelium model, and the results from the same authors after oral administration in rats did not suggest any significant internal exposure of the consumer to the NP by oral ingestion of nano- or larger particles of TiO2 via food [53]. In spite, the accumulation of both titanium (Ti) and TiO2 in the human liver and in the spleen analysed post-mortem that was reported recently suggests that the daily oral exposure to TiO2 can lead to bioaccumulation [38]. In fact, only recently, studies on uptake and translocation of ingested TiO2 across the GIT are starting to emerge. Following ingestion, uptake of NPs across the GIT can occur via different pathways. In the case of poorly soluble nano TiO2, active uptake by endocytosis-related pathways at the mucosal membrane are probably the most accepted uptake mechanisms [69]. Whether or not crystal structure and size influences the rate of uptake of Ti from TiO2 by gut cells, was investigated by Gitrowski et al. [69]. The authors found that cells accumulate Ti from TiO2 exposure possibly explained by an active uptake of Ti-containing particles in physiologically competent cells, suggesting the probable relevance of crystal structure-effect, being the anatase form of TiO2 absorbed faster than the rutile [69]. The TiO2 uptake in GIT, via the Peyers patches, was also proposed to take place, due to the elevated presence of TiO2 in the lymphoid tissues [67].
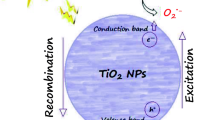
Information on cellular uptake of NMs gives a first indication on its possible mechanisms of action. For example, the interaction of NM directly with DNA can only occur if the NM is taken up by the cell and is able to enter the nucleus to reach the DNA [70]. Thus far, the mechanisms of NM tissue and/or cell damage is unclear, and the molecular changes involved in these processes are unclear [71], but it has been considered that ROS formation could contribute to the induction of cell damage [27]. An elevated level of reactive oxygen species (ROS) and expression of inflammatory transcripts with increasing NMs concentration, as well as the binding of TiO2 to the cellular membrane and its passage into the cells, has been reported. ROS formation have been implicated in both indirect primary genotoxicity and secondary genotoxicity mechanisms following exposure to NMs [72]. A comprehensive review of in vitro mammalian studies of effects of TiO2 by Iavicoli et al. [73] revealed that most papers report induction of ROS by TiO2, followed by different types of cellular effects [73]. In most of the studies, TiO2 induced ROS generation following exposure to TiO2. In undifferentiated Caco-2 cells, exposure to different types of TiO2 particles (anatase, 50 nm; rutile, 50 nm; anatase, 100 nm; rutile, 250 nm; and P25, 21 nm) at 25 and 50 μg/mL, significantly increased ROS levels in undifferentiated Caco-2 cells, following 3 h exposure, and an increase of IL-8 expression at the highest dose tested [74]. Exposure to different sizes of 80% anatase and 20% rutile TiO2 TNP 18 (5.84 ± 6.59 nm), TNP 30 (24.59 ± 8.60 nm) and TNP 87 (81.80 ± 5.27 nm) for 4 h was also showed to induced a 10–18 fold increase of ROS levels at higher doses (60 μg/mL and 100 μg/mL) compared to control for 48 h post exposure [75]. TiO2 A12 (95% anatase, 5% rutile; 12 nm) and R20 (90% rutile; 10% anatase;22 nm) were seen to accumulate in undifferentiated Caco-2 cell cultures exposed to 50 μg/mL, with no alterations in cell viability or DNA damage despite increased ROS generation, after 6 and 48 h [76]. A high-level increase of ROS in a dose-dependent manner was also seen after exposure to 1, 2.5, 5, 10, 20 μg/cm2 (corresponding to 6.4–128.0 μg/ml) of TiO2 (anatase <25 nm, 99.7% purity, BET surface area 45-55 m2/g), after 6 h, but not after 24 h, with no induction of cytotoxicity, or IL-8 release [77]. Later, the same group, found that exposure to 1 and 2.5 μg/cm2 (corresponding to 6.4 and 16.0 μg/ml) of the same NM significantly increased the basal level of DNA 8-oxodG in comparison to the control at 6 and 24 h of treatment, which was more evident at 6 h exposure [78]. Using a different model of non-mucus-producing phenotype of colorectal adenocarcinoma (HT-29) cells, an increase in ROS was observed after short exposures to 4.5, 9 and 36 μg/ml TiO2 (anatase, <25 nm, surface area 45-55 m2/g), for 6 and 24 h [66], more evident after 6 h exposure. In the human colon cancer cell line (HCT116) and normal colon cell line (NCM460), TiO2 (25 nm, anatase) promoted a dose-dependent increase of ROS production, after exposure to 15 μg/mL, 30 and 60 μg/mL for 24 h [71, 79]. The intracellular ROS formation was markedly elevated by TiO2 in a dose-dependent manner in Caco-2 and HepG2 cells treated with rutile 30 nm TiO2 (100–300 μg/mL) for 24 h [61]. Also, in HepG2 cells, ROS levels dramatically increased from 6th to 24th hours exposed to 10 μg/mL TiO2 [80, 81]. Positive findings on ROS generation have also been found in co-culture of Caco-2 and HT29-MTX cells. Guo et al. [63] assessed the formation of ROS, following 4 h and 5 days exposure to TiO2 (30 nm), showing an increase in ROS production. Following acute and chronic exposure to three different types of TiO2, particularly, E171 (> 95% anatase; 118 ± 53 nm), P25 (86% anatase/14% rutile; 24 ± 6 nm) and A12 (> 95% anatase; 12 ± 3 nm) induced ROS formation was observed after at all three timepoints (6 h, 24 h and 48 h), following acute exposure to 50 μg /mL P25 and E171 (the latter also induced ROS at 10 and 100 μg/mL concentrations), while A12 induced ROS after 6 and 24 h exposure, but not at 48 exposure [82]. Similarly, intracellular ROS levels were higher in repeatedly-exposed cells (along 21 days), following exposure to P25 (at 50 μg /mL) and E171 (at 50–100 μg/mL) when compared to untreated cells.. DNA strand breaks, alkali-labile sites and oxidative purine lesions were observed only when cells were exposed to the highest concentration, 50 μg/mL, of E171 using the comet assay and FPG-modified comet assay [82]. Later, the same group showed an induction of ROS generation after exposure for 6 h, 24 h or 48 h to 50 μg/mL to A12 (95% anatase, 5% rutile; 12 nm), NM-105 (86% anatase, 24 nm), or E171 (>95% anatase, 118 nm) or to 10, 50 and 100 μg/mL of E171, independently of exposure time or type of TiO2. Increased ROS level in cells exposed to E171, was concentration-dependent, with significantly higher ROS levels in cells exposed to 50 or 100 μg/mL of E171 [83]. After 24 h of exposure of NPs decrease in intracellular GSH levels of Caco-2 and HepG2 cells was observed at 100, 150, 200, and 300 μg/mL.
In vivo, after TiO2 treatment, the ROS levels of liver and kidney cells in ICR mice were significantly increased, in dose-dependent manners [80, 81]. After intragastric administration of TiO2 to mice during 30 days, an increase in the accumulation of ROS (e.g. OH−) was observed in the spleen of mice, involving p38-Nrf-2 signalling pathway, due to lipid peroxidation [84].
Negative results concerning oxidative stress were also reported in literature. In Caco-2 cells, TiO2 with a diameter ranging from 3.94–25.20 nm was induced cell mortality, but no oxidative stress or DNA damage [85]. Gerloff et al. [85] found that TiO2 containing anatase-rutile, in contrast to the pure anatase, induced cell death or mild DNA damage, suggesting that both surface area and crystallinity are critical determinants of TiO2 toxicity. Nevertheless, they did not find any signs of oxidative stress and ROS production, following exposure to 20 a 80 μg/cm2 for 24 h, suggesting that other mechanisms that require further studies might have led to the toxic responses reported [85]. Abbott Chalew and Schwab [86] also did not report increased ROS generation in undifferentiated Caco-2 and SW480 cells following 4 or 24 h exposure to 0, 0.1, 1, 10, or 100 μg/mL TiO2 Aeroxide P25 NM105 (80% rutile:20% anatase; 21 nm), as measured by DCFH-DA fluorescence assay [86]. In fact, they found an overall reduction of ROS, which was more prominent after 24 h exposure. ROS generation was also inhibited in medium comprising 0.05% BSA in two human colon cancer cells lines (Caco-2 and/or HCT116), as measured by electron spin resonance (ESR)/paramagnetic resonance spectroscopy, following 24 exposure to 0.143 and 1.43 μg/cm2 (which equivalents to 1 and 10 μg/mL, respectively) of E171, and TiO2 (10–30 nm), in Caco-2 cells, which was only increased following exposure to micro-sized TiO2 particles (average size 535 nm) [27]. The authors suggested a scavenging or inhibitory effect by the protein corona which may prevent ROS formation by inhibiting the contact between particle surface and ROS precursors. Also, no intracellular ROS generation was found in undifferentiated Caco-2 cells following exposure to 0.125–125 μg/ml E171, for 3 h [87]. In differentiated Caco-2 cells, no significant increase in ROS formation, cytotoxicity and DNA damage was observed following a 3 h or 24 h exposure to 0–256 μg/mL of TiO2 rutile hydrophobic form (JRC benchmark NM-103, 25 nm) and rutile hydrophilic (JRC benchmark NM-104, 25 nm), using the CellROX assay [88].
The use of digestion simulation fluids for TiO2 before undifferentiated Caco-2 cell cultures exposure, induced a slight decrease in cell viability and membrane integrity and an increase in ROS generation, following exposure to 100 μg/mL and 200 μg/mL of two anatases T1 (99 ± 30 nm) and T2 (26 ± 12 nm) for 24 h [89]. However, it had no effect on differentiated Caco-2 cells [89].
The inconsistency of the results observed in the literature may be due to the physicochemical properties of the NM itself, NM dispersion method, difference in NMs’ size and dispersion stability or to the specific protocol conditions, as previously described in a literature review [90], such as the time of exposure or the different cell models used.
The ability of NMs to affect the immune system has been discussed in several in vitro and in vivo studies. NMs were identified in recent reports as potential stimulants of immune responses that may lead to immunotoxicity, being this endpoint relevant for addressing nanosafety [91]. In vitro, Tada-Oikawa et al. [74] reported that the exposure to anatase (50 nm) TiO2 during 72 h, decreased the cell viability of Caco-2 cells in a dose-dependent way and also induced proinflammatory response, seen by increased levels of IL-1β and IL-8. In addition, TiO2 particles triggered an inflammatory response in co-culture of Caco-2/HT29-MTX cells, showing increased release of IL-1β, IL-8, IL-17A, eotaxin, and RANTES and moderate increase in the expression of some efflux pumps [83]. In other work, the exposure of cocultures to TiO2 caused increases in IL-8 release, but had no effect on IL-8 release in monocultures [63]. In vivo, Trouiller et al. [92] an elevated expression of inflammatory cytokines such as TNF-α, interferon-γ and IL-8 in the blood of mice was shown after oral intake of 100 mg/kg bw TiO2 for 5 days. In rats exposed for 7 and 100 days to ingestion of 10 mg/kg bw of E171, was observed a decreased frequency of immunoregulatory Tregs and CD4 + CD25+ Thelpers, as well as the induction of inflammatory markers such as TNF-α, IL-8 and IL-10, in aberrant crypts after 100 days of exposure [45]. A potent Th1/Th17 immune response was detected via an increased production of IFN-γ in Peyer’s Patches and IFN-γ and IL-17 in the spleen after 7 days of exposure [45]. More recently, increased concentration of IL-6 in the serum of rats treated with 50 mg/kgTiO2 for 30 days was observed [93]. Long-term oral exposure to TiO2 also impaired immune functions in rats [94]. Also, the molecular nature of TiO2-induced immunotoxicity in RAW 264.7 macrophage which shown to occur via induction of apoptosis and simultaneous multiple toll-like receptors signalling through ROS-dependent SAPK/JNK and p38 MAPK activation [95]. Using livers from mice exposed intragastrically to 10 mg/kg bw for 90 days, Cui et al. [96] observed the generation of inflammation and a reduction in immune capacity by the downregulation of genes involved in the complement system through whole genome microarray analysis. Liver Inflammation and fibrosis were described after long-term exposure to TiO2 in mice fed for 9 months [97]. In primary bone marrow derived macrophages, TiO2 activated the inflammasome in macrophages [98].
In a co-culture of Caco-2/HT29-MTX intestinal cells, although ROS production was detected, only minor changes were observed in mRNA expression of genes involved in ROS regulation, DNA repair via base-excision repair, and endoplasmic reticulum stress [83]. The consequences of epigenetic changes induced by exposure to NMs are still poorly understood [99]. It is recognized the potential of NMs to change global DNA methylation, as well as gene-specific methylation patterns, including tumour suppressor genes, inflammatory genes, DNA repair genes, and impaired expression of genes involved in DNA methylation reactions, are all potentially relevant to cancer development [100]. For example, in bronchial cells, hypomethylation was observed for anatase, rutile and anatase: rutile mixture forms of TiO2 [101], suggesting that epigenetic studies should be performed along with conventional toxicity testing methods.
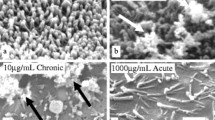
TiO2 appears to have impact on the microbiome, as seen as bacterial ratio of the human intestinal community in vitro which can affect the immune response [102]. In vitro bacterial growth inhibition and morphological and structural damage was observed following exposure to E171 [103]. However, these studies were conducted in vitro and therefore do not reflect the complexity of gut microbiome. Pinget et al. [104] investigated the impact of E171 on gut microbiota using male mice orally exposed via drinking water [104]. They observed that TiO2 had minimal impact on the composition of the microbiota in the small intestine and colon, but it changed the release of bacterial metabolites in vivo and affected the spatial distribution of commensal bacteria in vitro promoting biofilm formation. The same authors also reported, in mice exposed via intragastric to 150 mg/kg TiO2 (21 nm) for 30 days, reduced expression of a key component of the intestinal mucus layer, the colonic mucin-2 gene, and increased expression of the beta defensin gene, events associated with colonic inflammation [104, 105]. Furthermore, it was shown that, although unapparent pathological changes were observed in small intestine, gut microbiota was remarkably decreased, and gut microbial community compositions was significantly changed. Chen et al. [93] also found changes in the gut microbiota and faeces metabolomics, in Sprague-Dawley rats orally exposed to 0, 2, 10, 50 mg/kg TiO2 (29 nm, anatase), daily for 30 days [93]. Pathological inflammatory infiltration and mitochondrial abnormalities were observed also in rats after TiO2 [93].
Events such as immunotoxicity, inflammation and DNA damage are recognized in general to increase the risk of developing cancer. In distal colon of mice, after intragastric exposure to E171, Proquin et al. [106] observed induced oxidative stress and immune response pathways, activation of DNA repair genes and gene expression changes in genes related to cancer development, together with epithelium in colonic crypts, 14 and 21 days after E171 ingestion. The results are consistent with previous studies conducted by the same authors, with an identical colitis associated mouse model, in which hyperplastic alterations in the colon of mice were observed from 4 weeks of E171 ingestion accompanied by a decrease in the number of goblet cells in animals exposed by oral gavage to 5 mg/kg bw per day, 5 days a week, for 10 weeks, [107]. Besides, in an Adult male Wistar rat model exposed to 10 mg/kg bw/day for 7 days of E171, by intragastric gavage, led to the promotion of microinflammation, as well as initiation of preneoplastic lesions [45].
Overall, no clear picture has emerged yet between the key events (KE) and the adverse outcomes (AO) that have been reported upon GIT exposure to NMs, hindering the development of an adverse outcome pathway (AOP), as defined by OECD [108]. Results from multiple studies here presented, although often contradictory, suggest a potentially harmful effects of TiO2 in in vitro and in vivo intestinal tissue, liver and spleen after oral exposure, which is apparently related to generate ROS, induced oxidative stress and inflammation [109], but it is unknown whether these events subsequently result in irreversible adverse effects in humans [109]. Also, a great number of studies did not use food-grade NMs, such as E171, in their experiments, which might hinder conclusions on its relevance for human safety. It was suggested in a recent assessment of the current evidence that key cellular and molecular effects of TiO2 particles can occur in human liver, intestinal tissue, spleen and kidney after oral exposure, but it is unknown whether these events subsequently result in irreversible adverse outcomes (AO) in humans [109]. Further research is necessary to clarify whether TiO2 leads to AOs, and under which conditions this may occur, in order to guarantee the safe use of TiO2 as a food additive.
6 Ingested TiO2 Cytotoxic and Genotoxic Effects – Potential Implications in Cancer
Genotoxicity can be defined as the process in which a test agent is responsible for inducing damaging effects on DNA (single and double strand breaks, loss of excision repairs, cross-links, alkali labile sites), RNA or chromosomes (structural and numerical chromosomal aberrations), affecting the integrity or function of those structures [110, 111]. Furthermore, genotoxicity and carcinogenicity are correlated since many carcinogenic agents might act through genotoxic mechanisms [112, 113].
The genotoxic effects after the exposure to an agent, such as NMs, can be assessed by specific genotoxicity assays. According to the Food and Drug Administration (FDA), they can be defined as “in vitro and in vivo tests designed to detect compounds that induce genetic damage by various mechanisms” [114], that have the potential to replace long-term carcinogenicity studies. A positive result can indicate that a certain compound has the potential to be a human carcinogen [114]. For an adequate assessment of genotoxicity, the Organization for Economic Co-operation and Development (OECD) has defined Genetic Toxicology Test Guidelines (TGs) for the usage of these assays [115]. Methodologies such as the in vitro chromosome aberration, the in vitro or in vivo micronucleus test and the in vivo comet assay are included in those guidelines with specific orientations. Whenever possible, in vivo testing should be replaced by in vitro assays, in order to avoid using animal models [116]. It was necessary to adapt some of the previously described assays to NMs’ genotoxicity testing since some of their physicochemical properties interfere with the outcome [115, 117].
Since genotoxic effects can be often masked by cytotoxic effects, it is imperative to carry out a preliminary cytotoxicity assessment of a compound in order to find the proper range of concentrations to perform the following genotoxic assays. Cytotoxicity assays can detect the number of viable cells in a determined cell population and in this way, enable the assessment of the cytotoxic potential of a test agent. There are many assays to evaluate cytotoxicity, being one of the most important based on the mitochondrial activity and metabolic cell proliferation [118]. This includes the MTT (3-[4,5-dimethylthiazol-2-yl]-2,5 diphenyl tetrazolium bromide) assay, in which mitochondrial enzymes released only by living cells can convert tetrazolium salts (MTT) into insoluble formazan crystals. Accordingly, the amount of purple formazan crystals produced is dependent on the number of viable cells, which is reflected by an increase in the optical density (OD) [118, 119].
As previously described, nanosized TiO2 is one of the most used NMs with applications in consumer and industrial products and the trend for its use is increasing exponentially [120]. Bearing this in mind, the study of cytotoxicity and genotoxicity that may arise from the use of products containing these NMs has also triggered interest, namely in the food and feed sector. In this sense, the study of the adverse biological effects that may derive from the ingestion and subsequent digestion of TiO2 and its possible absorption into the GIT are of extreme importance.
Human intestinal epithelial cells (namely, Caco-2 and HT29-MTX cell lines) can be used as in vitro models to study the cytotoxic and genotoxic effects of TiO2 following its ingestion or a simulated digestion procedure [121]. These are less expensive, have an increased reproducibility and their outcome is more rapidly achieved in comparison with in vivo models [122]. Both referred cell lines are derived from a human epithelial colorectal adenocarcinoma. Caco-2 cell line is considered as the best characterized in vitro model for the intestinal barrier, since it mimics the most abundant cell type found in the small intestine - the absorptive enterocytes. It’s widely used in many (nano)toxicological and pharmacological studies, including drug transport and NM absorption/uptake [123,124,125]. On the other hand, HT29-MTX cells present a mucus-secreting phenotype that resembles Goblet cells, also found in the intestine [126]. The presence of a mucus layer is considered as a thick and dense physical barrier that might influence the diffusion of TiO2 in the intestine, which can be retained and consequently, reduce the possible translocation/internalization of these NMs [123].
The Caco-2 and HT29-MTX cell co-culture model can be advantageous compared to monocultures in in vitro absorption studies, since it allows to better mimic the intrinsic structure of the intestine epithelium and its physiological conditions, also increasing the robustness and reproducibility of the obtained results [124].
More complex representative models include in vivo testing in animals or human volunteer studies. The first, besides being time consuming and expensive, display significant differences in the physiology and nutrient uptake of the GIT of humans and rats, as pointed by some authors [127]. Volunteer studies may have ethical constrains and the results can be influenced by the characteristics of individuals, generally in small number [128].
Currently, there are already some studies reporting the cyto- and genotoxicity of TiO2 after a digestion process or after ingestion, upon exposure of intestinal cells, that are described in the next sections. Some recent projects addressing this issue are also underway, such as the nationally funded project INGESTnano (PTDC/SAU-PUB/29481/2017, Foundation for Science and Technology, Portugal).
6.1 Cytotoxicity of TIO2 and Ingested TIO2 In Vitro
A summary of the in vitro cytotoxicity studies related to TiO2 exposure in GIT is presented in Table 10.1, displaying 12 studies.
Regarding TiO2 cytotoxicity in intestinal cells, the majority of the studies in the Caco-2 cell line indicated absence of effects [82, 86, 88, 129]. TiO2 anatase with 215 nm was unable to produce a cytotoxic outcome on Caco-2 cells using the LDH assay (20 and 80 μg/cm2), after 4 h or 24 h exposure [129]. Also, Abbott Chalew and Schwab [86] reported no cytotoxicity in Caco-2 cells after 24 h and 48 h of exposure to P25 (80% rutile/20% anatase; 21 nm) (0–100 μg/mL) through the MTT assay. The same outcome was verified in Dorier et al. [82], after 24 h of exposure to P25 (86% anatase/14% rutile; 24 ± 6 nm), using the WST-1 assay (0–200 μg/mL). Additionally, after 24 h of exposure to rutile hydrophobic NM-103 and rutile hydrophilic NM-104 (0–256 μg/mL), Jalili et al. [88] reported no cytotoxic effects in Caco-2 differentiated monolayer cells using neutral red uptake assay. Likewise, Dorier et al. [76] reported an absence of cytotoxicity in Caco-2 cells upon 24 h exposure to A12 (95% anatase/5% rutile; 12 ± 3 nm) and R20 (90% rutile/10% anatase; 22 ± 4 nm). Conversely, using the Trypan Blue Viability test, E171 (316 ± 284.4 nm) and TiO2 (99.5% anatase; 10.25 nm) (0–143 μg/cm2) induced both a decrease in Caco-2 cell viability after 24 h of exposure to 143 μg/cm2 concentration, and to the 14.3 μg/cm2 concentration of E171 [27]. In the same experimental conditions, HCT116 cells (another human colon cancer cell line), did not show signs of cytotoxicity up to the concentration of 100 μg/cm2 [27].
There are some cytotoxicity studies performed using the HT29 cell model (i.e. non-producing mucus phenotype), following exposure to TiO2. However, studies using mucus-producing Goblet cells (HT29-MTX) are not widely used in this context, and no reports were found regarding cytotoxicity assessment upon TiO2 treatment. No cytotoxic effects were reported after 6, 24 and 48 h exposure of HT29 cells to 1–20 μg/cm2 TiO2 (anatase; < 25 nm) or to 2–10 μg/mL (anatase/rutile; 27.38 ± 5.90 nm) through the MTT assay [66, 131]. On the contrary, a 20–30% decrease in cell viability was observed after 48 h exposure of HT29 cells to higher concentrations (50 and 400 μg/mL) of TiO2 (< 20 nm), using the same assay [132]. Regarding the trypan blue exclusion test, it was also possible to detect a significant decrease of the membrane integrity and an abnormal increased percentage of apoptotic HT29 cells, after 24 h treatment to 2–10 μg/mL TiO2 [131]. This outcome can be a result of apoptotic processes activated by the uptaken or absorbed NMs [131].
More recently, Dorier et al. [82], using the WST-1 assay, verified that, after 6, 24 and 48 h of exposure, E171 (> 95% anatase; 118 ± 53 nm), P25 (86% anatase/14% rutile; 24 ± 6 nm) and A12 (> 95% anatase; 12 ± 3 nm) (0–200 ug/mL) did not induce cytotoxic effects in a co-culture system of Caco-2 and HT29-MTX intestinal cells. Later, Dorier et al. [83] described the same conclusions regarding the co-culture exposed for 24 h to the >95% anatase A12 (12 ± 3 nm), E171 (> 95% anatase; 118 ± 53 nm) and anatase-rutile mixture NM-105 (0–200 μg/mL), using the MTT assay.
As mentioned before, an important point to consider regarding the potential risk of TiO2 in food/feed is the variety of transformations that are likely to undergo when in the GIT. In this regard, some authors started to study the effects of ingested TiO2 in intestinal cell lines, following an in vitro simulated digestion process. Through the MTT assay, a slight reduction in C2BBe1 cell (a cell clone of Caco-2) viability was observed after 24 h of exposure to 10 μg/cm2 (app. 40 μg/mL) of digested anatase-rutile mixture (21 nm) [130]. Still, the authors point out that the minor cytotoxicity observed may be due to the bile salts that were adsorbed to the NMs’ surface. The digestion model used by McCracken et al. [130] had some differences compared to the most recent in vitro digestion process described by Brodkorb et al. [57]. For example, it did not include oral phase and it used other enzymes, bile salts concentrations and timepoints. Between steps, the NPs were recovered by centrifugation [130], a procedure not used in the INFOGEST 2.0 protocol.
In a distinct report by Cao et al. [134], E171 (110 nm) was submitted to two different types of in vitro simulated digestion procedure, namely the fasting food model (FFM) and the standardized food model (SFM), which was based on the American dietary. In both, it was used a GIT simulator in which the three phases of a digestion cycle are present: oral, gastric and small intestinal. More specifically, in the oral phase, E171 was mixed with simulated salivary fluid at 37 °C and inverted for only 10 seconds; on the gastric phase, the resulting product was combined with simulated gastric fluid and incubated for 2 h at 37 °C with agitation. Finally, in the small intestinal phase, the digested product was mixed with salts, bile extract and lipase that mimic the intestinal fluid and additionally incubated for 2 h at 37 °C. The obtained results showed a significant dose-dependent cytotoxicity (using the LDH assay) in a tri-culture of Caco-2/HT29-MTX/Raji B cells when exposed for 24 h to digested E171 (0.75% and 1.5% w/w), through the FFM. No significant reduction on the cell viability upon treatment with both concentrations of E171 was observed for the SFM. The authors concluded that the presence of E171 in a fasting type diet can result in cytotoxic effects [134]. Using the FFM, the LDH assay and the same tri-cellular model, Cao et al. [133] also assessed the potential combined effects of TiO2 (E171) and the pesticide boscalid in food. Exposure to digested E171 alone (1% w/w) and boscalid at 10 ppm, with or without E171 (1% w/w), only led to the induction of a slight cytotoxicty after 24 h. By contrast, 150 ppm boscalid in the presence of 1% w/w E171 digesta caused a reduction on the cell viability (22.6% cytotoxicity) level and was significantly more cytotoxic (p < 0.01) than digesta from FFM with 150 ppm boscalid alone [133]. Also, under the nationally funded project INGESTnano (PTDC/SAU-PUB/29481/2017, Foundation for Science and Technology, Portugal), the cytotoxicity of TiO2 was analyzed in Caco-2 cells, after a harmonized in vitro simulated digestion process. The TiO2 selected for this study was NM-102 (provided by Joint Research Center, Ispra, Italy; anatase; 22 nm). Preliminary studies using the MTT assay in Caco-2 cells exposed for 24 h to NM concentrations ranging from 0–48 μg/mL revealed a marked cytotoxicity at the highest concentrations (Fig. 10.3). This cytotoxicity was observed also in the negative controls of the digestion, where only solvent without NM was applied (cell culture medium with sterile-filtered 0.05 wt % BSA-water with 0.5% absolute ethanol, in the same proportion as in the NM samples).
Results of the cell viability assay in Caco-2 cells, showing cytotoxic effects as a function of the concentration of the digestion product (DIG product, %) without NM (DIG0), both with or without pefabloc, and comparison with the digestion product with NM (DIG-102) or the undigested NM (NM-102). Pefabloc is a reagent included in the last steps of the in vitro digestion process to inhibit enzymatic activity of the digestion mixture reagents
The results revealed that digestion products without the NM induced cytotoxic effects above the concentration equivalent to 20 μg/mL (>12.5% of digestion product) in cell culture medium, challenging the applicability of the digestion product in further biological assays. Conversely, no cytotoxicity was observed when cells were exposed to NM-102, without the simulated digestion process. It was thus concluded that the digestion product per se was cytotoxic and that the enzyme inhibitor pefabloc, added in the final step of simulated digestion, was not the source of this toxicity (Fig. 10.3). Likewise, changes in pH and/or osmolality were discarded as cause of DIG toxicity (results not shown).
When performing a digestion without adding bile salts (DIG0-mod), the results suggested that the addition of bile salts accounted for most of the toxicity observed (Fig. 10.4). This was verified when comparing the cytotoxic effects of digestion product without bile salts (DIG0-mod) with normal digestion procedure, DIG0 (Fig. 10.4), where a significant difference was observed in cytotoxicty (p < 0.05, Student’s t-test).
The fact that the in vitro human simulated digestion by Brodkorb et al. [57] requires a concentration of bile salts 166-fold higher than the concentration used by McCracken et al. [130] can justify the different toxicity observed for the same concentration tested in intestinal cells (40 μg/mL). This increased concentration of bile salts is based on the normal physiological values found in a human adult intestine [57, 58]. In addition, McCracken et al. [130] used purification by centrifugation, possibly further reducing the bile salts content before adding it to cells. Indeed, other authors also pointed out that bile salts present in digestion product could be considered cytotoxic [50, 135]. However, the introduction of a purification step in the digestion protocol used may lead to the loss of NM in the digestion product, as well to further modifications in the NMs’ properties that do not reflect a realistic situation.
It was concluded that, at a concentration range below 12.5% of digestion product (corresponding to 28 μg/mL of NM), even using bile salts, the harmonized digestion method could be used for addressing the toxicity of ingested NMs. In addition, the literature suggests that concentrations of 0.14 μg/mL of TiO2 are physiologically relevant for intestinal cells [65], so such levels of concentration was used for further experiments without concerns of cytotoxic effects due to interference of the digestion reagents. Having these findings in consideration, further studies of the toxic effects of three different TiO2 (NM-103, NM-103 and NM-105) on the gastrointestinal tract cells, Caco-2 and HT29-MTX-E12, were investigated, with the application of the standardized static INFOGEST 2.0 in vitro digestion method to mimic human digestion of TiO2. The most recent results showed that, among these three NMs, the digested NM-105 (anatase-rutile) showed an increased toxicity in HT29-MTX-E12 cells, compared to undigested NM. This difference was accompanied with subtle changes in secondary characteristics of this NM [59].
6.2 Cytotoxicity of Ingested TIO2 In Vivo
Few studies related to the study of the in vivo cytotoxicity of ingested or orally administered TiO2 using animal models have been reported and are summarized in Table 10.2.
In the Sycheva et al. [136] work, nanosized TiO2 (33.2 ± 16.7 nm) was administered daily for 7 days (40, 200 and 1000 mg/kg bw) to male mice. No cytogenetic effects were induced in the forestomach, colon and testis cells after exposure; on the contrary, upon treatment with the 40 mg/kg bw dose, a significant increase in the mitotic index was observed in forestomach and colon epithelia. Furthermore, an augmented mitotic activity in the colon at the 200 mg/kg bw and an increased apoptotic level at the highest concentration were detected [136].
An induction of the apoptosis pathway (assessed through the Bax and p53 gene expression) in the intestine and liver cells was observed in rats treated orally to 10, 50 and 100 mg/kg bw TiO2 following a 30-day exposure. Nonetheless, an activity of other biochemical parameters such as alanine aminotransferase (ALT), aspartate aminotransferase (ASP), lactate dehydrogenase (LDH) and alkaline phosphatase (ALP) were increased in all previous concentrations [61].
More recently, through oral gavage, Wister rats were exposed to 20 and 40 μg/mL bw of E171 daily for 90 consecutive days [94]. Two cytotoxic parameters were assessed, more specifically, the lymphocyte transformation and the determination of the LDH activity. A significant decrease in the lymphocyte proliferation was reported when compared to the control untreated group. Nevertheless, an increase of the LDH release was detected for both concentrations, following a linear and a quadratic increment [94].
In other animal model, namely Drosophila melanogaster, an induction of cytotoxic effects on midgut and imaginal disc tissues of larvae was detected in vivo after an 24 and 48 h oral exposure to 0.8 or 1.60 mg/mL TiO2 (anatase; < 25 nm), through the trypan blue dye exclusion test [137].
6.3 Genotoxicity of TIO2 and Ingested TIO2 In Vitro
As previously mentioned, the in vitro comet and the cytokinesis-blocked micronucleus (CBMN) assays are frequently used in the genotoxicity assessment of intestinal epithelial cells exposed to TiO2, but other assays such as mutation assays or chromosomal aberration tests, or even oxidative DNA damage assays can be used. Concerning the in vitro methods referred, different results have been reported after TiO2 exposure, mainly due to the distinct concentrations and primary sizes of the tested TiO2 or related to the exposure conditions. A review on genotoxic effects of TiO2 that includes other cell types and routes of administration not related to GIT, can be found in the recent EFSA report [28]. In the next sections, we focus on the effects related to GIT.
Table 10.3 synthetizes the reports in the literature corresponding to the in vitro genotoxicity assessment following exposure of intestinal epithelial cells to TiO2. No significant genotoxic effects were induced in the Caco-2 cell line exposed for 4 h to 20 μg/cm2 TiO2 (anatase, 6.7 ± 1.3 nm; anatase, 3.94 ± 0.05 nm; 90% anatase/10% rutile; 21.90 ± 0.30 nm), using the conventional and FPG-modified comet assays [129]. With the same assay, Dorier et al. [76] did not report increased DNA strand breaks after 6 h, 24 h and 48 h exposure of Caco-2 cells to 50 μg/mL of an anatase TiO2 (particle size of 12 ± 3 nm) or to a rutile TiO2 (22 ± 4 nm). In these two studies, the reports of the exposure in different units (μg/mL or μg/cm2) hamper the comparison between the different results mentioned, although in this case it is evident that the particle size did not induce differences in terms of genotoxicity. Furthermore, no genotoxic effects were reported in the conventional alkaline comet assay by Dorier et al. [82] after an acute 6 h, 24 h or 48 h exposure to 10 and 50 μg/mL P25 (86% anatase/14% rutile; 24 ± 6 nm), A12 (95% anatase/5% rutile; 12 ± 3 nm) and E171 (>95% anatase; 118 ± 53 nm). Likewise, a 21-day repeated exposure to the same TiO2 did not induce significant DNA damage in Caco-2 cells [82, 83].
Contradictory results were obtained for Caco-2 cells exposed for 21-days to E171 (10 and 50 μg/mL), in which a moderate genotoxicity was observed, using the FPG-modified comet assay [82]. Furthermore, through the conventional alkaline comet assay, the NanoGenotox Joint action reported that three TiO2 produced by the JRC repository, namely NM-102 (anatase; 22 nm), NM-103 (rutile hydrophobic; 25 nm) and NM-105 (81.5% anatase/19.5% rutile; 30 nm) induced genotoxic damage in Caco-2 cells (0–256 μg/mL concentration range), after 24 h exposure; conversely, treatment of the same cell type with the rutile hydrophilic NM-104 (25 nm) did not induce a significant level of DNA damage [138]. These results suggest that the hydrophobic or hydrophilic nature of NMs with the same primary size can greatly influence the genotoxicity outcome; besides, NMs with the same size but with distinct crystalline phases can lead to distinct outcomes regarding genotoxic damage. In the same work, no significant increased DNA strand break level was observed after just 3 h of exposure to any of the NMs referred to [138]. Zijno et al. [78] also reported an increase of the DNA damage concerning Caco-2 cells exposed to 1 and 2.5 μg/cm2 of anatase TiO2 (< 25 nm) with the conventional comet assay and its combination with the FPG and EndoIII enzymes. Despite experiments with four different exposure hours – 2, 4, 6 and 24 h - most of the genotoxicity outcomes were obtained at shorter exposure times and only one positive result was verified at the time of 24 h. In this sense, the author suggests that after 24 h of exposure to TiO2, Caco-2 cells can repair the DNA and oxidative lesions [78]. Consequently, the time of exposure can interfere tremendously with the final genotoxic result.
In a monolayer of differentiated Caco-2 cells model, Vila et al. [139] did not observe the induction of oxidative damage through the FPG version of the comet assay upon treatment with 10, 25 and 100 μg/mL of JRC NM-100 (104.01 ± 39.49 nm) for 24 h. Nonetheless, exposure to 10 μg/mL showed a slight genotoxicity DNA damage (increased DNA strand break level) through the conventional alkaline comet assay. This can be explained as the higher the concentration of TiO2, the greater their tendency to form aggregates in the cell culture medium. Then, TiO2 may remain attached to the extracellular membrane of Caco-2 cells, not being able to be internalized and to have contact with the cell nucleus, preventing the possibility of causing DNA damage at higher concentrations [140]. Likewise, Jalili et al. [88] reported no significant increase in DNA damage in a Caco-2 differentiated monolayer following a 24 h exposure to higher concentrations (0–256 μg/mL) of JRC benchmark NM-103 (rutile hydrophobic; 25 nm) and NM-104 (rutile hydrophilic; 25 nm), using the conventional and FPG-modified comet assays.
Regarding the CBMN assay, the majority of the reports show no genotoxic effects after exposure to TiO2. No significant chromosome damage effects were observed in Caco-2 cells after 52 h of treatment to 0–256 μg/mL NM-102, NM-103, NM-104 and NM-105 (all obtained from JRC), assessed by the CBMN assay [138]. Following a 6 and 24 h exposure to 1–20 μg/cm2 of anatase TiO2 (< 25 nm), no increase in the frequency of micronucleated cells was detected in Caco-2 cells [78]. Furthermore, Jalili et al. [88] observed also no clastogenic or aneugenic effects, evaluated through the CBMN assay, following a 24 h exposure to NM-103 (rutile hydrophobic; 25 nm) and NM-104 (rutile hydrophilic; 25 nm) (0–256 μg/mL) considering a Caco-2 differentiated monolayer. It is therefore possible to conclude that all mentioned studies did not report an increase in the frequency of micronuclei in Caco-2 cells following exposure to nano-sized TiO2. Nevertheless, there are still few studies related to this assay performed with intestinal epithelial cell lines, namely Caco-2, that allow definitive conclusions to be drawn regarding the capacity of TiO2 to induce chromosomal damage in the GIT. More experimental tests should then be performed in order to predict the behavior of these NMs in the GIT and to be able to draw a safe conclusion about their possible DNA or chromosomal damage ability in intestinal cells.
As with cytotoxicity assays, no studies on genotoxicity in HT29-MTX cells were found in the literature, but only in its non-mucus-producing phenotype (HT29 colorectal adenocarcinoma cells). Nevertheless, only one study was found regarding genotoxicity assessment (more specifically, the conventional and FPG-modified comet assay) in HT29 cells. This may be due to the fact that the Caco-2 cell line is currently the most applied in vitro model of the intestinal barrier for toxicological studies, since it resembles the most common type of cells in the small intestine, namely the absorptive enterocytes. After 24 h exposure of HT29 cells to an anatase/rutile mixture of TiO2 (27.38 ± 5.90 nm) (2–10 μg/mL), no significant increase in the DNA strand break level was observed evaluated by the conventional comet assay; conversely, an increase of the oxidative damage level was reported upon treatment with the 8 and 10 μg/mL concentrations. [131].
As already mentioned, the presence of a co-culture model comprising Caco-2 and HT29-MTX cells enable to better mimic the structure and physiological properties of the intestinal barrier. This allows it to be a more reliable and reproducible in vitro model in toxicological assessment studies as it is closer to the physiological condition of the human intestine. A co-culture of Caco-2 and HT29-MTX cells was exposed for 6 h, 24 h and 48 h or chronically for 21 days (three times a week for 3 weeks) to three different types of TiO2 (P25, A12 and E171) in two different concentrations – 10 and 50 μg/mL [82]. The conventional and FPG-modified comet assays were used and showed that only the highest concentration of E171 (50 μg/mL), induced a significant increase in oxidative purine lesions and alkali-labile sites, but no the DNA strand break level, following a chronic exposure [82]. Using the same assay and the same benchmark NMs at a concentration of 50 μg/mL, no DNA damage was detected in a co-culture of Caco-2 and HT29-MTX cells following only 24 h of exposure [83].
Through the mouse lymphoma gene mutation assay and using L5178Y cells, no increase of the mutation frequency was verified after 4 h and 24 h exposure to 40 nm TiO2 (0.0312–2 μg/mL) [141]. On the contrary, a linear increase in the mutation frequency was observed in WIL2-NS cells following incubation with 0, 25, 65 and 130 g/mL TiO2 (< 100 nm) for 6, 24 and 48 h, using the hypoxanthine-guanine phosphoribosyltransferase (HPRT) gene mutation assay [142].
As can be seen, inconsistent results are found in the literature concerning the in vitro genotoxicity assessment of TiO2. The conflicting results can be explained by the different crystalline phase, size, exposure time and concentration used in each genotoxicity assay. Besides that, the different methods applied, the NMs dispersion procedure or even the exposure units referred to in reports (μg/mL or μg/cm2) might influence critically the toxicological outcome. Due to the lack of harmonization in these procedures, a more detailed and in-depth investigation is needed in order to infer whether the ingested TiO2 are genotoxic. No reports were found regarding the genotoxicity testing of nanosized TiO2 following in vitro simulated digestion, that could provide an advancement for a more realistic approach.
6.4 Genotoxicity of Ingested TIO2 In Vivo
Although in vivo tests should be avoided, in vitro genotoxicity positive outcomes require confirmation by an appropriate follow-up in vivo. This is needed since this type of tests offers a more realistic approach, thus allowing a better prediction of biological responses of organisms to test agents like TiO2, in spite of species-specific differences already mentioned. Table 10.4 summarizes the reports found in the literature regarding the in vivo genotoxic effects of ingested TiO2.
Mice treated orally with TiO2 (anatase, 20–50 nm), for 14 days in a range of concentrations of 10–100 mg/kg bw, led to a statistically significant dose-dependent increase in the % of DNA in tail in the liver cells, evaluated through the comet assay. In the same study, using the CBMN assay, an increase of micronuclei frequency in bone marrow cells was observed only after treatment with the highest concentration - 100 mg/kg bw [145]. Conversely, the exposure of rats by oral gavage during 45 days to 0.5 mg/kg/day TiO2 (41.99 ± 1.63 nm) did not show DNA damage in blood or liver cells [148]. The exposure to 500 mg/kg bw of P25 (75% anatase/25% rutile; 21 nm) for 5 days, led to an increase in the frequency of micronucleated binucleated cells in peripheral blood cells of mice [92]. Furthermore, Manivannan et al. [149] reported genotoxic and clastogenic effects in multiple organs of Swiss albino male mice treated orally with sub-acute concentrations (0.2, 0.4 and 0.8 mg/kg bw) of rutile TiO2 (25 nm) over a period of 28 days. Long-term exposure to low concentrations of rutile TiO2 induced DNA damage in organs such as liver, spleen, and thymus. Chromosomal aberration test in bone marrow cells revealed the clastogenicity of TiO2 at sub-chronic low concentrations [149]. In fact, Wang et al. [54, 142] already had verified that TiO2 accumulate in the liver of rats after 2 weeks of oral exposure to a dose of 5 g/kg bw. This suggests that after ingested and internalized by the GIT, TiO2 might be transported to other tissues and organs, being the liver a possible target organ for the digested TiO2. This idea is reinforced by Heringa et al. [38] work, where both Ti and TiO2 were found in the human liver and the spleen analyzed post-mortem and, wherein at least 24% of the particles found (≥ 24%) were nanometric (< 100 nm), as already mentioned in this chapter.
Biopersistence of TiO2 in gut cells can possibly induce damage associated to cancer events. We take the example of Urrutia-Ortega et al. [107] and Bettini et al. [45] works, where the exposure to E171 induced tumor formation in the distal colon, as well as preneoplastic lesions and growth of aberrant crypt foci in rats [45, 107]. In spite Bettini reports were not replicated in subsequent studies Blevins et al. [150], the uncertainty of the consequences of the genotoxicity observed in most studies raise major concerns. The recent report by EFSA clearly states that, on balance TiO2 have the potential to induce chromosomal and DNA damage, and considering the fact that “genotoxicity concern could not be ruled out”, the Panel concluded that “E171 can no longer be considered as safe when used as a food additive “[28]. Furthermore, it is evident that physicochemical properties of NMs might influence the cytotoxic and genotoxic outcome, and other uses of TiO2 aside from E171, should be reconsidered. These observations show that it is essential to continue studying the possible genotoxic and cytotoxic effects, in order to verify if their oral consumption/intake is safe for human health.
7 Final Remarks/Perspectives
In this chapter, we showed the extensive work that has been reported worldwide for assessing the cellular and molecular mechanisms of toxicity of TiO2, with the purpose of assuring its safety for use in promising applications. In spite many of these applications rely on food and feed products, the risk analysis often disregards the impact of the ingestion process in the TiO2 toxicological outcomes. To this regard, knowledge gaps have been identified, concerning: (i) the modifications of the TiO2 throughout the GIT, upon interaction with digestion fluids; (ii) how these modifications can facilitate/block the systemic absorption of the TiO2; (iii) conclusive evidence of key molecular events that may lead to adverse outcomes; (iv) adverse outcomes such as genotoxicity and cancer, that can be most relevant after long term exposure to low doses.
In this context, the application of an in vitro digestion process for TiO2 can be considered a valuable tool. This is an innovative approach and currently there are no reports in literature related to the genotoxic potential of digested TiO2 in intestinal cells. To better integrate the modifications that NMs suffer in the organism, the addition of a simulated digestion process in the safety evaluation of ingested NMs used in vitro bioassays can provide a significant improvement on existing approaches [59], that may decrease uncertainties in the hazard assessment of ingested NMs. The added value of in vitro simulated GIT models has been highlighted in EFSA nanoguidance [25], but this outlook also emphasizes the need for a comprehensive in vitro-in vivo integrated approach associated to the use of documented dispersion protocols, concomitantly with a comprehensive physicochemical characterization of the test material in each case. Furthermore, the use of advanced multidimensional cellular models, such as co-cultures and 3D-cell cultures, with the inclusion of a multitude of individual factors that approximates in vivo conditions [60], as well as molecular screening and epigenetic endpoints, may provide additional information and a relevant alternative to animal experiments, at an early stage of safety assessment of NMs and in product development of NMs intended for human ingestion. By providing a screening tool for industry, a safe-by-design approach to the development of innovative NMs is foreseen in the near future.
References
Louro H, Borges T, Silva MJ (2013) Nanomateriais manufaturados: novos desafios para a saúde pública. Rev Portuguesa de Saude Pub 31. https://doi.org/10.1016/j.rpsp.2012.12.004
He X, Deng H, Hwang H, min. (2019) The current application of nanotechnology in food and agriculture. J Food Drug Anal 27(1):1–21. https://doi.org/10.1016/j.jfda.2018.12.002
Peters RJB, Bouwmeester H, Gottardo S, Amenta V, Arena M, Brandhoff P et al (2016) Nanomaterials for products and application in agriculture, feed and food. Trends Food Sci Technol 54:155–164. https://doi.org/10.1016/j.tifs.2016.06.008
Chaudhry Q, Scotter M, Blackburn J, Ross B, Boxall A, Castle L et al (2008) Applications and implications of nanotechnologies for the food sector. Food Addit Contaminants 25(3):241–258. https://doi.org/10.1080/02652030701744538
Weir A, Westerhoff P, Fabricius L, Hristovski K, Von Goetz N (2012) Titanium dioxide nanoparticles in food and personal care products. Environ Sci Technol 46(4):2242–2250. https://doi.org/10.1021/es204168d
Winkler HC, Notter T, Meyer U, Naegeli H (2018) Critical review of the safety assessment of titanium dioxide additives in food. J Nanobiotechnol 16. https://doi.org/10.1186/s12951-018-0376-8
Athinarayanan J, Periasamy VS, Alsaif MA, Al-Warthan AA, Alshatwi AA (2014) Presence of nanosilica (E551) in commercial food products: TNF-mediated oxidative stress and altered cell cycle progression in human lung fibroblast cells. Cell Biol Toxicol 30(2):89–100. https://doi.org/10.1007/s10565-014-9271-8
Jampilek J, Kos J, Kralova K (2019) Potential of nanomaterial applications in dietary supplements and foods for special medical purposes. Nano 9(2). https://doi.org/10.3390/nano9020296
Cao Y (2017) Toxicity of ingested nanomaterials. In: A. A. Press (ed) Food toxicology current advances and future challenges, pp 348–355. https://doi.org/10.1201/b13390-38
Xun W, Shi L, Yue W, Zhang C, Ren Y, Liu Q (2012) Effect of high-dose nano-selenium and selenium-yeast on feed digestibility, rumen fermentation, and purine derivatives in sheep. Biol Trace Elem Res 150:130–136. https://doi.org/10.1007/s12011-012-9452-3
Fondevila M, Herrer R, Casallas MC, Abecia L, Ducha JJ (2009) Silver nanoparticles as a potential antimicrobial additive for weaned pigs. Anim Feed Sci Technol 150(3–4):259–269. https://doi.org/10.1016/j.anifeedsci.2008.09.003
Gholami-Ahangaran M, Zia-Jahromi N (2013) Nanosilver effects on growth parameters in experimental aflatoxicosis in broiler chickens. Toxicol Ind Health 29(2):121–125. https://doi.org/10.1177/0748233711425078
Pineda L, Chwalibog A, Sawosz E, Lauridsen C, Engberg R, Elnif J et al (2012) Effect of silver nanoparticles on growth performance, metabolism and microbial profile of broiler chickens. Arch Anim Nutr 66(5):416–429. https://doi.org/10.1080/1745039X.2012.710081
Khin MM, Nair AS, Babu VJ, Murugan R, Ramakrishna S (2012) A review on nanomaterials for environmental remediation. Energy Environ Sci 5(8):8075–8109. https://doi.org/10.1039/c2ee21818f
Amenta V, Aschberger K, Arena M, Bouwmeester H, Botelho Moniz F, Brandhoff P et al (2015) Regulatory aspects of nanotechnology in the Agri/feed/food sector in EU and non-EU countries. Regul Toxicol Pharmacol 73(1):463–476. https://doi.org/10.1016/j.yrtph.2015.06.016
Peters R, Kramer E, Oomen AG, Herrera Rivera ZE, Oegema G, Tromp PC et al (2012) Presence of nano-sized silica during in vitro digestion of foods containing silica as a food additive. ACS Nano 6(3):2441–2451. https://doi.org/10.1021/nn204728k
European Commission (2011) Commission Regulation (EU) No 10/2011 of 14 January 2011 on plastic materials and articles intended to come into contact with food. Official Journal of the European Union
Dizaj SM, Lotfipour F, Barzegar-Jalali M, Zarrintan MH, Adibkia K (2014) Antimicrobial activity of the metals and metal oxide nanoparticles. Mater Sci Eng C 44:278–284. https://doi.org/10.1016/j.msec.2014.08.031
Li W, Li X, Zhang P, Xing Y (2011) Development of nano-ZnO coated food packaging film and its inhibitory effect on Escherichia coli in vitro and in actual tests. Adv Mater Res 152–153:489–492. https://doi.org/10.4028/www.scientific.net/AMR.152-153.489
Honarvar Z, Hadian Z, Mashayekh M (2016) Nanocomposites in food packaging applications and their risk assessment for health. Electron Physician 8(6):2531–2538. https://doi.org/10.19082/5212
Cubadda F (2019) Chapter 4: Exposure to substances via food consumption: nanoparticles in food. In: Heinemeyer G, Jantunen M, Hakkinen P (eds) The practice of consumer exposure assessment. Springer, pp 323–359
Sahoo D, Mandal A, Mitra T, Chakraborty K, Bardhan M, Dasgupta AK (2018) Nanosensing of pesticides by zinc oxide quantum dot: an optical and electrochemical approach for the detection of pesticides in water. J Agric Food Chem 66(2):414–423. https://doi.org/10.1021/acs.jafc.7b04188
Sun Y, Fang L, Wan Y, Gu Z (2018) Pathogenic detection and phenotype using magnetic nanoparticle-urease nanosensor. Sensors Actuators B Chem 259:428–432. https://doi.org/10.1016/j.snb.2017.12.095
Zhang W, Han Y, Chen X, Luo X, Wang J, Yue T, Li Z (2017) Surface molecularly imprinted polymer capped Mn-doped ZnS quantum dots as a phosphorescent nanosensor for detecting patulin in apple juice. Food Chem 232:145–154. https://doi.org/10.1016/j.foodchem.2017.03.156
EFSA Scientific Committee, Hardy A, Benford D, Halldorsson T, Jeger MJ, Knutsen HK, More S, Naegeli H, Noteborn H, Ockleford C, Ricci A, Rychen G, Schlatter JR, Silano V, Solecki R, Turck D, Younes M, Chaudhry Q, Cubadda F, Gott D, Oomen A, Weigel S, Karamitrou M, Schoonjans R, Mortensen A (2018) Guidance on risk assessment of the application of nanoscience and nanotechnologies in the food and feed chain: part 1, human and animal health. EFSA J 16(7):5327. https://doi.org/10.2903/j.efsa.2018.5327
European Commission (2012) Commission Regulation (EU) No 231/2012 of 9 March 2012 laying down specifications for food addtives listed in Annexes II and III to Regulation (EC) No 1333/2008 of the European Parliament and of the Council. Official Journal of the European Union (vol. 83). https://doi.org/10.1201/9781315152752
Proquin H, Rodríguez-Ibarra C, Moonen CGJ, Urrutia Ortega IM, Briedé JJ, de Kok TM et al (2016) Titanium dioxide food additive (E171) induces ROS formation and genotoxicity: contribution of micro and nano-sized fractions. Mutagenesis 32(1):139–149. https://doi.org/10.1093/mutage/gew051
EFSA Panel on Food Additives and Flavourings, Younes M, Aquilina G, Castle L, Engel K-H, Fowler P, Frutos Fernandez MJ, Furst P, Gundert-Remy U, Gurtler R, Husøy T, Manco M, Mennes W, Moldeus P, Passamonti S, Shah R, Waalkens-Berendsen I, Wolfle D, Corsini E, Cubadda F, De Groot D, FitzGerald R, Gunnare S, Gutleb AC, Mast J, Mortensen A, Oomen A, Piersma A, Plichta V, Ulbrich B, Van Loveren H, Benford D, Bignami M, Bolognesi C, Crebelli R, Dusinska M, Marcon F, Nielsen E, Schlatter J, Vleminckx C, Barmaz S, Carfı M, Civitella C, Giarola A, Rincon AM, Serafimova R, Smeraldi C, Tarazona J, Tard A, Wright M (2021) Scientific opinion on the safety assessment of titanium dioxide (E171) as a food additive. EFSA J 19(5):6585. https://doi.org/10.2903/j.efsa.2021.6585
Verleysen E, Waegeneers N, Brassinne F, De Vos S, Jimenez IO, Mathioudaki S, Mast J (2020) Physicochemical characterization of the pristine E171 food additive by standardized and validated methods. Nano 10(3):592. https://doi.org/10.3390/nano10030592
DeLoid GM, Cohen JM, Pyrgiotakis G, Demokritou P (2017a) An integrated dispersion preparation, characterization and in vitro dosimetry methodology for engineered nanomaterials. Nat Protoc 12(2):335–371. https://doi.org/10.1038/nprot.2016.172
Shi H, Magaye R, Castranova V, Zhao J (2013) Titanium dioxide nanoparticles: a review of current toxicological data. Part Fibre Toxicol 10(15):1–33
Martirosyan A, Schneider YJ (2014) Engineered nanomaterials in food: implications for food safety and consumer health. Int J Environ Res Public Health 11(6):5720–5750. https://doi.org/10.3390/ijerph110605720
EFSA (2016) Re-evaluation of titanium dioxide (E 171) as a food additive. EFSA J 14(9):1–83. https://doi.org/10.2903/j.efsa.2016.4545
Rompelberg C, Heringa MB, van Donkersgoed G, Drijvers J, Roos A, Westenbrink S et al (2016) Oral intake of added titanium dioxide and its nanofraction from food products, food supplements and toothpaste by the Dutch population. Nanotoxicology 10(10):1404–1414. https://doi.org/10.1080/17435390.2016.1222457
Sprong C, Bakker M, Niekerk M, Vennemann F (2015) Exposure assessment of the food additive titanium dioxide (E 171) based on use levels provided by the industry. National Institute for Public Health and the Environment, Bilthoven
Pele LC, Thoree V, Bruggraber SFA, Koller D, Thompson RPH, Lomer MC, Powell JJ (2015) Pharmaceutical/food grade titanium dioxide particles are absorbed into the bloodstream of human volunteers. Part Fibre Toxicol 12(1):1–6. https://doi.org/10.1186/s12989-015-0101-9
Böckmann J, Lahl H, Eckert T, Unterhalt B (2000) Blood titanium levels before and after oral administration titanium dioxide. Pharmazie 55(2):140–143
Heringa MB, Peters RJB, Bleys RLAW, van der Lee MK, Tromp PC, van Kesteren PCE et al (2018) Detection of titanium particles in human liver and spleen and possible health implications. Part Fibre Toxicol 15(1):15. https://doi.org/10.1186/s12989-018-0251-7
Bettini S, Houdeau E (2014) Exposition orale aux nanoparticules de dioxyde de titane (TiO2): du franchissement de l’épithélium buccal et intestinal au devenir et aux effets dans l’organisme. Biol Aujourdhui 208(2):167–175. https://doi.org/10.1051/jbio/20140022
Skocaj M, Filipic M, Petkovic J, Novak S (2011) Titanium dioxide in our everyday life; is it safe? Radiol Oncol 45(4):227–247. https://doi.org/10.2478/v10019-011-0037-0
Talamini L, Gimondi S, Violatto MB, Fiordaliso F, Pedica F, Tran NL, Sitia G, Aureli F, Raggi A, Nelissen I, Cubadda F, Bigini P, Diomede L (2019) Repeated administration of the food additive E171 to mice results in accumulation in intestine and liver and promotes an inflammatory status. Nanotoxicology 13(8):1087–1101. https://doi.org/10.1080/17435390.2019.1640910
Lyon F (2010) IARC monographs on the evaluation of carcinogenic risks to humans VOLUME 93 carbon black, titanium dioxide, and talc
Bernauer U, Chaudhry Q, Dusinska M, Lilienblum W, Platzek T, van Benthem J et al (2015) Opinion of the Scientific Committee on Consumer safety (SCCS) - revision of the opinion on the safety of the use of titanium dioxide, nano form, in cosmetic products. Regul Toxicol Pharmacol 73. https://doi.org/10.1016/j.yrtph.2015.09.005
ANSES (2019) AVIS de l’Agence nationale de sécurité sanitaire de l’alimentation, de l’environnement et du travail relatif aux risques liés à l’ingestion de l’additif alimentaire E171, Maisons-Alfort
Bettini S, Boutet-Robinet E, Cartier C, Coméra C, Gaultier E, Dupuy J et al (2017) Food-grade TiO2 impairs intestinal and systemic immune homeostasis, initiates preneoplastic lesions and promotes aberrant crypt development in the rat colon. Sci Rep 7. https://doi.org/10.1038/srep40373
Louro H (2018) Relevance of physicochemical characterization of nanomaterials for understanding nano-cellular interactions. Adv Exp Med Biol 1048. https://doi.org/10.1007/978-3-319-72041-8_8
Louro H, Saruga A, Santos J, Pinhão M, Silva MJ (2019) Biological impact of metal nanomaterials in relation to their physicochemical characteristics. Toxicol In Vitro 56. https://doi.org/10.1016/J.TIV.2019.01.018
Yusoff R, Kathawala MH, Nguyen LTH, Setyawati MI, Chiew P, Wu Y et al (2018) Biomolecular interaction and kinematics differences between P25 and E171 TiO2 nanoparticles. NanoImpact 12(August):51–57. https://doi.org/10.1016/j.impact.2018.10.001
Zhang Z, Zhang R, Xiao H, Bhattacharya K, Bitounis D, Demokritou P, McClements DJ (2019) Development of a standardized food model for studying the impact of food matrix effects on the gastrointestinal fate and toxicity of ingested nanomaterials. NanoImpact 13–25. https://doi.org/10.1016/j.impact.2018.11.002
DeLoid GM, Wang Y, Kapronezai K, Lorente LR, Zhang R, Pyrgiotakis G et al (2017b) An integrated methodology for assessing the impact of food matrix and gastrointestinal effects on the biokinetics and cellular toxicity of ingested engineered nanomaterials. Part Fibre Toxicol 14. https://doi.org/10.1186/s12989-017-0221-5
Avramescu M-L, Rasmussen PE, Chénier M, Gardner HD (2017) Influence of pH, particle size and crystal form on dissolution behaviour of engineered nanomaterials. Environ Sci Pollut Res 24:1553–1564. https://doi.org/10.1007/s11356-016-7932-2
Kreyling WG, Holzwarth U, Schleh C, Kozempel J, Wenk A, Haberl N et al (2017) Quantitative biokinetics of titanium dioxide nanoparticles after oral application in rats: part 2. Nanotoxicology 11. https://doi.org/10.1080/17435390.2017.1306893
MacNicoll A, Kelly M, Aksoy H, Kramer E, Bouwmeester H, Chaudhry Q (2015) A study of the uptake and biodistribution of nano-titanium dioxide using in vitro and in vivo models of oral intake. J Nanopart Res 17(2):1–20. https://doi.org/10.1007/s11051-015-2862-3
Wang J, Zhou G, Chen C, Yu H, Wang T, Ma Y et al (2007b) Acute toxicity and biodistribution of different sized titanium dioxide particles in mice after oral administration. Toxicol Lett 168(2):176–185. https://doi.org/10.1016/j.toxlet.2006.12.001
Sohal IS, Cho YK, O’Fallon KS, Gaines P, Demokritou P, Bello D (2018a) Dissolution behavior and biodurability of ingested engineered nanomaterials in the gastrointestinal environment. ACS Nano 12(8):8115–8128. https://doi.org/10.1021/acsnano.8b02978
Tan Y, Li R, Liu C, Muriel Mundo J, Zhou H, Liu J, McClements DJ (2020) Chitosan reduces vitamin D bioaccessibility in food emulsions by binding to mixed micelles. In: Food and function, vol 11. Royal Society of Chemistry, pp 187–199. https://doi.org/10.1039/c9fo02164g
Brodkorb A, Egger L, Alminger M, Alvito P, Assunção R, Ballance S et al (2019) INFOGEST static in vitro simulation of gastrointestinal food digestion. Nat Protoc 14. https://doi.org/10.1038/s41596-018-0119-1
Minekus M, Alminger M, Alvito P, Ballance S, Bohn T, Bourlieu C et al (2014) A standardised static in vitro digestion method suitable for food-an international consensus. Food Function 5:1113–1124. https://doi.org/10.1039/c3fo60702j
Bettencourt A, Gonçalves LM, Gramacho AC, Vieira A, Rolo D, Martins C et al (2020) Analysis of the characteristics and cytotoxicity of titanium dioxide nanomaterials following simulated in vitro digestion. Nano 10(8):1516. https://doi.org/10.3390/nano10081516
Kämpfer AAM, Busch M, Schins RPF (2020) Advanced in vitro testing strategies and models of the intestine for Nanosafety research. Chem Res Toxicol 33. https://doi.org/10.1021/acs.chemrestox.0c00079
Abbasi-Oshaghi E, Mirzaei F, Pourjafar M (2019) NLRP3 inflammasome, oxidative stress, and apoptosis induced in the intestine and liver of rats treated with titanium dioxide nanoparticles: in vivo and in vitro study. Int J Nanomedicine 14:1919–1936. https://doi.org/10.2147/IJN.S192382
Faust JJ, Doudrick K, Yang Y, Westerhoff P, Capco DG (2014) Food grade titanium dioxide disrupts intestinal brush border microvilli in vitro independent of sedimentation. Cell Biol Toxicol 30(3):169–188. https://doi.org/10.1007/s10565-014-9278-1
Guo Z, Martucci NJ, Moreno-Olivas F, Tako E, Mahler GJ (2017) Titanium dioxide nanoparticle ingestion alters nutrient absorption in an in vitro model of the small intestine. NanoImpact 5:70–82. https://doi.org/10.1016/j.impact.2017.01.002
Koeneman BA, Zhang Y, Westerhoff P, Chen Y, Crittenden JC, Capco DG (2010) Toxicity and cellular responses of intestinal cells exposed to titanium dioxide. Cell Biol Toxicol 26(3):225–238. https://doi.org/10.1007/s10565-009-9132-z
Richter JW, Shull GM, Fountain JH, Guo Z, Musselman LP, Fiumera AC, Mahler GJ (2018) Titanium dioxide nanoparticle exposure alters metabolic homeostasis in a cell culture model of the intestinal epithelium and drosophila melanogaster. Nanotoxicology 12(5):390–406. https://doi.org/10.1080/17435390.2018.1457189
Ammendolia MG, Iosi F, Maranghi F, Tassinari R, Cubadda F, Aureli F et al (2017) Short-term oral exposure to low doses of nano-sized TiO2 and potential modulatory effects on intestinal cells. Food Chem Toxicol 102:63–75. https://doi.org/10.1016/j.fct.2017.01.031
Brun E, Barreau F, Veronesi G, Fayard B, Sorieul S, Chanéac C, …, Carrière M (2014) Titanium dioxide nanoparticle impact and translocation through ex vivo, in vivo and in vitro gut epithelia
Pedata P, Ricci G, Malorni L, Venezia A, Cammarota M, Volpe MG et al (2019) In vitro intestinal epithelium responses to titanium dioxide nanoparticles. Food Res Int 119:634–642. https://doi.org/10.1016/j.foodres.2018.10.041
Gitrowski C, Al-Jubory AR, Handy RD (2014) Uptake of different crystal structures of TiO2 nanoparticles by Caco-2 intestinal cells. Toxicol Lett 226(3):264–276. https://doi.org/10.1016/j.toxlet.2014.02.014
Dekkers S, Wijnhoven SWP, Braakhuis HM, Soeteman-Hernandez LG, Sips AJAM, Tavernaro I et al (2020) Safe-by-design part I: proposal for nanospecific human health safety aspects needed along the innovation process. NanoImpact 18(May):100227. https://doi.org/10.1016/j.impact.2020.100227
Li W, Jia MX, Deng J, Wang JH, Zuberi Z, Yang S et al (2020) MicroRNA response and toxicity of potential pathways in human colon cancer cells exposed to titanium dioxide nanoparticles. Cancers 12(5). https://doi.org/10.3390/cancers12051236
Magdolenova Z, Collins A, Kumar A, Dhawan A, Stone V, Dusinska M (2014) Mechanisms of genotoxicity. A review of in vitro and in vivo studies with engineered nanoparticles. Nanotoxicology 8(3):233–278. https://doi.org/10.3109/17435390.2013.773464
Iavicoli I, Leso V, Fontana L, Bergamaschi A (2011) Toxicological effects of titanium dioxide nanoparticles: A review of in vitro mammalian studies. Eur Rev Med Pharmacol Sci 15. https://doi.org/10.1155/2012/964381
Tada-Oikawa S, Ichihara G, Fukatsu H, Shimanuki Y, Tanaka N, Watanabe E et al (2016) Titanium dioxide particle type and concentration influence the inflammatory response in Caco-2 cells. Int J Mol Sci 17(4). https://doi.org/10.3390/ijms17040576
Gandamalla D, Lingabathula H, Yellu N (2019) Nano titanium exposure induces dose- and size-dependent cytotoxicity on human epithelial lung and colon cells. Drug Chem Toxicol 42(1):24–34. https://doi.org/10.1080/01480545.2018.1452930
Dorier M, Brun E, Veronesi G, Barreau F, Pernet-Gallay K, Desvergne C et al (2015) Impact of anatase and rutile titanium dioxide nanoparticles on uptake carriers and efflux pumps in Caco-2 gut epithelial cells. Nanoscale 7(16):7352–7360. https://doi.org/10.1039/c5nr00505a
De Angelis I, Barone F, Zijno A, Bizzarri L, Russo MT, Pozzi R et al (2013) Comparative study of ZnO and TiO2 nanoparticles: physicochemical characterisation and toxicological effects on human colon carcinoma cells. Nanotoxicology 7(8):1361–1372. https://doi.org/10.3109/17435390.2012.741724
Zijno A, De Angelis I, De Berardis B, Andreoli C, Russo MT, Pietraforte D et al (2015) Different mechanisms are involved in oxidative DNA damage and genotoxicity induction by ZnO and TiO2 nanoparticles in human colon carcinoma cells. Toxicol In Vitro 29(7):1503–1512. https://doi.org/10.1016/j.tiv.2015.06.009
Li N, Ma L, Wang J, Zheng L, Liu J, Duan Y et al (2009) Interaction between Nano-Anatase TiO 2 and liver DNA from mice in vivo. Nanoscale Res Lett 5(1):108–115. https://doi.org/10.1007/s11671-009-9451-2
Shi Z, Niu Y, Wang Q, Shi L, Guo H, Liu Y et al (2015a) Reduction of DNA damage induced by titanium dioxide nanoparticles through Nrf2 in vitro and in vivo. J Hazard Mater 298:310–319. https://doi.org/10.1016/j.jhazmat.2015.05.043
Shi Z, Niu Y, Wang Q, Shi L, Guo H, Liu Y, Zhu Y, Liu S, Liu C, Chen X, Zhang R (2015b) Reduction of DNA damage induced by titanium dioxide nanoparticles through Nrf2 in vitro and in vivo. J Hazard Mater 298:310–319. https://doi.org/10.1016/j.jhazmat.2015.05.043
Dorier M, Béal D, Marie-Desvergne C, Dubosson M, Barreau F, Houdeau E et al (2017) Continuous in vitro exposure of intestinal epithelial cells to E171 food additive causes oxidative stress, inducing oxidation of DNA bases but no endoplasmic reticulum stress. Nanotoxicology 11. https://doi.org/10.1080/17435390.2017.1349203
Dorier M, Tisseyre C, Dussert F, Béal D, Arnal ME, Douki T et al (2019) Toxicological impact of acute exposure to E171 food additive and TiO2 nanoparticles on a co-culture of Caco-2 and HT29-MTX intestinal cells. Mutat Res Genet Toxicol Environ Mutagenesis 845(July 2018):402980. https://doi.org/10.1016/j.mrgentox.2018.11.004
Wang J, Li N, Zheng L, Wang S, Wang Y, Zhao X et al (2011) P38-Nrf-2 signaling pathway of oxidative stress in mice caused by nanoparticulate TiO2. Biol Trace Elem Res 140(2):186–197. https://doi.org/10.1007/s12011-010-8687-0
Gerloff K, Albrecht C, Boots AW, Frster I, Schins RPF (2009) Cytotoxicity and oxidative DNA damage by nanoparticles in human intestinal Caco-2 cells. Nanotoxicology 3(4):355–364. https://doi.org/10.3109/17435390903276933
Abbott Chalew TE, Schwab KJ (2013) Toxicity of commercially available engineered nanoparticles to Caco-2 and SW480 human intestinal epithelial cells. Cell Biol Toxicol 29(2):101–116. https://doi.org/10.1007/s10565-013-9241-6
Jensen DM, Løhr M, Sheykhzade M, Lykkesfeldt J, Wils RS, Loft S, Møller P (2019) Telomere length and genotoxicity in the lung of rats following intragastric exposure to food-grade titanium dioxide and vegetable carbon particles. Mutagenesis 34(2):203–214. https://doi.org/10.1093/mutage/gez003
Jalili P, Gueniche N, Lanceleur R, Burel A, Lavault M-T, Sieg H et al (2018) Investigation of the in vitro genotoxicity of two rutile TiO2 nanomaterials in human intestinal and hepatic cells and evaluation of their interference with toxicity assays. NanoImpact 11:69–81. https://doi.org/10.1016/J.IMPACT.2018.02.004
Song ZM, Chen N, Liu JH, Tang H, Deng X, Xi WS et al (2015) Biological effect of food additive titanium dioxide nanoparticles on intestine: an in vitro study. J Appl Toxicol 35(10):1169–1178. https://doi.org/10.1002/jat.3171
Charles S, Jomini S, Fessard V, Bigorgne-Vizade E, Rousselle C, Michel C (2018) Assessment of the in vitro genotoxicity of TiO2 nanoparticles in a regulatory context. Nanotoxicology 12(4):357–374. https://doi.org/10.1080/17435390.2018.1451567
IPCS (2019) Principles and methods to assess the risk of immunotoxicity associated with exposure to nanomaterials. Environmental Health Criteria: n. 244. Geneva
Trouiller B, Reliene R, Westbrook A, Solaimani P, Schiestl RH (2009) Titanium dioxide nanoparticles induce DNA damage and genetic instability in vivo in mice. Cancer Res 69(22):8784–8789. https://doi.org/10.1158/0008-5472.CAN-09-2496
Chen Z, Han S, Zhou D, Zhou S, Jia G (2019) Effects of oral exposure to titanium dioxide nanoparticles on gut microbiota and gut-associated metabolism: in vivo. Nanoscale 11(46):22398–22412. https://doi.org/10.1039/c9nr07580a
Hashem MM, Abo-EL-Sooud K, Abd-Elhakim YM, Badr YAH, El-Metwally AE, Bahy-El-Dien A (2020) The long-term oral exposure to titanium dioxide impaired immune functions and triggered cytotoxic and genotoxic impacts in rats. J Trace Elem Med Biol 60(February):126473. https://doi.org/10.1016/j.jtemb.2020.126473
Dhupal M, Oh JM, Tripathy DR, Kim SK, Koh SB, Park KS (2018) Immunotoxicity of titanium dioxide nanoparticles via simultaneous induction of apoptosis and multiple toll-like receptors signaling through ROS-dependent SAPK/JNK and p38 MAPK activation. Int J Nanomedicine 13:6735–6750. https://doi.org/10.2147/IJN.S176087
Cui Y, Liu H, Ze Y, Zhang Z, Hu Y, Cheng Z, Cheng J, Hu R, Gao G, Wang L, Tang M, Hong F (2015) Corrigendum: gene expression in liver injury caused by long-term exposure to titanium dioxide nanoparticles in mice. Toxicol Sci 146(1):202. https://doi.org/10.1093/toxsci/kfv097. Erratum for: Toxicol Sci. 2012 Jul;128(1):171-85. PMID: 26101236
Hong F, Ji J, Ze X, Zhou Y, Ze Y (2020) Liver inflammation and fibrosis induced by long-term exposure to Nano titanium dioxide (TiO2) nanoparticles in mice and its molecular mechanism. J Biomed Nanotechnol 16(5):616–625. https://doi.org/10.1166/jbn.2020.2921
Kolling J, Tigges J, Hellack B, Albrecht C, Schins RPF (2020) Evaluation of the nlrp3 inflammasome activating effects of a large panel of tio2 nanomaterials in macrophages. Nano 10(9):1–18. https://doi.org/10.3390/nano10091876
Smolkova B, El Yamani N, Collins AR, Gutleb AC, Dusinska M (2015) Nanoparticles in food. Epigenetic changes induced by nanomaterials and possible impact on health. Food Chem Toxicol 77:64–73. https://doi.org/10.1016/j.fct.2014.12.015
Stoccoro A, Karlsson HL, Coppedè F, Migliore L (2013) Epigenetic effects of nano-sized materials. Toxicology 313. https://doi.org/10.1016/j.tox.2012.12.002
Ghosh M, Öner D, Duca RC, Cokic SM, Seys S, Kerkhofs S et al (2017) Cyto-genotoxic and DNA methylation changes induced by different crystal phases of TiO 2 -np in bronchial epithelial (16-HBE) cells. Mutat Res 796:1–12. https://doi.org/10.1016/j.mrfmmm.2017.01.003
Dudefoi W, Moniz K, Allen-Vercoe E, Ropers MH, Walker VK (2017) Impact of food grade and nano-TiO2 particles on a human intestinal community. Food Chem Toxicol 106(Pt A):242–249. https://doi.org/10.1016/j.fct.2017.05.050
Radziwill-Bienkowska JM, Talbot P, Kamphuis JBJ, Robert V, Cartier C, Fourquaux I, Lentzen E, Audinot JN, Jamme F, Réfrégiers M, Bardowski JK, Langella P, Kowalczyk M, Houdeau E, Thomas M, Mercier-Bonin M (2018) Toxicity of food-grade TiO2 to commensal intestinal and transient food-borne bacteria: new insights using Nano-SIMS and synchrotron UV fluorescence imaging. Front Microbiol 9:794. https://doi.org/10.3389/fmicb.2018.00794
Pinget G, Tan J, Janac B, Kaakoush NO, Angelatos AS, O’Sullivan J et al (2019) Impact of the food additive titanium dioxide (e171) on gut microbiota-host interaction. Frontiers. Nutrition 6(May). https://doi.org/10.3389/fnut.2019.00057
Zhang S, Jiang X, Cheng S, Fan J, Qin X, Wang T et al (2020) Titanium dioxide nanoparticles via oral exposure leads to adverse disturbance of gut microecology and locomotor activity in adult mice. Arch Toxicol 94(4):1173–1190. https://doi.org/10.1007/s00204-020-02698-2
Proquin H, Jetten MJ, Jonkhout MCM, Garduño-Balderas LG, Briedé JJ, de Kok TM, van Loveren H, Chirino YI (2018) Transcriptomics analysis reveals new insights in E171-induced molecular alterations in a mouse model of colon cancer. Sci Rep 8(1):9738. https://doi.org/10.1038/s41598-018-28063-z
Urrutia-Ortega IM, Garduño-Balderas LG, Delgado-Buenrostro NL, Freyre-Fonseca V, Flores-Flores JO, González-Robles A et al (2016) Food-grade titanium dioxide exposure exacerbates tumor formation in colitis associated cancer model. Food Chem Toxicol 93:20–31. https://doi.org/10.1016/j.fct.2016.04.014
OECD (2016) Users’ handbook supplement to the guidance document for developing and assessing adverse outcome pathways. ENV/JM/MONO(2016) 12. Paris. https://doi.org/10.1787/5jlv1m9d1g32-en
Brand W, Peters RJB, Braakhuis HM, Maślankiewicz L, Oomen AG (2020) Possible effects of titanium dioxide particles on human liver, intestinal tissue, spleen and kidney after oral exposure. Nanotoxicology 14(7):985–1007. https://doi.org/10.1080/17435390.2020.1778809
Louro H, Bettencourt A, Gonçalves LM, Almeida AJ, Silva MJ (2015) Nanotechnology applications for tissue engineering. In: Thomas S, Grohens Y, Ninan N (eds) Nanotechnology applications for tissue engineering. Elsevier, pp 263–287. https://doi.org/10.1016/B978-0-323-32889-0.00009-1
Shah SU (2012) Importance of genotoxicity & S2A guidelines for genotoxicity testing for pharmaceuticals. IOSR J Pharm Biol Sci 1(2):43–54. https://doi.org/10.1103/PhysRevB.84.064423
Nohmi T (2018) Thresholds of genotoxic and non-genotoxic carcinogens. Toxicol Res 34(4):281–290. https://doi.org/10.5487/TR.2018.34.4.281
Singh N, Manshian B, Jenkins GJS, Griffiths SM, Williams PM, Maffeis TGG et al (2009) NanoGenotoxicology: the DNA damaging potential of engineered nanomaterials. Biomaterials 30(23–24):3891–3914. https://doi.org/10.1016/j.biomaterials.2009.04.009
Food and Drug Administration (FDA) (2012) S2(R1) genotoxicity testing and data interpretation for pharmaceuticals intended for human use. https://doi.org/10.1246/bcsj.79.1054
OECD (2017) Overview of the set of OECD Genetic Toxicology Test Guidelines and updates performed in 2014–2015. Series on Testing & Assessment, No. 238 (2nd edn), ENV/JM/MONO(2016)33/REV1. Retrieved from https://www.oecd.org/officialdocuments/publicdisplaydocumentpdf/?cote=ENV-JM-MONO(2016)33/rev1&doclanguage=en
ICH (1995) Guideline on the need for Carcinogenity Studies on Pharmaceuticals (S1A)
Dusinska M, Mariussen E, Pran ER, Hudecova AM, Elje E, Kazimirova A et al (2019) In vitro approaches for assessing the genotoxicity of nanomaterials. In: Zhang Q (ed) Nanotoxicity: methods and protocols, methods in molecular biology. Springer, pp 83–122
Adan A, Kiraz Y, Baran Y (2016) Cell proliferation and cytotoxicity assays. Curr Biotechnol Pharm 17(14):1873–4316. https://doi.org/10.2174/13892010176661608081605
van Meerloo J, Kaspers GJL, Cloos J (2011) Cell sensitivity assays: the MTT assay. In: Cree IA (ed) Cancer cell culture. Methods in molecular biology (methods and protocols), vol 731. Humana Press, pp 237–246. https://doi.org/10.1007/978-1-61779-080-5
Landsiedel R, Ma-Hock L, Kroll A, Hahn D, Schnekenburger J, Wiench K, Wohlleben W (2010) Testing metal-oxide nanomaterials for human safety. Adv Mater 22(24):2601–2627. https://doi.org/10.1002/adma.200902658
McCracken C, Dutta PK, Waldman WJ (2016) Critical assessment of toxicological effects of ingested nanoparticles. Environ Sci Nano 3(2):256–282. https://doi.org/10.31729/jnma.1240
Laloux L, Polet M, Schneider Y-J (2017) Interaction between ingested-engineered nanomaterials and the gastrointestinal tract: in vitro toxicology aspects. In: Axelos MAV, Vande Voorde M (eds) Nanotechnology in agriculture and food science. Wiley, pp 311–332. https://doi.org/10.1002/9783527697724.ch18
Braakhuis HM, Kloet SK, Kezic S, Kuper F, Park MVDZ, Bellmann S, Bouwmeester H (2015) Progress and future of in vitro models to study translocation of nanoparticles. Arch Toxicol 89(9):1469–1495. https://doi.org/10.1007/s00204-015-1518-5
Hilgendorf C, Spahn-Langguth H, Regårdh CG, Lipka E, Amidon GL, Langguth P (2000) Caco-2 versus Caco-2/HT29-MTX co-cultured cell lines: Permeabilities via diffusion, inside- and outside-directed carrier-mediated transport. J Pharm Sci 89(1):63–75. https://doi.org/10.1002/(SICI)1520-6017(200001)89:1<63::AID-JPS7>3.0.CO;2-6
Natoli M, Leoni BD, D’Agnano I, Zucco F, Felsani A (2012) Good Caco-2 cell culture practices. Toxicol In Vitro 26. https://doi.org/10.1016/j.tiv.2012.03.009
Lesuffleur T, Barbat A, Dussaulx E, Zweibaum A (1990) Growth adaptation to methotrexate of HT-29 human colon carcinoma cells is associated with their ability to differentiate into columnar absorptive and mucus-secreting cells. Cancer Res 50(19):6334–6343
Sohal IS, O’Fallon KS, Gaines P, Demokritou P, Bello D (2018b) Ingested engineered nanomaterials: state of science in nanotoxicity testing and future research needs. Part Fibre Toxicol 15(1):29. https://doi.org/10.1186/s12989-018-0265-1
Hur SJ, Lim BO, Decker EA, McClements DJ (2011) In vitro human digestion models for food applications. Food Chem 125(1):1–12. https://doi.org/10.1016/j.foodchem.2010.08.036
Gerloff K, Fenoglio I, Carella E, Kolling J, Albrecht C, Boots AW et al (2012) Distinctive toxicity of TiO 2 rutile/anatase mixed phase nanoparticles on Caco-2 cells. Chem Res Toxicol 25. https://doi.org/10.1021/tx200334k
McCracken C, Zane A, Knight DA, Dutta PK, Waldman WJ (2013) Minimal intestinal epithelial cell toxicity in response to short- and long-term food-relevant inorganic nanoparticle exposure. Chem Res Toxicol 26(10):1514–1525. https://doi.org/10.1021/tx400231u
Schneider T, Westermann M, Glei M (2017) In vitro uptake and toxicity studies of metal nanoparticles and metal oxide nanoparticles in human HT29 cells. Arch Toxicol 91(11):3517–3527. https://doi.org/10.1007/s00204-017-1976-z
Kukia NR, Rasmi Y, Abbasi A, Koshoridze N, Shirpoor A, Burjanadze G, Saboory E (2018) Bio-effects of TiO2 nanoparticles on human colorectal cancer and umbilical vein endothelial cell lines. Asian Pacific J Cancer Prevent 19(10):2821–2829. https://doi.org/10.22034/APJCP.2018.19.10.2821
Cao X, Deloid GM, Bitounis D, La Torre-Roche RD, White C, Zhang Z et al (2019) Co-exposure to the food additives SiO2 (E551) or TiO2 (E171) and the pesticide boscalid increases cytotoxicity and bioavailability of the pesticide in a tri-culture small intestinal epithelium model: potential health implications. Environ Sci Nano 6(9):2786–2800. https://doi.org/10.1039/c9en00676a
Cao X, Zhang T, DeLoid GM, Gaffrey MJ, Weitz KK, Thrall BD et al (2020) Evaluation of the cytotoxic and cellular proteome impacts of food-grade TiO2 (E171) using simulated gastrointestinal digestions and a tri-culture small intestinal epithelial model. NanoImpact 17(August 2019). https://doi.org/10.1016/j.impact.2019.100202
Barrasa JI, Olmo N, Lizarbe MA, Turnay J (2013) Bile acids in the colon, from healthy to cytotoxic molecules. Toxicol In Vitro 27(2):964–977. https://doi.org/10.1016/j.tiv.2012.12.020
Sycheva LP, Zhurkov VS, Iurchenko VV, Daugel-Dauge NO, Kovalenko MA, Krivtsova EK, Durnev AD (2011) Investigation of genotoxic and cytotoxic effects of micro- and nanosized titanium dioxide in six organs of mice in vivo. Mutat Res 726(1):8–14. https://doi.org/10.1016/j.mrgentox.2011.07.010
Carmona ER, Escobar B, Vales G, Marcos R (2015) Genotoxic testing of titanium dioxide anatase nanoparticles using the wing-spot test and the comet assay in Drosophila. Mutat Res Genet Toxicol Environ Mutagenesis 778:12–21. https://doi.org/10.1016/j.mrgentox.2014.12.004
NanoGenoTox Joint Action (2013) NANOGENOTOX final report. Facilitating the safety evaluation of manufactured nanomaterials by characterising their potential genotoxic hazard. Retrieved from http://www.nanogenotox.eu/index.php?option=com_content&view=article&id=136&Itemid=158
Vila L, García-Rodríguez A, Marcos R, Hernández A (2018b) Titanium dioxide nanoparticles translocate through differentiated Caco-2 cell monolayers, without disrupting the barrier functionality or inducing genotoxic damage. J Appl Toxicol 38(9):1195–1205. https://doi.org/10.1002/jat.3630
Vila L, García-Rodríguez A, Cortés C, Marcos R, Hernández A (2018a) Assessing the effects of silver nanoparticles on monolayers of differentiated Caco-2 cells, as a model of intestinal barrier. Food Chem Toxicol 116. https://doi.org/10.1016/j.fct.2018.04.008
Du X, Gao S, Hong L, Zheng X, Zhou Q, Wu J (2019) Genotoxicity evaluation of titanium dioxide nanoparticles using the mouse lymphoma assay and the Ames test. Mutat Res Genet Toxicol Environ Mutagenesis 838(November 2018):22–27. https://doi.org/10.1016/j.mrgentox.2018.11.015
Wang JJ, Sanderson BJS, Wang H (2007a) Cyto- and genotoxicity of ultrafine TiO2 particles in cultured human lymphoblastoid cells. Mutat Res 628(2):99–106. https://doi.org/10.1016/j.mrgentox.2006.12.003
Murugadoss S, Brassinne F, Sebaihi N, Petry J, Cokic SM, Van Landuyt KL, Godderis L, Mast J, Lison D, Hoet PH, van den Brule S (2020) Agglomeration of titanium dioxide nanoparticles increases toxicological responses in vitro and in vivo. Part Fibre Toxicol 17(1):10. https://doi.org/10.1186/s12989-020-00341-7
Grissa I, Elghoul J, Ezzi L, Chakroun S, Kerkeni E, Hassine M, El Mir L, Mehdi M, Ben CH, Haouas Z (2015) Anemia and genotoxicity induced by sub-chronic intragastric treatment of rats with titanium dioxide nanoparticles. Mutat Res Genet Toxicol Environ Mutagen 794:25–31. https://doi.org/10.1016/j.mrgentox.2015.09.005
Shukla RK, Kumar A, Vallabani NVS, Pandey AK, Dhawan A (2014) Titanium dioxide nanoparticle-induced oxidative stress triggers DNA damage and hepatic injury in mice. Nanomedicine 9(9):1423–1434. https://doi.org/10.2217/nnm.13.100
Chakrabarti S, Goyary D, Karmakar S, Chattopadhyay P (2019) Exploration of cytotoxic and genotoxic endpoints following sub-chronic oral exposure to titanium dioxide nanoparticles. Toxicol Ind Health 35(9):577–592. https://doi.org/10.1177/0748233719879611
Chen Z, Wang Y, Ba T, Li Y, Pu J, Chen T, Song Y, Gu Y, Qian Q, Yang J, Jia G (2014) Genotoxic evaluation of titanium dioxide nanoparticles in vivo and in vitro. Toxicol Lett 226(3):314–319. https://doi.org/10.1016/j.toxlet.2014.02.020
Martins ADC Jr, Azevedo LF, de Souza Rocha CC, Carneiro MFH, Venancio VP, de Almeida MR, Antunes LMG, de Carvalho Hott R, Rodrigues JL, Ogunjimi AT, Adeyemi JA, Barbosa F Jr (2017) Evaluation of distribution, redox parameters, and genotoxicity in Wistar rats co-exposed to silver and titanium dioxide nanoparticles. J Toxicol Environ Health A 80(19–21):1156–1165. https://doi.org/10.1080/15287394.2017.1357376
Manivannan J, Banerjee R, Mukherjee A (2019) Genotoxicity analysis of rutile titanium dioxide nanoparticles in mice after 28 days of repeated oral administration. Nucleus 63(1):17–24. https://doi.org/10.1007/s13237-019-00277-0
Blevins LK, Crawford RB, Bach A, Rizzo MD, Zhou J, Henriquez JE, Khan DMIO, Sermet S, Arnold LL, Pennington KL, Souza NP, Cohen SM, Kaminski NE (2019) Evaluation of immunologic and intestinal effects in rats administered an E 171-containing diet, a food grade titanium dioxide (TiO2). Food Chem Toxicol 133:110793. https://doi.org/10.1016/j.fct.2019.110793
Acknowledgements
This work was funded by national funds through the FCT - Foundation for Science and Technology, I.P., under the project INGESTnano- PTDC/SAU-PUB/29481/2017. Research co-funded by European Union Seventh Framework Programme (FP7/ 2007e2013) under the project NANoREG (A common European approach to the regulatory testing of nanomaterials), grant agreement 310584 and by UIDB/00009/2020; UIDP/00009/2020 (Centre for Toxicogenomics and Human Health – ToxOmics, Foundation for Science and Technology). NV holds a FCT PhD Scholarship grant (2020.07168.BD).
The authors thank all the support from the colleagues Paula Alvito, Carla Martins and Ricardo Assunção (Food Safety Department, INSA, Lisbon, Portugal) and from Ana F. Bettencourt and Lídia Gonçalves (FarmID, Lisbon University, Portugal), as well from all INGESTnano team members.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2022 The Author(s)
About this chapter
Cite this chapter
Vieira, A., Gramacho, A., Rolo, D., Vital, N., Silva, M.J., Louro, H. (2022). Cellular and Molecular Mechanisms of Toxicity of Ingested Titanium Dioxide Nanomaterials. In: Louro, H., Silva, M.J. (eds) Nanotoxicology in Safety Assessment of Nanomaterials. Advances in Experimental Medicine and Biology, vol 1357. Springer, Cham. https://doi.org/10.1007/978-3-030-88071-2_10
Download citation
DOI: https://doi.org/10.1007/978-3-030-88071-2_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-88070-5
Online ISBN: 978-3-030-88071-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)