Abstract
Inflammatory bowel disease (IBD) is an autoimmune disorder affecting the gastrointestinal tract. It is generally categorized into Crohn’s disease (CD) and ulcerative colitis (UC). These disease processes are more recently thought of as a disease continuum, with distinct features as well as substantial overlap (Cleynen, et al. Lancet 387(10014):156–167, 2016). There is no single test that can definitely establish the diagnosis of IBD or reliably distinguish between the two disease states of CD and UC. Additionally, IBD can present atypically or overlap with other disease processes. As a result of the complexity involved in making this diagnosis, there still remain substantial delays from the onset of symptoms to the diagnosis. A recent US study found an average delay of 9.5 months from symptoms to diagnosis for Crohn’s disease and 3.1 months for ulcerative colitis (Nguyen, et al. Inflamm Bowel Dis 23(10):1825–1831, 2017). This additional time to diagnosis for Crohn’s is borne out in several other international studies (Novacek, et al. Wien Klin Wochenschr 131(5–6):104–112, 2019; Zaharie, et al. J Crohns Colitis 10(3):306–314, 2016; El Mouzan, et al. Saudi J Gastroenterol 25:257–261, 2019). Intervening early in the disease course has significant implications on prognosis (Halme, et al. World J Gastroenterol 12(23):3668–3672, 2006), as early treatment can restore baseline function, while delays often result in permanent structural damage.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Cleynen I, Boucher G, Jostins L, Schumm LP, Zeissig S, Ahmad T, Andersen V, Andrews JM, Annese V, Brand S, Brant SR, Cho JH, Daly MJ, Dubinsky M, Duerr RH, Ferguson LR, Franke A, Gearry RB, Goyette P, Hakonarson H, Halfvarson J, Hov JR, Huang H, Kennedy NA, Kupcinskas L, Lawrance IC, Lee JC, Satsangi J, Schreiber S, Théâtre E, van der Meulen-de Jong AE, Weersma RK, Wilson DC; International Inflammatory Bowel Disease Genetics Consortium, Parkes M, Vermeire S, Rioux JD, Mansfield J, Silverberg MS, Radford-Smith G, McGovern DP, Barrett JC, Lees CW. Inherited determinants of Crohn's disease and ulcerative colitis phenotypes: a genetic association study. Lancet. 2016;387(10014):156–67. https://doi.org/10.1016/S0140-6736(15)00465-1. Epub 2015 Oct 18.
Nguyen VQ, Jiang D, Hoffman SN, Guntaka S, Mays JL, Wang A, Gomes J, Sorrentino D. Impact of diagnostic delay and associated factors on clinical outcomes in a U.S. Inflammatory Bowel Disease Cohort. Inflamm Bowel Dis. 2017;23(10):1825–31.
Novacek G, Gröchenig HP, Haas T, Wenzl H, Steiner P, Koch R, Feichtenschlager T, Eckhardt G, Mayer A, Kirchgatterer A, Ludwiczek O, Platzer R, Papay P, Gartner J, Fuchssteiner H, Miehsler W, Peters PG, Reicht G, Vogelsang H, Dejaco C, Waldhör T; Austrian IBD Study Group (ATISG). Diagnostic delay in patients with inflammatory bowel disease in Austria. Wien Klin Wochenschr 2019;131(5–6):104–112. https://doi.org/10.1007/s00508-019-1451-3. Epub 2019 Feb 4. PMID: 30715607.
Zaharie R, Tantau A, Zaharie F, Tantau M, Gheorghe L, Gheorghe C, Gologan S, Cijevschi C, Trifan A, Dobru D, Goldis A, Constantinescu G, Iacob R, Diculescu M; IBDPROSPECT Study Group. Diagnostic delay in romanian patients with inflammatory bowel disease: risk factors and impact on the disease course and need for surgery. J Crohns Colitis. 2016;10(3):306–14. https://doi.org/10.1093/ecco-jcc/jjv215. Epub 2015 Nov 20. PMID: 26589956; PMCID: PMC4957477.
El Mouzan MI, AlSaleem BI, Hasosah MY, Al-Hussaini AA, Al Anazi AH, Saadah OI, et al. Diagnostic delay of pediatric inflammatory bowel disease in Saudi Arabia. Saudi J Gastroenterol. 2019;25:257–61.
Halme L, Paavola-Sakki P, Turunen U, Lappalainen M, Farkkila M, Kontula K. Family and twin studies in inflammatory bowel disease. World J Gastroenterol. 2006;12(23):3668–72. https://doi.org/10.3748/wjg.v12.i23.3668.
Yang H, McElree C, Roth MP, Shanahan F, Targan SR, Rotter JI. Familial empirical risks for inflammatory bowel disease: differences between Jews and non-Jews. Gut. 1993;34(4):517–24. https://doi.org/10.1136/gut.34.4.517.
Uniken Venema WT, Voskuil MD, Dijkstra G, Weersma RK, Festen EA. The genetic background of inflammatory bowel disease: from correlation to causality. J Pathol. 2017;241(2):146–58. https://doi.org/10.1002/path.4817. Epub 2016 Nov 15.
Denson LA, Curran M, McGovern DPB, Koltun WA, Duerr RH, Kim SC, Sartor RB, Sylvester FA, Abraham C, de Zoeten EF, Siegel CA, Burns RM, Dobes AM, Shtraizent N, Honig G, Heller CA, Hurtado-Lorenzo A, Cho JH. Challenges in IBD research: precision medicine. Inflamm Bowel Dis. 2019;25(Suppl 2):S31–9. https://doi.org/10.1093/ibd/izz078.
Ni J, Wu GD, Albenberg L, Tomov VT. Gut microbiota and IBD: causation or correlation? Nat Rev Gastroenterol Hepatol. 2017;14(10):573–84. https://doi.org/10.1038/nrgastro.2017.88.
Ananthakrishnan AN. Epidemiology and risk factors for IBD. Nat Rev Gastroenterol Hepatol. 2015;12(4):205–17. https://doi.org/10.1038/nrgastro.2015.34. Epub 2015 Mar 3.
Ananthakrishnan AN, Bernstein CN, Iliopoulos D, Macpherson A, Neurath MF, Ali RAR, Vavricka SR, Fiocchi C. Environmental triggers in IBD: a review of progress and evidence. Nat Rev Gastroenterol Hepatol. 2018;15(1):39–49. https://doi.org/10.1038/nrgastro.2017.136. Epub 2017 Oct 11.
Forbes A, Escher J, Hébuterne X, Kłęk S, Krznaric Z, Schneider S, Shamir R, Stardelova K, Wierdsma N, Wiskin AE, Bischoff SC. ESPEN guideline: Clinical nutrition in inflammatory bowel disease. Clin Nutr. 2017;36(2):321–347. https://doi.org/10.1016/j.clnu.2016.12.027. Epub 2016 Dec 31. Erratum in: Clin Nutr. 2019 Jun;38(3):1486. Erratum in: Clin Nutr. 2019 Jun;38(3):1485.
Dahlhamer JM, Zammitti EP, Ward BW, Wheaton AG, Croft JB. Prevalence of inflammatory bowel disease among adults aged ≥18 years - United States, 2015. MMWR Morb Mortal Wkly Rep. 2016;65(42):1166–1169. https://doi.org/10.15585/mmwr.mm6542a3. PMID: 27787492.
Ruel J, Ruane D, Mehandru S, Gower-Rousseau C, Colombel JF. IBD across the age spectrum: is it the same disease? Nat Rev Gastroenterol Hepatol. 2014;11(2):88–98. https://doi.org/10.1038/nrgastro.2013.240. Epub 2013 Dec 17. PMID: 24345891.
Molodecky NA, et al. Increasing incidence and prevalence of the inflammatory bowel disease with time, based on systematic review. Gastroenterology. 2012;142:46–54.
Van Limbergen J, Russell RK, Drummond HE, Aldhous MC, Round NK, Nimmo ER, Smith L, Gillett PM, McGrogan P, Weaver LT, Bisset WM, Mahdi G, Arnott ID, Satsangi J, Wilson DC. Definition of phenotypic characteristics of childhood-onset inflammatory bowel disease. Gastroenterology. 2008;135(4):1114–22. https://doi.org/10.1053/j.gastro.2008.06.081. Epub 2008 Jul 3. PMID: 18725221.
Pigneur B, Seksik P, Viola S, Viala J, Beaugerie L, Girardet JP, Ruemmele FM, Cosnes J. Natural history of Crohn's disease: comparison between childhood- and adult-onset disease. Inflamm Bowel Dis. 2010;16(6):953–61. https://doi.org/10.1002/ibd.21152. PMID: 19834970.
Freeman HJ. Natural history and long-term clinical course of Crohn's disease. World J Gastroenterol. 2014;20(1):31–6. https://doi.org/10.3748/wjg.v20.i1.31.
Kariyawasam VC, et al. Natural history of elderly onset inflammatory bowel disease—Sydney IBD cohort (1942–2012). Gastroenterology 144(Suppl. 1), Mo1314 (2013).
Corinne G-R, Luc D, Gwénola V-M, Emmanuelle T, Franck B, Véronique M, Jean-Louis D, Guillaume S, Mamadou B, Raymond M, Éric L, Antoine C, Jean-Louis S, Dominique T, Jean-Frédéric C. The natural history of pediatric ulcerative colitis. Am J Gastroenterol. 2009;104(8):2008–88.
Magro F, Rodrigues A, Vieira AI, Portela F, Cremers I, Cotter J, Correia L, Duarte MA, Tavares ML, Lago P, Ministro P, Peixe P, Lopes S, Garcia EB. Review of the disease course among adult ulcerative colitis population-based longitudinal cohorts. Inflamm Bowel Dis. 2012;18(3):573–83. https://doi.org/10.1002/ibd.21815. Epub 2011 Jul 26. PMID: 21793126.
Kaplan GG, Ng SC. Understanding and preventing the global increase of inflammatory bowel disease. Gastroenterology. 2017;152(2):313–321.e2. https://doi.org/10.1053/j.gastro.2016.10.020.
Agrawal M, Shah S, Patel A, Pinotti R, Colombel JF, Burisch J. Changing epidemiology of immune-mediated inflammatory diseases in immigrants: a systematic review of population-based studies. J Autoimmun. 2019;105:102303. https://doi.org/10.1016/j.jaut.2019.07.002.
Afzali A, Cross RK. Racial and ethnic minorities with inflammatory bowel disease in the United States: a systematic review of disease characteristics and differences. Inflamm Bowel Dis. 2016;22(8):2023–40.
Sands B. From symptom to diagnosis: clinical distinctions among various forms of intestinal inflammation. Gastroenterology. 2004;126:1518–32.
Peyrin-Biroulet L, Loftus EV Jr, Colombel JF, Sandborn WJ. The natural history of adult Crohn's disease in population-based cohorts. Am J Gastroenterol. 2010;105(2):289–97. https://doi.org/10.1038/ajg.2009.579. Epub 2009 Oct 27. PMID: 19861953.
Subramanian R, Khardori R. Severe hypophosphatemia. Pathophysiologic implications, clinical presentations, and treatment. Medicine (Baltimore). 2000;79:1.
McClain C, Soutor C, Zieve L. Zinc deficiency: a complication of Crohn's disease. Gastroenterology. 1980;78(2):272–9.
Victor M. The Wernicke-Korsakoff syndrome and related neurologic disorders due to alcoholism and malnutrition. Contemp Neurol Series. 1989;30.
Said HM, Ross AC. Riboflavin. In: Ross AC, Caballero B, Cousins RJ, Tucker KL, Ziegler TR, editors. Modern nutrition in health and disease. 11th ed. Philadelphia: Lippincotto Williams and Wilkins; 2014.
Cervantes-Laurean N, McElvaney G, Moss J. Niacin. In: Shils M, editor. Modern nutrition in health and medicine. Lippincott, Philadelphia; 2000.
Hemmer B, Glocker FX, Schumacher M, et al. Subacute combined degeneration: clinical, electrophysiological, and magnetic resonance imaging findings. J Neurol Neurosurg Psychiatry. 1998;65:822.
Slater GH, Ren CJ, Siegel N, et al. Serum fat-soluble vitamin deficiency and abnormal calcium metabolism after malabsorptive bariatric surgery. J Gastrointest Surg. 2004;8:48.
Garg MK, Tandon N, Marwaha RK, et al. The relationship between serum 25-hydroxy vitamin D, parathormone and bone mineral density in Indian population. Clin Endocrinol. 2014;80:41.
Di Donato I, Bianchi S, Federico A. Ataxia with vitamin E deficiency: update of molecular diagnosis. Neurol Sci. 2010;31:511.
Oski FA, Barness LA. Vitamin E deficiency: a previously unrecognized cause of hemolytic anemia in the premature infant. J Pediatr. 1967;70:211.
Sankar MJ, Chandrasekaran A, Kumar P, et al. Vitamin K prophylaxis for prevention of vitamin K deficiency bleeding: a systematic review. J Perinatol. 2016;36(Suppl 1):S29.
Jaiser SR, Winston GP. Copper deficiency myelopathy. J Neurol. 2010;257:869.
Evans JA, Forcione DG, Friedman LS. Gastrointestinal complications in the postoperative period. Med Manag Surg Pat. 2008:275–347.
Andersson H, Bosaeus I, Fasth S, Hellberg R, Hultén L. Cholelithiasis and urolithiasis in Crohn’s disease. Scand J Gastroenterol. 1987;22:253–6.
Chadwick VS, Modha K. Dowling RH Mechanism for hyperoxaluria in patients with ileal dysfunction. N Engl J Med. 1973;289(4):172–6.
Abraham BP, Mehta S, El-Serag HB. Natural history of pediatric-onset inflammatory bowel disease: a systematic review. J Clin Gastroenterol. 2012;46(7):581–9. https://doi.org/10.1097/MCG.0b013e318247c32f.
Ingle SB, Loftus EV Jr. The natural history of perianal Crohn's disease. Dig Liver Dis. 2007;39(10):963–9. https://doi.org/10.1016/j.dld.2007.07.154. Epub 2007 Aug 27. PMID: 17720635
Kuehn HG, Gebbensleben O, Hilger Y, Rohde H. Relationship between anal symptoms and anal findings. Int J Med Sci. 2009;6(2):77–84. https://doi.org/10.7150/ijms.6.77.
Adegbola SO, Pisani A, Sahnan K, Tozer P, Ellul P, Warusavitarne J. Medical and surgical management of perianal Crohn's disease. Ann Gastroenterol. 2018;31(2):129–39. https://doi.org/10.20524/aog.2018.0236
Parks AG, Gordon PH, Hardcastle JD. A classification of fistula-in-ano. Br J Surg. 1976;63:1–12.
Hirten RP, Shah S, Sachar DB, Colombel J-F. The management of intestinal penetrating Crohn's Disease. Inflamm Bowel Dis. 2018;24(4):752–65. https://doi.org/10.1093/ibd/izx108.
Schwartz DA, Loftus EV, Tremaine WJ, Panaccione R, Harmsen WS, Zinsmeister AR, et al. The natural history of fistulizing Crohn's disease in Olmsted County. Minnesota Gastroenterol. 2002;122:875–80.
Kobayashi H, Sugihara K. Successful management of rectovaginal fistula treated by endorectal advancement flap: report of two cases and literature review. Springerplus. 2015;4:21. Published 2015 Jan 15. https://doi.org/10.1186/s40064-015-0799-8.
Menteş BB, Leventoğlu S, Osmanov İ, Kösehan D, Erol T. Anal abscess due to leech therapy of hemorrhoids: mumbo jumbo is still in vogue. J Surg Case Rep. 2019;2019(7):rjz218. Published 2019 Jul 31. https://doi.org/10.1093/jscr/rjz218.
Chen WT, Chi CC. Association of hidradenitis suppurativa with inflammatory bowel disease: a systematic review and meta-analysis. JAMA Dermatol. 2019;155(9):1022–7. https://doi.org/10.1001/jamadermatol.2019.0891.
Podugu A, Tandon K, Castro FJ. Crohn's disease presenting as acute gastrointestinal hemorrhage. World J Gastroenterol. 2016;22(16):4073–8. https://doi.org/10.3748/wjg.v22.i16.4073.
Mills S, Stamos MJ. Colonic Crohn's disease. Clin Colon Rectal Surg. 2007;20(4):309–13. https://doi.org/10.1055/s-2007-991030.
Van Limbergen J, Russell RK, Drummond HE, Aldhous MC, Round NK, Nimmo ER, Smith L, Gillett PM, McGrogan P, Weaver LT, Bisset WM, Mahdi G, Arnott ID, Satsangi J, Wilson DC. Definition of phenotypic characteristics of childhood-onset inflammatory bowel disease. Gastroenterology. 2008;135:1114–22.
Nóbrega AC, Ferreira BR, Oliveira GJ, et al. Dyspeptic symptoms and delayed gastric emptying of solids in patients with inactive Crohn's disease. BMC Gastroenterol. 2012;12:175. Published 2012 Dec 7. https://doi.org/10.1186/1471-230X-12-175.
Vadstrup K, Alulis S, Borsi A, Jørgensen TR, Nielsen A, Munkholm P, Qvist N. Extraintestinal manifestations and other comorbidities in ulcerative colitis and Crohn Disease: a Danish Nationwide Registry Study 2003–2016. Crohn's & Colitis 360. 2020;2(3):otaa070.
Vavricka SR, Schoepfer A, Scharl M, Lakatos PL, Navarini A, Rogler G. Extraintestinal manifestations of inflammatory bowel disease. Inflamm Bowel Dis. 2015;21(8):1982–92.
Vlachos C, Gaitanis G, Katsanos KH, Christodoulou DK, Tsianos E, Bassukas ID. Psoriasis and inflammatory bowel disease: links and risks. Psoriasis (Auckl). 2016;6:73–92. Published 2016 Jul 20. https://doi.org/10.2147/PTT.S85194.
Fausa O, Schrumpf E, Elgjo K. Relationship of inflammatory bowel disease and primary sclerosing cholangitis. Semin Liver Dis. 1991;11(01):31–9.
Fumery M, Singh S, Dulai PS, Gower-Rousseau C, Peyrin-Biroulet L, Sandborn WJ. Natural history of adult ulcerative colitis in population-based cohorts: a systematic review. Clin Gastroenterol Hepatol. 2018;16(3):343–56.e3.
Heuschen UA, Hinz U, Allemeyer EH, et al. Backwash ileitis is strongly associated with colorectal carcinoma in ulcerative colitis. Gastroenterology. 2001;120(4):841–7.
Truelove SC, Witts LJ. Cortisone in ulcerative colitis; final report on a therapeutic trial. Br Med J. 1955;2(4947):1041–8. https://doi.org/10.1136/bmj.2.4947.1041. PMID: 13260656; PMCID: PMC1981500.
Walmsley RS, Ayres RC, Pounder RE, Allan RN. A simple clinical colitis activity index. Gut. 1998;43:29–32.
Schroeder KW, Tremaine WJ, Ilstrup DM. Coated oral 5-aminosalicylic acid therapy for mildly to moderately active ulcerative colitis A randomized study. N Engl J Med. 1987;317:1625–9.
Wéra O, Lancellotti P, Oury C. The dual role of neutrophils in inflammatory bowel diseases. J Clin Med. 2016;5(12):118. Published 2016 Dec 17.
Sandborn WJ, Panes J, Zhang H, et al. Correlation between concentrations of fecal calprotectin and outcomes of patients with ulcerative colitis in a phase 2 trial. Gastroenterology. 2016;150:96–102.
Mosli MH, Zou G, Garg SK, et al. C-reactive protein, fecal calprotectin, and stool lactoferrin for detection of endoscopic activity in symptomatic inflammatory bowel disease patients: A systematic review and meta-analysis. Am J Gastroenterol. 2015;110:802–19.
Patel A, Panchal H, Dubinsky MC. Fecal calprotectin levels predict histological healing in ulcerative colitis. Inflamm Bowel Dis. 2017;23:1600–4.
Lee SH, Kim MJ, Chang K, et al. Fecal calprotectin predicts complete mucosal healing and better correlates with the Ulcerative Colitis Endoscopic Index of Severity than with the Mayo endoscopic subscore in patients with ulcerative colitis. BMC Gastroenterol. 2017;17:110.
Theede K, Holck S, Ibsen P, et al. Fecal Calprotectin predicts relapse and histological mucosal healing in ulcerative colitis. Inflamm Bowel Dis. 2016;22:1042–8.
Wright E, Kamm M, De Cruz P, et al. Measurement of fecal calprotectin improves monitoring and detection of recurrence of Crohn's disease after surgery. Gastroenterology. 2015;148:938–47.
Ferreiro-Iglesias R, Barreiro-de Acosta M, Otero Santiago M, et al. Fecal calprotectin as predictor of relapse in patients with inflammatory bowel disease under maintenance infliximab therapy. J Clin Gastroenterol. 2016;50:147–51.
Mishra A, Makharia GK. Techniques of functional and motility test: how to perform and interpret intestinal permeability. J Neurogastroenterol Motil. 2012;18(4):443–7. https://doi.org/10.5056/jnm.2012.18.4.443.
Andre F, Andre C, Emery Y, Forichon J, Descos L, Minaire Y. Assessment of the lactulose-mannitol test in Crohn’s disease. Gut. 1988;29(4):511–5.
Mendoza JL, Abreu MT. Biological markers in inflammatory bowel disease: practical consideration for clinicians. Gastroenterologie Clinique Et Biologique. 2009;33:S158–73.
Turner D, Mack DR, Hyams J, et al. C-reactive protein (CRP), erythrocyte sedimentation rate (ESR) or both? A systematic evaluation in pediatric ulcerative colitis. J Crohn's Colitis. 2011;5(5):423–9.
Knovich W, Coffman LG, Torti FM, Torti SV. Serum ferritin: past, present and future. Biochim Biophys Acta. 2010;1800(8):760–9. https://doi.org/10.1016/j.bbagen.2010.03.011.
Lipschitz DA, Cook JD, Finch CA. A clinical evaluation of serum ferritin as an index of iron stores. N Engl J Med 2010.
Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan. China JAMA Intern Med. 2020;180(7):934–43. https://doi.org/10.1001/jamainternmed.2020.0994.
Ko CW, et al. AGA clinical practice guidelines on the gastrointestinal evaluation of iron deficiency anemia. Gastroenterology. 2020;159(3):1085–94.
Peyrin-Biroulet L, Standaert-Vitse A, Branche J, Chamaillard M. IBD serological panels: facts and perspectives. Infl amm Bowel Dis. 2007;13:1561–6.
Birimberg-Schwartz L, Wilson DC, Kolho KL, et al. pANCA and ASCA in children with IBD-unclassified, crohn's colitis, and ulcerative colitis-a longitudinal report from the IBD Porto Group of ESPGHAN. Inflamm Bowel Dis. 2016:1908–14.
Benor S, Russell GH, Silver M, Israel EJ, Yuan Q, Winter HS. Shortcomings of the inflammatory bowel disease Serology 7 panel. Pediatrics. 2010;125:1230–6.
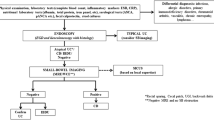
Deepak P, Bruining DH. Radiographical evaluation of ulcerative colitis. Gastroenterol Rep. 2014;2(3):169–77.
Kilcoyne A, Kaplan JL, Gee MS. Inflammatory bowel disease imaging: current practice and future directions. World J Gastroenterol. 2016;22(3):917.
Levine MS, Laufer I. The upper gastrointestinal series at a crossroads. AJR. AJR Am J Roentgenol. 1993;161(6):1131–7.
Solem CA, Loftus EV Jr, Fletcher JG, Baron TH, Gostout CJ, Petersen BT, Tremaine WJ, Egan LJ, Faubion WA, Schroeder KW, Pardi DS. Small-bowel imaging in Crohn's disease: a prospective, blinded, 4-way comparison trial. Gastrointest Endosc. 2008;68(2):255–66.
Elsayes KM, Al-Hawary MM, Jagdish J, Ganesh HS, Platt JF. CT enterography: principles, trends, and interpretation of findings. Radiographics. 2010;30(7):1955–70.
Mantarro A, Scalise P, Guidi E, Neri E. Magnetic resonance enterography in Crohn’s disease: how we do it and common imaging findings. World J Radiol. 2017;9(2):46.
Rudnick MR, Berns JS, Cohen RM, Goldfarb S. Nephrotoxic risks of renal angiography: contrast media associated nephrotoxicity and atheroembolism—a critical review. Am J Kidney Dis. 1994;24(4):713–27.
Schwab SJ, Hlatky MA, Pieper KS, Davidson CJ, Morris KG, Skelton TN, Bashore TM. Contrast nephrotoxicity: a randomized controlled trial of a nonionic and an ionic radiographic contrast agent. New England J Med. 1989;320(3):149–53.
Zhang B, Liang L, Chen W, Liang C, Zhang S. An updated study to determine association between gadolinium-based contrast agents and nephrogenic systemic fibrosis. PLoS One. 2015;10(6):e0129720.
Liu W, Liu J, Xiao W, Luo G. A diagnostic accuracy meta-analysis of CT and MRI for the evaluation of small bowel Crohn disease. Acad Radiol. 2017;24(10):1216–25.
Siddiki H, Fletcher JG, Hara AK, Kofler JM, McCollough CH, Fidler JL, Guimaraes L, Huprich JE, Sandborn WJ, Loftus EV Jr, Mandrekar J. Validation of a lower radiation computed tomography enterography imaging protocol to detect Crohn's disease in the small bowel. Inflamm Bowel Dis. 2011;17(3):778–86.
Korutz AW, Obajuluwa A, Lester MS, McComb EN, Hijaz TA, Collins JD, Dandamudi S, Knight BP, Nemeth AJ. Pacemakers in MRI for the neuroradiologist. Am J Neuroradiol. 2017;38(12):2222–30.
Shin DY, Park S, Kim A, Kim ES, Jeon HH. Compatibility of endoclips in the gastrointestinal tract with magnetic resonance imaging. Sci Rep. 2020;10(1):1–7.
Munn Z, Moola S, Lisy K, Riitano D, Murphy F. Claustrophobia in magnetic resonance imaging: a systematic review and meta-analysis. Radiography. 2015;21(2):e59–63.
Kanal E, Barkovich AJ, Bell C, Borgstede JP, Bradley WG Jr, Froelich JW. ACR guidance document for safe MR practices. 2007;188(6):1447–74.
Prola-Netto J, Woods M, Roberts VH, Sullivan EL, Miller CA, Frias AE, Oh KY. Gadolinium chelate safety in pregnancy: barely detectable gadolinium levels in the juvenile nonhuman primate after in utero exposure. Radiology. 2018;286(1):122–8.
Bandorski D, Höltgen R, Stunder D, Keuchel M. Capsule endoscopy in patients with cardiac pacemakers, implantable cardioverter defibrillators and left heart assist devices. Ann Gastroenterol. 2014;27(1):3.
Harris LA, Hansel SL, Rajan E, Srivathsan K, Rea R, Crowell MD, Fleischer DE, Pasha SF, Gurudu SR, Heigh RI, Shiff AD. Capsule endoscopy in patients with implantable electromedical devices is safe. Gastroenterol Res Pract. 2013;2013
Dionisio PM, Gurudu SR, Leighton JA, Leontiadis GI, Fleischer DE, Hara AK, Heigh RI, Shiff AD, Sharma VK. Capsule endoscopy has a significantly higher diagnostic yield in patients with suspected and established small-bowel Crohn's disease: a meta-analysis. Am J Gastroenterol. 2010;105(6):1240–8.
Hall B, Holleran G, Costigan D, McNamara D. Capsule endoscopy: high negative predictive value in the long term despite a low diagnostic yield in patients with suspected Crohn's disease. United European Gastroenterol J. 2013;1(6):461–6.
Robertson KD, Singh R. Capsule endoscopy. StatPearls [Internet]. 2020.
Park SK, Ye BD, Kim KO, Park CH, Lee WS, Jang BI, Jeen YT, Choi MG, Kim HJ, Korean Gut Image Study Group. Guidelines for video capsule endoscopy: emphasis on Crohn's disease. ClinEndosc. 2015;48(2):128.
Spada C, Shah SK, Riccioni ME, Spera G, Marchese M, Iacopini F, Familiari P, Costamagna G. Video capsule endoscopy in patients with known or suspected small bowel stricture previously tested with the dissolving patency capsule. J Clin Gastroenterol. 2007;41(6):576–82.
Rozendorn N, Klang E, Lahat A, Yablecovitch D, Kopylov U, Eliakim A, Ben-Horin S, Amitai MM. Prediction of patency capsule retention in known Crohn's disease patients by using magnetic resonance imaging. Gastrointest Endosc. 2016;83(1):182–7.
Nemeth A, Kopylov U, Koulaouzidis A, Johansson GW, Thorlacius H, Amre D, Eliakim R, Seidman EG, Toth E. Use of patency capsule in patients with established Crohn’s disease. Endoscopy. 2016;48(04):373–9.
Enns RA, Hookey L, Armstrong D, Bernstein CN, Heitman SJ, Teshima C, Leontiadis GI, Tse F, Sadowski D. Clinical practice guidelines for the use of video capsule endoscopy. Gastroenterology. 2017;152(3):497–514.
Mustafa BF, Samaan M, Langmead L, Khasraw M. Small bowel video capsule endoscopy: an overview. Expert Rev Gastroenterol Hepatol. 2013;7(4):323–9.
Cave DR, Hakimian S, Patel K. Current controversies concerning capsule endoscopy. Dig Dis Sci. 2019;64(11):3040–7.
Jensen MD, Nathan T, Rafaelsen SR, Kjeldsen J. Diagnostic accuracy of capsule endoscopy for small bowel Crohn's disease is superior to that of MR enterography or CT enterography. Clin Gastroenterol Hepatol. 2011;9(2):124–9.
Griffin N, Grant LA, Anderson S, Irving P, Sanderson J. Small bowel MR enterography: problem solving in Crohn's disease. Insights Imaging. 2012;3(3):251–63. https://doi.org/10.1007/s13244-012-0154-3.
Eglinton TW, Barclay ML, Gearry RB, Frizelle FA. The spectrum of perianal Crohn’s disease in a population-based cohort. Dis Colon Rectum 2012;55(7):773–7.
Hellers G, Bergstrand O, Ewerth S, Holmström B. Occurrence and outcome after primary treatment of anal fistulae in Crohn's disease. Gut. 1980;21(6):525–7.
Yamaguchi A, Matsui T, Sakurai T, Ueki T, Nakabayashi S, Yao T, Futami K, Arima S, Ono H. The clinical characteristics and outcome of intraabdominal abscess in Crohn’s disease. J Gastroenterol. 2004;39(5):441–8.
Yoon SJ, Yoon DY, Kim SS, Rho YS, Chung EJ, Eom JS, Lee JS. CT differentiation of abscess and non-infected fluid in the postoperative neck. Acta Radiol. 2013;54(1):48–53.
Solberg IC, Vatn MH, Hoie O, et al. Clinical course in Crohn's disease: results of a Norwegian population-based ten-year follow-up study. Clin Gastroenterol Hepatol. 2007;5:1430–8.
Henriksen M, Jahnsen J, Lygren I, et al. Clinical course in Crohn's disease: results of a five-year population-based follow-up study (the IBSEN study). Scand J Gastroenterol. 2007;42:602–10.
Thia KT, Sandborn WJ, Harmsen WS, et al. Risk factors associated with progression to intestinal complications of Crohn's disease in a population-based cohort. Gastroenterology. 2010;139:1147–55.
Ramadas AV, Gunesh S, Thomas GA, et al. Natural history of Crohn's disease in a population-based cohort from Cardiff (1986–2003): a study of changes in medical treatment and surgical resection rates. Gut. 2010;59:1200–6.
Lakatos PL, Golovics PA, David G, et al. Has there been a change in the natural history of Crohn's disease? Surgical rates and medical management in a population-based inception cohort from Western Hungary between 1977–2009. Am J Gastroenterol. 2012;107:579–88.
Gower-Rousseau C, Vasseur F, Fumery M, et al. Epidemiology of inflammatory bowel diseases: new insights from a French population-based registry (EPIMAD). Dig Liver Dis. 2013;45:89–94.
Louis E, Collard A, Oger AF, et al. Behaviour of Crohn's disease according to the Vienna classification: changing pattern over the course of the disease. Gut. 2001;49:777–82.
Cosnes J, Cattan S, Blain A, et al. Long-term evolution of disease behavior of Crohn's disease. Inflamm Bowel Dis. 2002;8:244–50.
Panes J, Bouzas R, Chaparro M, et al. Systematic review: the use of ultrasonography, computed tomography and magnetic resonance imaging for the diagnosis, assessment of activity and abdominal complications of Crohn's disease. Aliment Pharmacol Ther. 2011;34:125–45.
Negreanu L, Voiosu T, State M, Voiosu A, Bengus A, Mateescu BR. Endoscopy in inflammatory bowel disease: from guidelines to real life. Ther Adv Gastroenterol. 2019;12:1756284819865153.
Bharadwaj S, Narula N, Tandon P, Yaghoobi M. Role of endoscopy in inflammatory bowel disease. Gastroenterology Report. 2018;6(2):75–82.
Pera A, Bellando P, Caldera D, Ponti V, Astegiano M, Barletti C, David E, Arrigoni A, Rocca G, Verme G. Colonoscopy in inflammatory bowel disease: diagnostic accuracy and proposal of an endoscopic score. Gastroenterology. 1987;92(1):181–5.
Mowat C, Cole A, Windsor AL, Ahmad T, Arnott I, Driscoll R, Mitton S, Orchard T, Rutter M, Younge L, Lees C. Guidelines for the management of inflammatory bowel disease in adults. Gut. 2011;60(5):571–607.
Bentley E, Jenkins D, Campbell F, Warren B. How could pathologists improve the initial diagnosis of colitis? Evidence from an international workshop. J Clin Pathol. 2002;55(12):955–60.
Shergill AK, Lightdale JR, Bruining DH, Acosta RD, Chandrasekhara V, Chathadi KV, Decker GA, Early DS, Evans JA, Fanelli RD, Fisher DA. The role of endoscopy in inflammatory bowel disease. Gastrointest Endosc. 2015;81(5):1101–21.
Haskell H, Andrews CW Jr, Reddy SI, Dendrinos K, Farraye FA, Stucchi AF, Becker JM, Odze RD. Pathologic features and clinical significance of “backwash” ileitis in ulcerative colitis. Am J Surg Pathol. 2005;29(11):1472–81.
Annunziata ML, Caviglia R, Papparella LG, Cicala M. Upper gastrointestinal involvement of Crohn’s disease: a prospective study on the role of upper endoscopy in the diagnostic work-up. Dig Dis Sci. 2012;57(6):1618–23.
Mary JY, Modigliani R. Development and validation of an endoscopic index of the severity for Crohn's disease: a prospective multicentre study. Groupe d'Etudes Therapeutiques des Affections Inflammatoires du Tube Digestif (GETAID). Gut. 1989;30(7):983–9.
Daperno M, D'Haens G, Van Assche G, Baert F, Bulois P, Maunoury V, Sostegni R, Rocca R, Pera A, Gevers A, Mary JY. Development and validation of a new, simplified endoscopic activity score for Crohn's disease: the SES-CD. Gastrointest Endosc. 2004;60(4):505–12.
Khanna R, Zou G, D'Haens G, Rutgeerts P, McDonald JW, Daperno M, Feagan BG, Sandborn WJ, Dubcenco E, Stitt L, Vandervoort MK. Reliability among central readers in the evaluation of endoscopic findings from patients with Crohn's disease. Gut. 2016;65(7):1119–25.
Vashist NM, Samaan M, Mosli MH, Parker CE, MacDonald JK, Nelson SA, Zou GY, Feagan BG, Khanna R, Jairath V. Endoscopic scoring indices for evaluation of disease activity in ulcerative colitis. Cochrane Database Syst Rev. 2018;1
de Jong DC, Löwenberg M, Koumoutsos I, Ray S, Mawdsley J, Anderson S, Sanderson JD, Gecse K, Ponsioen CY, D’Haens GR, Irving PM. Validation and investigation of the operating characteristics of the ulcerative colitis endoscopic index of severity. Inflamm Bowel Dis. 2019;25(5):937–44.
Travis SP, Schnell D, Feagan BG, Abreu MT, Altman DG, Hanauer SB, Krzeski P, Lichtenstein GR, Marteau PR, Mary JY, Reinisch W. The impact of clinical information on the assessment of endoscopic activity: characteristics of the ulcerative colitis endoscopic index of severity [UCEIS]. J Crohn's Colitis. 2015;9(8):607–16.
Travis SP, Schnell D, Krzeski P, Abreu MT, Altman DG, Colombel JF, Feagan BG, Hanauer SB, Lichtenstein GR, Marteau PR, Reinisch W. Reliability and initial validation of the ulcerative colitis endoscopic index of severity. Gastroenterology. 2013;145(5):987–95.
Annese V, Daperno M, Rutter MD, Amiot A, Bossuyt P, East J, Ferrante M, Götz M, Katsanos KH, Kießlich R, Ordás I. European evidence based consensus for endoscopy in inflammatory bowel disease. J Crohn's Colitis. 2013;7(12):982–1018.
Rubin DT, Ananthakrishnan AN, Siegel CA, Sauer BG, Long MD. ACG Clinical Guideline: Ulcerative Colitis in Adults. Am J Gastroenterol. 2019;114:384–413; Farraye FA, Odze RD, Eaden J, Itzkowitz SH. AGA technical review on the diagnosis and management of colorectal neoplasia in inflammatory bowel disease. Gastroenterology. 2010;138:746–74, 774.e1–4; quiz e12–13.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Passarella, A., Grewal, P., Vrabie, R. (2021). Diagnosis and Monitoring in Inflammatory Bowel Disease: Who, When, Where, and How. In: Rajapakse, R. (eds) Inflammatory Bowel Disease. Clinical Gastroenterology. Humana, Cham. https://doi.org/10.1007/978-3-030-81780-0_2
Download citation
DOI: https://doi.org/10.1007/978-3-030-81780-0_2
Published:
Publisher Name: Humana, Cham
Print ISBN: 978-3-030-81779-4
Online ISBN: 978-3-030-81780-0
eBook Packages: MedicineMedicine (R0)