Abstract
Pelvic organ prolapse and urinary incontinence are common disorders among women and often coexist. This chapter reviews the epidemiology of prolapse, presents a summary of the data and theories behind a shared mechanism of disease between prolapse and urinary incontinence, and the impact of prolapse treatment on urinary incontinence symptoms.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Haylen BT, Maher CF, Barber MD, Camargo S, Dandolu V, Digesu A, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic organ prolapse (POP). Int Urogynecol J. 2016;27(4):655–84. https://doi.org/10.1007/s00192-016-3003-y.
Rogers RG. Female pelvic medicine and reconstructive surgery: clinical practice and surgical atlas. 1st ed. New York: McGraw-Hill; 2013.
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175(1):10–7.
Baden WF, Walker T. Surgical repair of vaginal defects. Philadelphia: Lippincott; 1992.
Nygaard I, Barber MD, Burgio KL, Kenton K, Meikle S, Schaffer J, et al. Prevalence of symptomatic pelvic floor disorders in US women. JAMA. 2008;300(11):1311–6. https://doi.org/10.1001/jama.300.11.1311.
Barber MD, Maher C. Epidemiology and outcome assessment of pelvic organ prolapse. Int Urogynecol J. 2013;24(11):1783–90. https://doi.org/10.1007/s00192-013-2169-9.
Swift SE. The distribution of pelvic organ support in a population of female subjects seen for routine gynecologic health care. Am J Obstet Gynecol. 2000;183(2):277–85. https://doi.org/10.1067/mob.2000.107583.
Hendrix SL, Clark A, Nygaard I, Aragaki A, Barnabei V, McTiernan A. Pelvic organ prolapse in the Women’s Health Initiative: gravity and gravidity. Am J Obstet Gynecol. 2002;186(6):1160–6.
Dieter AA, Wilkins MF, Wu JM. Epidemiological trends and future care needs for pelvic floor disorders. Curr Opin Obstet Gynecol. 2015;27(5):380–4. https://doi.org/10.1097/GCO.0000000000000200.
Delancey JO, Kane Low L, Miller JM, Patel DA, Tumbarello JA. Graphic integration of causal factors of pelvic floor disorders: an integrated life span model. Am J Obstet Gynecol. 2008;199(6):610, e1-5. https://doi.org/10.1016/j.ajog.2008.04.001.
Wu JM, Vaughan CP, Goode PS, Redden DT, Burgio KL, Richter HE, et al. Prevalence and trends of symptomatic pelvic floor disorders in U.S. women. Obstet Gynecol. 2014;123(1):141–8. https://doi.org/10.1097/AOG.0000000000000057.
Akervall S, Al-Mukhtar Othman J, Molin M, Gyhagen M. Symptomatic pelvic organ prolapse in middle-aged women: a national matched cohort study on the influence of childbirth. Am J Obstet Gynecol. 2020;222(4):356, e1-e14. https://doi.org/10.1016/j.ajog.2019.10.007.
Chiaffarino F, Chatenoud L, Dindelli M, Meschia M, Buonaguidi A, Amicarelli F, et al. Reproductive factors, family history, occupation and risk of urogenital prolapse. Eur J Obstet Gynecol Reprod Biol. 1999;82(1):63–7. https://doi.org/10.1016/s0301-2115(98)00175-4.
Handa VL, Blomquist JL, Roem J, Munoz A. Longitudinal study of quantitative changes in pelvic organ support among parous women. Am J Obstet Gynecol. 2018;218(3):320, e1-e7. https://doi.org/10.1016/j.ajog.2017.12.214.
Lukacz ES, Lawrence JM, Contreras R, Nager CW, Luber KM. Parity, mode of delivery, and pelvic floor disorders. Obstet Gynecol. 2006;107(6):1253–60. https://doi.org/10.1097/01.AOG.0000218096.54169.34.
Moalli PA, Jones Ivy S, Meyn LA, Zyczynski HM. Risk factors associated with pelvic floor disorders in women undergoing surgical repair. Obstet Gynecol. 2003;101(5 Pt 1):869–74. https://doi.org/10.1016/s0029-7844(03)00078-4.
Kearney R, Fitzpatrick M, Brennan S, Behan M, Miller J, Keane D, et al. Levator ani injury in primiparous women with forceps delivery for fetal distress, forceps for second stage arrest, and spontaneous delivery. Int J Gynaecol Obstet. 2010;111(1):19–22. https://doi.org/10.1016/j.ijgo.2010.05.019.
DeLancey JO, Morgan DM, Fenner DE, Kearney R, Guire K, Miller JM, et al. Comparison of levator ani muscle defects and function in women with and without pelvic organ prolapse. Obstet Gynecol. 2007;109(2 Pt 1):295–302. https://doi.org/10.1097/01.AOG.0000250901.57095.ba.
Dietz HP, Simpson JM. Levator trauma is associated with pelvic organ prolapse. BJOG. 2008;115(8):979–84. https://doi.org/10.1111/j.1471-0528.2008.01751.x.
Lammers K, Lince SL, Spath MA, van Kempen LC, Hendriks JC, Vierhout ME, et al. Pelvic organ prolapse and collagen-associated disorders. Int Urogynecol J. 2012;23(3):313–9. https://doi.org/10.1007/s00192-011-1532-y.
Weidner AC, Jamison MG, Branham V, South MM, Borawski KM, Romero AA. Neuropathic injury to the levator ani occurs in 1 in 4 primiparous women. Am J Obstet Gynecol. 2006;195(6):1851–6. https://doi.org/10.1016/j.ajog.2006.06.062.
Lien KC, Morgan DM, Delancey JO, Ashton-Miller JA. Pudendal nerve stretch during vaginal birth: a 3D computer simulation. Am J Obstet Gynecol. 2005;192(5):1669–76. https://doi.org/10.1016/j.ajog.2005.01.032.
Blomquist JL, Munoz A, Carroll M, Handa VL. Association of delivery mode with pelvic floor disorders after childbirth. JAMA. 2018;320(23):2438–47. https://doi.org/10.1001/jama.2018.18315.
Allen-Brady K, Cannon-Albright L, Farnham JM, Teerlink C, Vierhout ME, van Kempen LCL, et al. Identification of six loci associated with pelvic organ prolapse using genome-wide association analysis. Obstet Gynecol. 2011;118(6):1345–53. https://doi.org/10.1097/AOG.0b013e318236f4b5.
Carley ME, Schaffer J. Urinary incontinence and pelvic organ prolapse in women with Marfan or Ehlers Danlos syndrome. Am J Obstet Gynecol. 2000;182(5):1021–3. https://doi.org/10.1067/mob.2000.105410.
Ward RM, Velez Edwards DR, Edwards T, Giri A, Jerome RN, Wu JM. Genetic epidemiology of pelvic organ prolapse: a systematic review. Am J Obstet Gynecol. 2014;211(4):326–35. https://doi.org/10.1016/j.ajog.2014.04.006.
Cartwright R, Kirby AC, Tikkinen KA, Mangera A, Thiagamoorthy G, Rajan P, et al. Systematic review and metaanalysis of genetic association studies of urinary symptoms and prolapse in women. Am J Obstet Gynecol. 2015;212(2):199, e1-24. https://doi.org/10.1016/j.ajog.2014.08.005.
Snooks SJ, Barnes PR, Swash M, Henry MM. Damage to the innervation of the pelvic floor musculature in chronic constipation. Gastroenterology. 1985;89(5):977–81. https://doi.org/10.1016/0016-5085(85)90196-9.
Bai SW, Jeon MJ, Kim JY, Chung KA, Kim SK, Park KH. Relationship between stress urinary incontinence and pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2002;13(4):256–60.; discussion 60. https://doi.org/10.1007/s001920200053.
Muniz KS, Pilkinton M, Winkler HA, Shalom DF. Prevalence of stress urinary incontinence and intrinsic sphincter deficiency in patients with stage IV pelvic organ prolapse. J Obstet Gynaecol Res. 2020;47(2):640–4. https://doi.org/10.1111/jog.14574.
Hoyte LPJ, Damaser M. Biomechanics of the female pelvic floor. London/San Diego: Academic Press is an imprint of Elsevier; 2016.
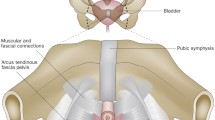
DeLancey JO. Structural support of the urethra as it relates to stress urinary incontinence: the hammock hypothesis. Am J Obstet Gynecol. 1994;170(6):1713–20.; discussion 20-3. https://doi.org/10.1016/s0002-9378(94)70346-9.
Burrows LJ, Meyn LA, Walters MD, Weber AM. Pelvic symptoms in women with pelvic organ prolapse. Obstet Gynecol. 2004;104(5 Pt 1):982–8. https://doi.org/10.1097/01.AOG.0000142708.61298.be.
DeLancey JO, Trowbridge ER, Miller JM, Morgan DM, Guire K, Fenner DE, et al. Stress urinary incontinence: relative importance of urethral support and urethral closure pressure. J Urol. 2008;179(6):2286–90.; discussion 90. https://doi.org/10.1016/j.juro.2008.01.098.
Bai SW, Cho JM, Kwon HS, Park JH, Shin JS, Kim SK, et al. The relationship between maximal urethral closure pressure and functional urethral length in anterior vaginal wall prolapse patients according to stage and age. Yonsei Med J. 2005;46(3):408–13. https://doi.org/10.3349/ymj.2005.46.3.408.
Chang HW, Ng SC, Chen GD. Correlations between severity of anterior vaginal wall prolapse and parameters of urethral pressure profile. Low Urin Tract Symptoms. 2020;13(2):238–43. https://doi.org/10.1111/luts.12357.
Trowbridge ER, Wei JT, Fenner DE, Ashton-Miller JA, Delancey JO. Effects of aging on lower urinary tract and pelvic floor function in nulliparous women. Obstet Gynecol. 2007;109(3):715–20. https://doi.org/10.1097/01.AOG.0000257074.98122.69.
Cameron AP. Systematic review of lower urinary tract symptoms occurring with pelvic organ prolapse. Arab J Urol. 2019;17(1):23–9. https://doi.org/10.1080/2090598X.2019.1589929.
Bradley CS, Nygaard IE. Vaginal wall descensus and pelvic floor symptoms in older women. Obstet Gynecol. 2005;106(4):759–66. https://doi.org/10.1097/01.AOG.0000180183.03897.72.
Fritel X, Varnoux N, Zins M, Breart G, Ringa V. Symptomatic pelvic organ prolapse at midlife, quality of life, and risk factors. Obstet Gynecol. 2009;113(3):609–16. https://doi.org/10.1097/AOG.0b013e3181985312.
Tegerstedt G, Maehle-Schmidt M, Nyren O, Hammarstrom M. Prevalence of symptomatic pelvic organ prolapse in a Swedish population. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16(6):497–503. https://doi.org/10.1007/s00192-005-1326-1.
de Boer TA, Salvatore S, Cardozo L, Chapple C, Kelleher C, van Kerrebroeck P, et al. Pelvic organ prolapse and overactive bladder. Neurourol Urodyn. 2010;29(1):30–9. https://doi.org/10.1002/nau.20858.
Birder LA, de Groat WC. Mechanisms of disease: involvement of the urothelium in bladder dysfunction. Nat Clin Pract Urol. 2007;4(1):46–54. https://doi.org/10.1038/ncpuro0672.
Ferguson DR, Kennedy I, Burton TJ. ATP is released from rabbit urinary bladder epithelial cells by hydrostatic pressure changes--a possible sensory mechanism? J Physiol. 1997;505(Pt 2):503–11. https://doi.org/10.1111/j.1469-7793.1997.503bb.x.
Keay SK, Birder LA, Chai TC. Evidence for bladder urothelial pathophysiology in functional bladder disorders. Biomed Res Int. 2014;2014:865463. https://doi.org/10.1155/2014/865463.
Glazener CM, Cooper K, Mashayekhi A. Anterior vaginal repair for urinary incontinence in women. Cochrane Database Syst Rev. 2017;7:CD001755. https://doi.org/10.1002/14651858.CD001755.pub2.
Handa VL, Jones M. Do pessaries prevent the progression of pelvic organ prolapse? Int Urogynecol J Pelvic Floor Dysfunct. 2002;13(6):349–51.; discussion 52. https://doi.org/10.1007/s001920200078.
Clemons JL, Aguilar VC, Tillinghast TA, Jackson ND, Myers DL. Patient satisfaction and changes in prolapse and urinary symptoms in women who were fitted successfully with a pessary for pelvic organ prolapse. Am J Obstet Gynecol. 2004;190(4):1025–9. https://doi.org/10.1016/j.ajog.2003.10.711.
Fernando RJ, Thakar R, Sultan AH, Shah SM, Jones PW. Effect of vaginal pessaries on symptoms associated with pelvic organ prolapse. Obstet Gynecol. 2006;108(1):93–9. https://doi.org/10.1097/01.AOG.0000222903.38684.cc.
Romanzi LJ, Chaikin DC, Blaivas JG. The effect of genital prolapse on voiding. J Urol. 1999;161(2):581–6.
Ding J, Chen C, Song XC, Zhang L, Deng M, Zhu L. Changes in prolapse and urinary symptoms after successful fitting of a ring pessary with support in women with advanced pelvic organ prolapse: a prospective study. Urology. 2016;87:70–5. https://doi.org/10.1016/j.urology.2015.07.025.
American Urogynecologic Society Guidelines Statements Committee, Carberry CL, Tulikangas PK, Ridgeway BM, Collins SA, Adam RA. American urogynecologic society best practice statement: evaluation and counseling of patients with pelvic organ prolapse. Female Pelvic Med Reconstr Surg. 2017;23(5):281–7. https://doi.org/10.1097/SPV.0000000000000424.
Abrams P, Cardozo L, Wagg A, Wein A, editors. Incontinence. 6th ed. Bristol: International Continence Society; 2017.
Foster RT Sr, Barber MD, Parasio MF, Walters MD, Weidner AC, Amundsen CL. A prospective assessment of overactive bladder symptoms in a cohort of elderly women who underwent transvaginal surgery for advanced pelvic organ prolapse. Am J Obstet Gynecol. 2007;197(1):82, e1-4. https://doi.org/10.1016/j.ajog.2007.02.049.
Maher C, Feiner B, Baessler K, Schmid C. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2013;(4):CD004014. https://doi.org/10.1002/14651858.CD004014.pub5.
Colombo M, Vitobello D, Proietti F, Milani R. Randomised comparison of Burch colposuspension versus anterior colporrhaphy in women with stress urinary incontinence and anterior vaginal wall prolapse. BJOG. 2000;107(4):544–51. https://doi.org/10.1111/j.1471-0528.2000.tb13276.x.
Borstad E, Abdelnoor M, Staff AC, Kulseng-Hanssen S. Surgical strategies for women with pelvic organ prolapse and urinary stress incontinence. Int Urogynecol J. 2010;21(2):179–86. https://doi.org/10.1007/s00192-009-1007-6.
Brubaker L, Cundiff GW, Fine P, Nygaard I, Richter HE, Visco AG, et al. Abdominal sacrocolpopexy with Burch colposuspension to reduce urinary stress incontinence. N Engl J Med. 2006;354(15):1557–66. https://doi.org/10.1056/NEJMoa054208.
Liang CC, Chang YL, Chang SD, Lo TS, Soong YK. Pessary test to predict postoperative urinary incontinence in women undergoing hysterectomy for prolapse. Obstet Gynecol. 2004;104(4):795–800. https://doi.org/10.1097/01.AOG.0000140689.90131.01.
Visco AG, Brubaker L, Nygaard I, Richter HE, Cundiff G, Fine P, et al. The role of preoperative urodynamic testing in stress-continent women undergoing sacrocolpopexy: the Colpopexy and Urinary Reduction Efforts (CARE) randomized surgical trial. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(5):607–14. https://doi.org/10.1007/s00192-007-0498-2.
Wei JT, Nygaard I, Richter HE, Nager CW, Barber MD, Kenton K, et al. A midurethral sling to reduce incontinence after vaginal prolapse repair. N Engl J Med. 2012;366(25):2358–67. https://doi.org/10.1056/NEJMoa1111967.
Ellstrom Engh AM, Ekeryd A, Magnusson A, Olsson I, Otterlind L, Tobiasson G. Can de novo stress incontinence after anterior wall repair be predicted? Acta Obstet Gynecol Scand. 2011;90(5):488–93. https://doi.org/10.1111/j.1600-0412.2011.01087.x.
Nager CW, Brubaker L, Litman HJ, Zyczynski HM, Varner RE, Amundsen C, et al. A randomized trial of urodynamic testing before stress-incontinence surgery. N Engl J Med. 2012;366(21):1987–97. https://doi.org/10.1056/NEJMoa1113595.
Hullfish KL, Bovbjerg VE, Steers WD. Patient-centered goals for pelvic floor dysfunction surgery: long-term follow-up. Am J Obstet Gynecol. 2004;191(1):201–5. https://doi.org/10.1016/j.ajog.2004.03.086.
Jelovsek JE. Predicting urinary incontinence after surgery for pelvic organ prolapse. Curr Opin Obstet Gynecol. 2016;28(5):399–406. https://doi.org/10.1097/GCO.0000000000000308.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Horner, W., Swenson, C.W. (2022). Prolapse as a Contributing Factor to Stress and Urgency Urinary Incontinence. In: Cameron, A.P. (eds) Female Urinary Incontinence. Springer, Cham. https://doi.org/10.1007/978-3-030-84352-6_20
Download citation
DOI: https://doi.org/10.1007/978-3-030-84352-6_20
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-84351-9
Online ISBN: 978-3-030-84352-6
eBook Packages: MedicineMedicine (R0)