Abstract
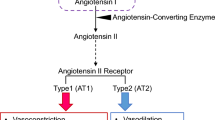
Genetically altered rat and mouse models have been instrumental in the functional analysis of genes in a physiological context. In particular, studies on the renin-angiotensin system (RAS) have profited from this technology in the past. In this review, we summarize the existing animal models for the protective axis of the RAS consisting of angiotensin-converting enzyme 2 (ACE2), angiotensin-(1-7)(Ang-(1-7), and its receptor Mas. With the help of models with altered expression of the components of this axis in the brain and cardiovascular organs, its physiological and pathophysiological functions have been elucidated. Thus, novel opportunities for therapeutic interventions in cardiovascular diseases were revealed targeting ACE2 or Mas.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Transgenic and knockout animal models are the most effective tools to study cardiovascular hormone systems, since they reveal effects of changes in single components of these systems on the whole physiology. In particular, studies on the renin-angiotensin systems (RAS) have profited from this technology in recent decades [3, 5, 58]. Therefore, it was warranted to establish such models also for the novel RAS consisting of ACE2, Ang-(1-7), and Mas (Table 1). Despite that these three components comprise a common axis, distinct phenotypes of models with one of the components altered are expected since each of the three components has distinct additional functions independent from the two other molecules. ACE2, in particular, is a protein with several functions, a carboxypeptidase metabolizing a multitude of peptides, such as AngII and apelins, thereby either activating or inactivating them [104], a protein with a collectrin domain, which is involved in amino acid uptake in the gut [34, 95], and the receptor for the severe acute respiratory syndrome (SARS) coronavirus [45]. Moreover, also Ang-(1-7) may interact with other receptors than Mas and Mas may have other ligands or exert ligand-independent effects [4, 86].
ACE2 Models
ACE2 Knockout Mice
Since the ACE2 gene is localized on the X-chromosome, male mice with ACE2 gene deletion (ACE2−/y) are already deficient in the enzyme in the hemizygous state. Based on the pleiotropic actions of this protein, mice lacking ACE2 are expected to exhibit increased levels of AngII, decreased levels of Ang-(1-7) and tryptophan, as well as alterations in other peptide levels, which all may contribute to observed phenotypes. ACE2−/y mice and also heterozygous female ACE2+/− mice were more susceptible to cardiac injury induced by pressure overload, AngII infusion, or diabetes [69, 109, 115, 125] and ACE2−/y mice developed cardiac abnormalities at older age [17] probably due to an increased level of Ang II [68]. However, the spontaneous appearance of cardiac alterations could not be confirmed by another group and therefore remains controversial [31, 32, 125]. However, obesity-induced epicardial inflammation was worsened and caused cardiac dysfunction in ACE2−/y mice [70]. Furthermore, in heart and skeletal muscle, ACE2 was involved in training-induced physiological hypertrophy [59].
There were also inconsistencies in the reports about hypertension in ACE2−/y mice, but it is now accepted that this phenotype is depending on the strain of mice appearing in C57BL/6 and FVB/N but not in 129 mice [32, 38, 77, 101]. ACE2-deficient mice on C57BL/6 background even developed a pre-ecclampsia-like syndrome when pregnant [8] and placental hypoxia and uterine artery dysfuncion caused fetal growth restriction in these animals [124]. In ACE2−/− female mice, estrogen cannot inhibit obesity-induced hypertension in contrast to wild-type controls [114]. We and others have described AngII-dependent endothelial dysfunction in ACE2-deficient mice [49, 77], which probably mediated the prohypertensive phenotype. However, an increased sympathetic outflow may have also contributed [119]. On the other hand, ACE2 also degrades the vasodilator apelin peptides which consequently accumulate in ACE2−/y mice and counteract the effects on the RAS [110]. Nevertheless, there were several other vascular effects of genetic ACE2-deletion such as a worsening of atherosclerosis and aortic aneurysm in apolipoprotein E (ApoE)- and low-density lipoprotein receptor-deficient mice [63, 81, 99, 100] and an increased neointima formation after vascular injury [81], to which the endothelial dysfunction was a major contributor.
In double knockout mice for ACE2 and ApoE, also the renal injury induced by atherosclerosis was aggravated [38]. Moreover, ACE2−/y mice spontaneously developed glomerulosclerosis in older age [67] and were more susceptible to renal ischemia/reperfusion injury due to increased cytokine expression, inflammation, and oxidative stress [23]. Accordingly, genetic ACE2 deficiency led to accelerated nephropathy in streptozotocin (STZ)-induced and Akita diabetic mice [91, 115]. Furthermore, knockout mice for ACE2 infused with AngII showed enhanced collagen I deposition in renal glomeruli and expression of genes related to fibrosis, such as smooth muscle actin, transforming growth factor β (TGF-β), and procollagen I, probably through activation of ERK1/2 and enhancement of protein kinase C levels [133]. ACE2-deficient mice also showed a worse outcome in shock-induced kidney injury [127], chronic hepatic injury [66], liver steatosis [12, 64], and cerulein-induced pancreatitis [48].
The lung is a major site of ACE2 expression. Accordingly, ACE2−/y mice exhibited an aggravated pathogenesis of lung injury induced by cigarette smoke, air pollution, bleomycin, influenza virus or respiratory syncytial virus [30, 36, 46, 80, 134], of pulmonary hypertension [129], and of acute respiratory distress syndrome [37]. In most of these injury models, the increased oxidative stress observed in kidneys [116], livers [12, 64], and vessels [71] of ACE2−/y mice contributed to the exacerbation.
ACE2 in the gut with its collectrin domain is part of the amino acid uptake system and, therefore, mice lacking this protein showed reduced tryptophan in the blood, an altered gut microflora, and intestinal inflammation [34, 95]. These results were recently confirmed in a novel ACE2-deficient mouse model on an outbred genetic background generated by transcription-activator-like effector nucleases (TALEN) [47]. Whether the collectrin-domain-dependent effects contributed to the metabolic alterations shown in ACE2-deficient mice, such as insulin resistance and impaired glucose homeostasis [12, 63] in particular under a high-fat diet [15, 50, 90, 92, 123] needs still to elucidated [7]. However, in the liver, the carboxypeptidase function of ACE2 was more relevant for these metabolic effects since they could be ameliorated by Ang-(1-7) infusion [12].
ACE2 in the brain also influences behavior since ACE2-deficient mice showed impaired performance in cognition and memory tests [111].
ACE2 S680D Knockin Mouse
Recently, it was discovered that serine 680 of mouse ACE2 is phosphorylated by AMP kinase, leading to increased stability of the protein. When this phosphorylation was mimicked (S680D) in knockin mice by CRISPR/Cas9 technology, the resulting animals were partially resistant to a pulmonary hypertension model [129].
ACE2 Knockout Rats
ACE2 knockout rats have recently been established using TALEN technology [130]. These animals exhibited cardiac hypertrophy and impaired heart function; however, their blood pressure was not reported. Therefore, it remains unclear whether the cardiac effects are direct or caused by hypertension.
Inducible Mouse ACE2 Overexpression in Mouse
In order to allow tissue-specific activation of ACE2 expression, the mouse ACE2 coding region was knocked into the Rosa26 locus of mice with a Stop-lox cassette in front of it, which inhibits transcription. This cassette can be removed by Cre-recombinase expression and then ACE2 gets highly expressed in the cells expressing Cre-recombinase. When Cre-recombinase was expressed in the germline, ubiquitously ACE2 overexpressing mice resulted, which were protected from post-infarction cardiac dysfunction [75] and exhibited less anxiety-related behavior [107]. The same behavioral effects were also observed when the gene was only activated in CRH (corticotropin-releasing hormone) expressing cells using the corresponding Cre-recombinase-expressing mouse for breeding with the ACE2/Rosa26 animals [108].
Human ACE2 Overexpression in Mouse
Human ACE2 is hijacked by the SARS virus as a receptor to enter cells. In order to create a model for this disease, mice were “humanized” by several groups by inserting human ACE2 transgenes in their genome either using the ACE2 promoter itself [126], the ubiquitously active cytomegalovirus (CMV) promoter [102, 128], or the airway-specific cytokeratin 18 promoter [53, 62]. These animals were also suitable for studies on the role of ACE2 in other diseases and therefore the first model was tested in a kidney injury model and showed a protected phenotype [127]. Moreover, it was shown to be protected from AngII-induced hypertension and myocardial fibrosis [109].
Human ACE2 Overexpression in Mouse Heart
When human ACE2 was overexpressed in hearts of transgenic mice, surprisingly ventricular tachycardia and sudden death was observed accompanied by a dysregulation of connexin expression [21]. Apelin, which is also a substrate for ACE2 [104], may in this case be lacking and this deficiency may have caused the cardiac dysfunction [41].
Human ACE2 Overexpression in Mouse Podocytes
When human ACE2 was overexpressed in kidneys of transgenic mice, particularly in podocytes using the nephrin promoter, the animals became protected from diabetes-induced renal injury [61]. The authors provided evidence that the relative amounts of AngII and Ang-(1-7) are critical for the phenotype by increased AngII upregulating TGF-β.
Human ACE2 Overexpression in Mouse Brain
When human ACE2 was overexpressed in brains of transgenic mice using the synapsin promoter, a protective phenotype is observed for several cardiovascular diseases. This included hypertension induced by peripheral infusions of AngII [26] and by desoxycorticosterone acetate (DOCA)/salt treatment [118], cardiac hypertrophy elicited by AngII [25], coronary ligation-induced chronic heart failure [120], and stroke triggered by middle cerebral artery occlusion [14, 132]. In another model, the ACE2 transgene was flanked by loxP sites and it could therefore be specifically deleted in distinct brain regions by the local injection of Cre-recombinase-expressing adeno-associated viruses to assess the relevance of these areas for the blood pressure increase after DOCA/salt treatment. Such experiments revealed the paraventricular nucleus of the hypothalamus and the subfornical organ as important but not exclusive contributors to hypertension development [117]. The shift in the balance between Ang-(1-7) and AngII in brain regions important for cardiovascular control modulated local NO and ROS production as well as cyclooxygenase-mediated neuroinflammation [97] and likely caused the beneficial effects of ACE2 in the brain. Accordingly, the AngII-dependent deleterious effects on brain tissues observed in double transgenic mice expressing human angiotensinogen and human renin were mitigated in triple transgenic animals additionally expressing human ACE2 [14, 131].
Human ACE2 Overexpression in Rat Vascular Smooth Muscle
When we overexpressed human ACE2 in vascular smooth muscle of transgenic rats of the spontaneously hypertensive stroke-prone (SHRSP) strain using the smooth muscle myosin heavy chain promoter, blood pressure was significantly reduced [79]. This confirmed a study postulating that reduced ACE2 is an important genetic determinant for hypertension in this strain [17]. Reduced blood pressure was accompanied by decreased oxidative stress and improved endothelial function [79].
Mas Models
Mas Knockout Mice
When we generated Mas-deficient (Mas−/−) mice, it was not yet known that it is the receptor for Ang-(1-7) [105]. Therefore, phenotyping concentrated on the brain as major Mas-expressing organ. Male (but not female [106]) Mas-deficient mice showed increased anxiety-like behavior and long-term potentiation (LTP) in the hippocampus [105]. Surprisingly, despite the improved LTP, object recognition memory was impaired [43]. However, Mas−/− mice showed delayed extinction of fear memory [42] and were protected from cognitive impairments induced by ischemia but only in the presence of the AngII AT2 receptor [35] supporting a role of the dimerization of both receptors in brain function [44].
After our discovery that Mas is the receptor for Ang-(1-7) [85], we performed comprehensive cardiovascular phenotyping. Mas-deficient mice on the C57BL/6 background exhibited spontaneous cardiac fibrosis and dysfunction [13, 72, 83, 113]. Increased oxidative stress and endothelial dysfunction were observed on all genetic backgrounds studied (C57BL/6 and FVB/N) [33, 78, 121], but only resulted in hypertension in FVB/N mice. Possibly, an autonomic dysbalance in Mas−/− mice also contributed to the increased blood pressure [76]. Moreover, regional blood flow and local vascular resistance were differentially altered in different tissues of Mas−/− mice [10], which may also be the cause for the increased vascular resistance in the corpus cavernosum and the resulting erectile dysfunction observed in these mice [29].
Mas−/− mice showed an impaired renal function with increased urinary volume and proteinuria [74]. However, Esteban and coworkers found that Mas knockout mice presented an attenuation of renal damage in the unilateral ureteral obstruction and in the renal ischemia/reperfusion model [22]. The authors reported that Ang-(1-7) infusion led to NF-κB activation and inflammation via Mas. In contrast, Kim et al. showed protective effects of Ang-(1-7) infusion in the same model [40] and no aggravation of renal injury produced by kidney ischemia/reperfusion was observed in Mas−/− mice [6]. Moreover, Mas−/− mice were protected from adriamycin-induced renal injury, again confirming the protective actions of the ACE2/Ang-(1-7)/Mas axis of the RAS in the kidney [94]. The discrepancy between the studies remained unresolved, but anti-inflammatory and protective actions of Mas have repeatedly been described also in other organs: Ang-(1-7) protected from intracranial aneurysm only in wild-type but not in Mas−/− mice [73]. Mas deficiency promoted atherosclerosis and autoimmune encephalitis by affecting macrophage polarization and migration [33] and by increasing vascular intima proliferation [2]. The effects on macrophages and other leukocytes were probably also the reason for the higher susceptibility of Mas−/− mice in an endotoxic shock model [65, 96]. Moreover, Mas−/− mice presented aggravated inflammatory pain [16] and allergic pulmonary inflammation [51].
Mas−/− mice are also a model for metabolic syndrome since they developed metabolic abnormalities, such as type 2 diabetes mellitus and dyslipidemia [88], besides their hypertensive phenotype. On the mechanistic level, this was accompanied by decreased PPARγ expression in fat tissue [52] and a change in the relative amounts of α and β cells in pancreatic islets [24]. Ang-(1-7), mainly via Mas, stimulated insulin secretion from β cells [82]. Furthermore, Mas−/− mice developed liver steatosis when bred with ApoE-deficient mice [93] and Mas−/− female mice were more susceptible to obesity-induced hypertension [113]. Ang-(1-7) and Mas were involved in vascular repair, which is deficient in diabetes, and hindlimb ischemia-induced progenitor cell mobilization was absent in Mas−/− mice [103].
In skeletal muscle, Ang-(1-7) and Mas protected from atrophy since Mas−/− mice were more susceptible to a Duchenne muscular dystrophy model (mdx) [1] and to immobilization-induced atrophy [56].
Mas Knockout Rats
Mas knockout rats have been established using Zinc-finger nuclease technology but their phenotype is only partially reported on the Rat Genome Database website (https://rgd.mcw.edu/rgdweb/report/gene/main.html?id=3049).
Mas Overexpression in Retina
Transgenic mice overexpressing Mas in the retina under the control of the opsin promoter developed degeneration of photoreceptors [122]. This surprising phenotype may have been caused by the ligand-independent constitutive activity of Mas [4] causing proliferative effects in cells when the gene is overexpressed.
Ang-(1-7) Models
Transgenic Rats Overexpressing Ang-(1-7)
The group of Timothy Reudelhuber invented a method to express and secrete peptides from an artificial protein without the need of specific proteases in transgenic animals [54, 55]. Using this method, Ang-(1-7) was overexpressed in transgenic rats (TGR(A1-7)3292) using the CMV promoter [28]. These animals mainly expressed the peptide in the testis, which nevertheless significantly increased plasma levels of Ang-(1-7). As a consequence, total peripheral resistance was decreased together with increases in the blood flow to several organs. Nonetheless, the animals remained normotensive, probably since they exhibited an improved pumping function of the heart [11]. These cardiac effects also protected the heart from pressure and ischemia-induced damage [84] as well as from DOCA-induced diastolic dysfunction [19]. A part of these effects may be due to alterations in autonomic regulation observed in these rats [18]. The increased levels of plasma Ang-(1-7) exerted antinatriuretic actions in the kidney resulting in reduced urinary flow and increased urinary osmolality [28]. Furthermore, TGR(A1-7)3292 rats exhibited metabolic improvements such as decreased plasma lipid levels, improved glucose tolerance, less fat tissue, decreased lipogenesis, and less cafeteria-diet-induced obesity [9, 57, 87, 89]. Moreover, these rats presented a reduction in anxiety-like behavior [39] and in the response to stress [60].
Transgenic Mice and Rats Overexpressing Ang-(1-7) in the Heart
We also generated transgenic mice and rats expressing the Ang-(1-7) release protein specifically in the heart using the α cardiac myosin heavy chain promoter. Both lines showed a slightly improved heart function at baseline and were protected from cardiac hypertrophy [27, 54], but, interestingly, not from myocardial infarction [112].
Conclusions
As summarized in this chapter, several genetically altered rat and mouse models have been generated changing the expression of components of the ACE2/Ang-(1-7)/Mas axis of the RAS (Table 1). With the help of these models, physiological and pathophysiological functions of this axis have been elucidated. Nevertheless, novel models are warranted with cell-type-specific deficiency of ACE2 or Mas to further delineate their tissue-specific effects. The already collected findings are the basis for the development of novel therapeutic strategies for cardiovascular and metabolic diseases by targeting ACE2 or Mas [86, 98].
References
Acuna MJ, Pessina P, Olguin H, Cabrera D, Vio CP, Bader M, Munoz-Canoves P, Santos RA, Cabello-Verrugio C, Brandan E. Restoration of muscle strength in dystrophic muscle by angiotensin-1-7 through inhibition of TGF-beta signalling. Hum Mol Genet. 2014;23:1237–49.
Alsaadon H, Kruzliak P, Smardencas A, Hayes A, Bader M, Angus P, Herath C, Zulli A. Increased aortic intimal proliferation due to MasR deletion in vitro. Int J Exp Pathol. 2015;96:183.
Bader M. Rat models of cardiovascular diseases. Methods Mol Biol. 2010;597:403–14.
Bader M, Alenina N, Andrade-Navarro MA, and Santos RA. Mas and its related G protein-coupled receptors. Pharmacol Rev. 2014;66:1080–105.
Bader M, Bohnemeier H, Zollmann FS, Lockley-Jones OE, Ganten D. Transgenic animals in cardiovascular disease research. Exp Physiol. 2000;85:713–31.
Barroso LC, Silveira KD, Lima CX, Borges V, Bader M, Rachid M, Santos RA, Souza DG. Simoes e Silva AC, and Teixeira MM. Renoprotective effects of AVE0991, a nonpeptide Mas receptor agonist, in experimental acute renal injury. Int. J Hypertens. 2012;2012:808726.
Bernardi S, Tikellis C, Candido R, Tsorotes D, Pickering RJ, Bossi F, Carretta R, Fabris B, Cooper ME, Thomas MC. ACE2 deficiency shifts energy metabolism towards glucose utilization. Metabolism. 2015;64:406–15.
Bharadwaj MS, Strawn WB, Groban L, Yamaleyeva LM, Chappell MC, Horta C, Atkins K, Firmes L, Gurley SB, Brosnihan KB. Angiotensin-converting enzyme 2 deficiency is associated with impaired gestational weight gain and fetal growth restriction. Hypertension. 2011;58:852–8.
Bilman V, Mares-Guia L, Nadu AP, Bader M, Campagnole-Santos MJ, Santos RA, Santos SH. Decreased hepatic gluconeogenesis in transgenic rats with increased circulating angiotensin-(1-7). Peptides. 2012;37:247–51.
Botelho-Santos GA, Bader M, Alenina N, Santos RA. Altered regional blood flow distribution in Mas-deficient mice. Ther Adv Cardiovasc Dis. 2012;6:201–11.
Botelho-Santos GA, Sampaio WO, Reudelhuber TL, Bader M, Campagnole-Santos MJ, Santos RA. Expression of an angiotensin-(1-7)-producing fusion protein in rats induced marked changes in regional vascular resistance. Am J Phys. 2007;292:H2485–90.
Cao X, Yang FY, Xin Z, Xie RR, Yang JK. The ACE2/Ang-(1-7)/Mas axis can inhibit hepatic insulin resistance. Mol Cell Endocrinol. 2014;393:30–8.
Castro CH, Santos RA, Ferreira AJ, Bader M, Alenina N, Almeida AP. Effects of genetic deletion of angiotensin-(1-7) receptor Mas on cardiac function during ischemia/reperfusion in the isolated perfused mouse heart. Life Sci. 2006;80:264–8.
Chen J, Zhao Y, Chen S, Wang J, Xiao X, Ma X, Penchikala M, Xia H, Lazartigues E, Zhao B, Chen Y. Neuronal over-expression of ACE2 protects brain from ischemia-induced damage. Neuropharmacology. 2014;79:550–8.
Chodavarapu H, Chhabra KH, Xia H, Shenoy V, Yue X, Lazartigues E. High-fat diet-induced glucose dysregulation is independent of changes in islet ACE2 in mice. Am J Physiol Regul Integr Comp Physiol. 2016;311:R1223–33.
Costa AC, Romero TR, Pacheco DF, Perez AC, Savernini A, Santos RR, Duarte ID. Participation of AT1 and Mas receptors in the modulation of inflammatory pain. Peptides. 2014;61:17–22.
Crackower MA, Sarao R, Oudit GY, Yagil C, Kozieradzki I, Scanga SE, Oliveira-dos-Santos AJ, da Costa J, Zhang L, Pei Y, Scholey J, Ferrario CM, Manoukian AS, Chappell MC, Backx PH, Yagil Y, Penninger JM. Angiotensin-converting enzyme 2 is an essential regulator of heart function. Nature. 2002;417:822–8.
Dartora DR, Irigoyen MC, Casali KR, Moraes-Silva IC, Bertagnolli M, Bader M, Santos RAS. Improved cardiovascular autonomic modulation in transgenic rats expressing an Ang-(1-7)-producing fusion protein. Can J Physiol Pharmacol. 2017;95:993–8.
de Almeida PW, Melo MB, Lima RF, Gavioli M, Santiago NM, Greco L, Jesus IC, Nocchi E, Parreira A, Alves MN, Mitraud L, Resende RR, Campagnole-Santos MJ, Dos Santos RA, Guatimosim S. Beneficial effects of angiotensin-(1-7) against deoxycorticosterone acetate-induced diastolic dysfunction occur independently of changes in blood pressure. Hypertension. 2015;66:389–95.
Dickinson ME, Flenniken AM, Ji X, Teboul L, Wong MD, White JK, Meehan TF, Weninger WJ, Westerberg H, Adissu H, Baker CN, Bower L, Brown JM, Caddle LB, Chiani F, Clary D, Cleak J, Daly MJ, Denegre JM, Doe B, Dolan ME, Edie SM, Fuchs H, Gailus-Durner V, Galli A, Gambadoro A, Gallegos J, Guo S, Horner NR, Hsu CW, Johnson SJ, Kalaga S, Keith LC, Lanoue L, Lawson TN, Lek M, Mark M, Marschall S, Mason J, ML ME, Newbigging S, Nutter LM, Peterson KA, Ramirez-Solis R, Rowland DJ, Ryder E, Samocha KE, Seavitt JR, Selloum M, Szoke-Kovacs Z, Tamura M, Trainor AG, Tudose I, Wakana S, Warren J, Wendling O, West DB, Wong L, Yoshiki A, MacArthur DG, Tocchini-Valentini GP, Gao X, Flicek P, Bradley A, Skarnes WC, Justice MJ, Parkinson HE, Moore M, Wells S, Braun RE, Svenson KL, de Angelis MH, Herault Y, Mohun T, Mallon AM, Henkelman RM, Brown SD, Adams DJ, Lloyd KC, McKerlie C, Beaudet AL, Bucan M, Murray SA. High-throughput discovery of novel developmental phenotypes. Nature. 2016;537:508–14.
Donoghue M, Wakimoto H, Maguire CT, Acton S, Hales P, Stagliano N, Fairchild-Huntress V, Xu J, Lorenz JN, Kadambi V, Berul CI, Breitbart RE. Heart block, ventricular tachycardia, and sudden death in ACE2 transgenic mice with downregulated connexins. J Mol Cell Cardiol. 2003;35:1043–53.
Esteban V, Heringer-Walther S, Sterner-Kock A, de BR, van den Engel S, Wang Y, Mezzano S, Egido J, Schultheiss HP, Ruiz-Ortega M, Walther T. Angiotensin-(1-7) and the g protein-coupled receptor MAS are key players in renal inflammation. PLoS ONE. 2009;4:e5406.
Fang F, Liu GC, Zhou X, Yang S, Reich HN, Williams V, Hu A, Pan J, Konvalinka A, Oudit GY, Scholey JW, John R. Loss of ACE2 exacerbates murine renal ischemia-reperfusion injury. PLoS One. 2013;8:e71433.
Felix BJ, Ravizzoni DD, Alenina N, Bader M, Santos RA. Glucagon-producing cells are increased in Mas-deficient mice. Endocr Connect. 2017;6:27–32.
Feng Y, Hans C, McIlwain E, Varner KJ, Lazartigues E. Angiotensin-converting enzyme 2 over-expression in the central nervous system reduces angiotensin-II-mediated cardiac hypertrophy. PLoS One. 2012;7:e48910.
Feng Y, Xia H, Cai Y, Halabi CM, Becker LK, Santos RA, Speth RC, Sigmund CD, Lazartigues E. Brain-selective overexpression of human angiotensin-converting enzyme type 2 attenuates neurogenic hypertension. Circ Res. 2010;106:373–82.
Ferreira AJ, Castro CH, Guatimosim S, Almeida PW, Gomes ER, Dias-Peixoto MF, Alves MN, Fagundes-Moura CR, Rentzsch B, Gava E, Almeida AP, Guimaraes AM, Kitten GT, Reudelhuber T, Bader M, Santos RA. Attenuation of isoproterenol-induced cardiac fibrosis in transgenic rats harboring an angiotensin-(1-7)-producing fusion protein in the heart. Ther Adv Cardiovasc Dis. 2010;4:83–96.
Ferreira AJ, Pinheiro SVB, Castro CH, Silva GAB, Simoes e Silva AC, Almeida AP, Bader M, Rentzsch B, Reudelhuber TL, Santos RA. Renal functions in transgenic rats expressing an angiotensin-(1-7)-producing fusion protein. Regul Pept. 2006;137:128–33.
Goncalves ACC, Leite R, Silva RAF, Pinheiro SVB, Sampaio WO, Reis AB, Reis FM, Thouyz RM, Webb R, Alenina N, Bader M, Santos RA. The vasodilator angiotensin-(1-7)-Mas axis plays an essential role in erectile function. Am J Phys. 2007;293:2588–96.
Gu H, Xie Z, Li T, Zhang S, Lai C, Zhu P, Wang K, Han L, Duan Y, Zhao Z, Yang X, Xing L, Zhang P, Wang Z, Li R, Yu JJ, Wang X, Yang P. Angiotensin-converting enzyme 2 inhibits lung injury induced by respiratory syncytial virus. Sci Rep. 2016;6:19840.
Gurley SB, Allred A, Le TH, Griffiths R, Mao L, Philip N, Haystead TA, Donoghue M, Breitbart RE, Acton SL, Rockman HA, Coffman TM. Altered blood pressure responses and normal cardiac phenotype in ACE2-null mice. J Clin Invest. 2006;116:2218–25.
Gurley SB, Coffman TM. Angiotensin-converting enzyme 2 gene targeting studies in mice: mixed messages. Exp Physiol. 2008;93:538–42.
Hammer A, Yang G, Friedrich J, Kovacs A, Lee DH, Grave K, Jorg S, Alenina N, Grosch J, Winkler J, Gold R, Bader M, Manzel A, Rump LC, Muller DN, Linker RA, Stegbauer J. Role of the receptor Mas in macrophage-mediated inflammation in vivo. Proc Natl Acad Sci U S A. 2016;113:14109–14.
Hashimoto T, Perlot T, Rehman A, Trichereau J, Ishiguro H, Paolino M, Sigl V, Hanada T, Hanada R, Lipinski S, Wild B, Camargo SM, Singer D, Richter A, Kuba K, Fukamizu A, Schreiber S, Clevers H, Verrey F, Rosenstiel P, Penninger JM. ACE2 links amino acid malnutrition to microbial ecology and intestinal inflammation. Nature. 2012;487:477–81.
Higaki A, Mogi M, Iwanami J, Min LJ, Bai HY, Shan BS, Kukida M, Yamauchi T, Tsukuda K, Kan-No H, Ikeda S, Higaki J, Horiuchi M. Beneficial Effect of Mas Receptor Deficiency on Vascular Cognitive Impairment in the Presence of Angiotensin II Type 2 Receptor. J Am Heart Assoc. 2018;7.
Hung YH, Hsieh WY, Hsieh JS, Liu FC, Tsai CH, Lu LC, Huang CY, Wu CL, Lin CS. Alternative roles of STAT3 and MAPK signaling pathways in the MMPs activation and progression of lung injury induced by cigarette smoke exposure in ACE2 knockout mice. Int J Biol Sci. 2016;12:454–65.
Imai Y, Kuba K, Rao S, Huan Y, Guo F, Guan B, Yang P, Sarao R, Wada T, Leong-Poi H, Crackower MA, Fukamizu A, Hui CC, Hein L, Uhlig S, Slutsky AS, Jiang C, Penninger JM. Angiotensin-converting enzyme 2 protects from severe acute lung failure. Nature. 2005;436:112–6.
Jin HY, Chen LJ, Zhang ZZ, Xu YL, Song B, Xu R, Oudit GY, Gao PJ, Zhu DL, Zhong JC. Deletion of angiotensin-converting enzyme 2 exacerbates renal inflammation and injury in apolipoprotein E-deficient mice through modulation of the nephrin and TNF-alpha-TNFRSF1A signaling. J Transl Med. 2015;13:255.
Kangussu LM, Almeida-Santos AF, Moreira FA, Fontes MAP, Santos RAS, Aguiar DC, Campagnole-Santos MJ. Reduced anxiety-like behavior in transgenic rats with chronically overproduction of angiotensin-(1-7): role of the Mas receptor. Behav Brain Res. 2017;331:193–8.
Kim CS, Kim IJ, Bae EH, Ma SK, Lee J, Kim SW. Angiotensin-(1-7) attenuates kidney injury due to obstructive nephropathy in rats. PLoS One. 2015;10:e0142664.
Kuba K, Zhang L, Imai Y, Arab S, Chen M, Maekawa Y, Leschnik M, Leibbrandt A, Markovic M, Schwaighofer J, Beetz N, Musialek R, Neely GG, Komnenovic V, Kolm U, Metzler B, Ricci R, Hara H, Meixner A, Nghiem M, Chen X, Dawood F, Wong KM, Sarao R, Cukerman E, Kimura A, Hein L, Thalhammer J, Liu PP, Penninger JM. Impaired heart contractility in Apelin gene-deficient mice associated with aging and pressure overload. Circ Res. 2007;101:e32–42.
Lazaroni TL, Bastos CP, Moraes MF, Santos RS, Pereira GS. Angiotensin-(1-7)/Mas axis modulates fear memory and extinction in mice. Neurobiol Learn Mem. 2016;127:27–33.
Lazaroni TL, Raslan AC, Fontes WR, de Oliveira ML, Bader M, Alenina N, Moraes MF, Dos Santos RA, Pereira GS. Angiotensin-(1-7)/Mas axis integrity is required for the expression of object recognition memory. Neurobiol Learn Mem. 2012;97:113–23.
Leonhardt J, Villela DC, Teichmann A, Munter LM, Mayer MC, Mardahl M, Kirsch S, Namsolleck P, Lucht K, Benz V, Alenina N, Daniell N, Horiuchi M, Iwai M, Multhaup G, Schulein R, Bader M, Santos RA, Unger T, Steckelings UM. Evidence for Heterodimerization and functional interaction of the angiotensin type 2 receptor and the receptor MAS. Hypertension. 2017;69:1128–35.
Li W, Moore MJ, Vasilieva N, Sui J, Wong SK, Berne MA, Somasundaran M, Sullivan JL, Luzuriaga K, Greenough TC, Choe H, Farzan M. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature. 2003;426:450–4.
Lin CI, Tsai CH, Sun YL, Hsieh WY, Lin YC, Chen CY, Lin CS. Instillation of particulate matter 2.5 induced acute lung injury and attenuated the injury recovery in ACE2 knockout mice. Int J Biol Sci. 2018;14:253–65.
Liu C, Xiao L, Li F, Zhang H, Li Q, Liu H, Fu S, Li C, Zhang X, Wang J, Staunstrup NH, Li Y, Yang H. Generation of outbred Ace2 knockout mice by RNA transfection of TALENs displaying colitis reminiscent pathophysiology and inflammation. Transgenic Res. 2015;24:433–46.
Liu R, Qi H, Wang J, Wang Y, Cui L, Wen Y, Yin C. Angiotensin-converting enzyme (ACE and ACE2) imbalance correlates with the severity of cerulein-induced acute pancreatitis in mice. Exp Physiol. 2014;99:651–63.
Lovren F, Pan Y, Quan A, Teoh H, Wang G, Shukla PC, Levitt KS, Oudit GY, Al-Omran M, Stewart DJ, Slutsky AS, Peterson MD, Backx PH, Penninger JM, Verma S. Angiotensin converting enzyme-2 confers endothelial protection and attenuates atherosclerosis. Am J Physiol Heart Circ Physiol. 2008;295:H1377–84.
Lu CL, Wang Y, Yuan L, Li Y, Li XY. The angiotensin-converting enzyme 2/angiotensin (1-7)/Mas axis protects the function of pancreatic beta cells by improving the function of islet microvascular endothelial cells. Int J Mol Med. 2014;34:1293–300.
Magalhaes GS, Rodrigues-Machado MD, Motta-Santos D, Alenina N, Bader M, Santos RA, Barcelos LS, Campagnole-Santos MJ. Chronic allergic pulmonary inflammation is aggravated in angiotensin-(1-7) Mas receptor knockout mice. Am J Physiol Lung Cell Mol Physiol ajplung. 2016;311:L1141.
Mario EG, Santos SH, Ferreira AV, Bader M, Santos RA, Botion LM. Angiotensin-(1-7) Mas-receptor deficiency decreases peroxisome proliferator-activated receptor gamma expression in adipocytes. Peptides. 2012;33:174–7.
McCray PB Jr, Pewe L, Wohlford-Lenane C, Hickey M, Manzel L, Shi L, Netland J, Jia HP, Halabi C, Sigmund CD, Meyerholz DK, Kirby P, Look DC, Perlman S. Lethal infection of K18-hACE2 mice infected with severe acute respiratory syndrome coronavirus. J Virol. 2007;81:813–21.
Mercure C, Yogi A, Callera GE, Aranha AB, Bader M, Ferreira AJ, Santos RA, Walther T, Thouyz RM, Reudelhuber TL. Angiotensin 1-7 blunts hypertensive cardiac remodeling by a direct effect on the heart. Circ Res. 2008;103:1319–26.
Methot D, Lapointe MC, Touyz RM, Yang XP, Carretero OA, Deschepper CF, Schiffrin EL, Thibault G, Reudelhuber TL. Tissue targeting of angiotensin peptides. J Biol Chem. 1997;272:12994–9.
Morales MG, Abrigo J, Acuna MJ, Santos RA, Bader M, Brandan E, Simon F, Olguin H, Cabrera D, Cabello-Verrugio C. Angiotensin-(1-7) attenuates disuse skeletal muscle atrophy in mice via its receptor, Mas. Dis Model Mech. 2016;9:441–9.
Moreira CCL, Lourenco FC, Mario EG, Santos RAS, Botion LM, Chaves VE. Long-term effects of angiotensin-(1-7) on lipid metabolism in the adipose tissue and liver. Peptides. 2017;92:16–22.
Mori MAS, Bader M, Pesquero JB. Genetically altered animals in the study of the metabolic functions of peptide hormone systems. Curr Opin Nephrol Hypertens. 2008;17:11–7.
Motta-Santos D, Dos Santos RA, Oliveira M, Qadri F, Poglitsch M, Mosienko V, Kappes BL, Campagnole-Santos MJ, Penninger M, Alenina N, Bader M. Effects of ACE2 deficiency on physical performance and physiological adaptations of cardiac and skeletal muscle to exercise. Hypertens Res. 2016;39:506–12.
Moura SD, Ribeiro MF, Limborco-Filho M, de Oliveira ML, Hamamoto D, Xavier CH, Moreira FA, Santos RA, Campagnole-Santos MJ, Peliky Fontes MA. Chronic overexpression of angiotensin-(1-7) in rats reduces cardiac reactivity to acute stress and dampens anxious behavior. Stress. 2017;20:189–96.
Nadarajah R, Milagres R, Dilauro M, Gutsol A, Xiao F, Zimpelmann J, Kennedy C, Wysocki J, Batlle D, Burns KD. Podocyte-specific overexpression of human angiotensin-converting enzyme 2 attenuates diabetic nephropathy in mice. Kidney Int. 2012;82:292–303.
Netland J, Meyerholz DK, Moore S, Cassell M, Perlman S. Severe acute respiratory syndrome coronavirus infection causes neuronal death in the absence of encephalitis in mice transgenic for human ACE2. J Virol. 2008;82:7264–75.
Niu MJ, Yang JK, Lin SS, Ji XJ, Guo LM. Loss of angiotensin-converting enzyme 2 leads to impaired glucose homeostasis in mice. Endocrine. 2008;34:56–61.
Nunes-Souza V, Alenina N, Qadri F, Penninger JM, Santos RA, Bader M, Rabelo LA. CD36/Sirtuin 1 Axis impairment contributes to hepatic steatosis in ACE2-deficient mice. Oxidative Med Cell Longev. 2016;2016:6487509.
Oliveira-Lima OC, Pinto MC, Duchene J, Qadri F, Souza LL, Alenina N, Bader M, Santos RA, Carvalho-Tavares J. Mas receptor deficiency exacerbates lipopolysaccharide-induced cerebral and systemic inflammation in mice. Immunobiology. 2015;220:1311–21.
Osterreicher CH, Taura K, De MS, Seki E, Penz-Osterreicher M, Kodama Y, Kluwe J, Schuster M, Oudit GY, Penninger JM, Brenner DA. Angiotensin-converting-enzyme 2 inhibits liver fibrosis in mice. Hepatology (Baltimore, Md). 2009;50:929–38.
Oudit GY, Herzenberg AM, Kassiri Z, Wong D, Reich H, Khokha R, Crackower MA, Backx PH, Penninger JM, Scholey JW. Loss of angiotensin-converting enzyme-2 leads to the late development of angiotensin II-dependent glomerulosclerosis. Am J Pathol. 2006;168:1808–20.
Oudit GY, Kassiri Z, Patel MP, Chappell M, Butany J, Backx PH, Tsushima RG, Scholey JW, Khokha R, Penninger JM. Angiotensin II-mediated oxidative stress and inflammation mediate the age-dependent cardiomyopathy in ACE2 null mice. Cardiovasc Res. 2007;75:29–39.
Patel VB, Bodiga S, Fan D, Das SK, Wang Z, Wang W, Basu R, Zhong J, Kassiri Z, Oudit GY. Cardioprotective effects mediated by angiotensin II type 1 receptor blockade and enhancing angiotensin 1-7 in experimental heart failure in angiotensin-converting enzyme 2-null mice. Hypertension. 2012;59:1195–203.
Patel VB, Mori J, McLean BA, Basu R, Das SK, Ramprasath T, Parajuli N, Penninger JM, Grant MB, Lopaschuk GD, Oudit GY. ACE2 deficiency worsens Epicardial adipose tissue inflammation and cardiac dysfunction in response to diet-induced obesity. Diabetes. 2016;65:85–95.
Patel VB, Zhong JC, Fan D, Basu R, Morton JS, Parajuli N, McMurtry MS, Davidge ST, Kassiri Z, Oudit GY. Angiotensin-converting enzyme 2 is a critical determinant of angiotensin II-induced loss of vascular smooth muscle cells and adverse vascular remodeling. Hypertension. 2014;64:157–64.
Peiro C, Vallejo S, Gembardt F, Azcutia V, Heringer-Walther S, Rodriguez-Manas L, Schultheiss HP, Sanchez-Ferrer CF, Walther T. Endothelial dysfunction through genetic deletion or inhibition of the G protein-coupled receptor Mas: a new target to improve endothelial function. J Hypertens. 2007;25:2421–5.
Pena Silva RA, Kung DK, Mitchell IJ, Alenina N, Bader M, Santos RA, Faraci FM, Heistad DD, Hasan DM. Angiotensin 1-7 reduces mortality and rupture of intracranial aneurysms in mice. Hypertension. 2014;64:362–8.
Pinheiro SVB, Ferreira AJ, Kitten GT, da Silveira KD, da Silva DA, Santos SHS, Gava E, Castro CH, Magalhaes JA, da Mota RK, Botelho-Santos GA, Bader M, Alenina N, Santos RA, Simoes e Silva AC. Genetic deletion of the angiotensin(1-7) receptor Mas leads to glomerular hyperfiltration and microalbuminuria. Kidney Int. 2009;75:1184–93.
Qi YF, Zhang J, Wang L, Shenoy V, Krause E, Oh SP, Pepine CJ, Katovich MJ, Raizada MK. Angiotensin-converting enzyme 2 inhibits high-mobility group box 1 and attenuates cardiac dysfunction post-myocardial ischemia. J Mol Med (Berl). 2016;94:37–49.
Rabello CK, Ravizzoni DD, Moura M, Bertagnolli M, Bader M, Haibara A, Alenina N, Irigoyen MC, Santos RA. Increased vascular sympathetic modulation in mice with Mas receptor deficiency. J Renin-Angiotensin-Aldosterone Syst. 2016;17:1470320316643643.
Rabelo LA, Todiras M, Nunes-Souza V, Qadri F, Szijarto IA, Gollasch M, Penninger JM, Bader M, Santos RA, Alenina N. Genetic deletion of ACE2 induces vascular dysfunction in C57BL/6 mice: role of nitric oxide imbalance and oxidative stress. PLoS One. 2016;11:e0150255.
Rabelo LA, Xu P, Todiras M, Sampaio WO, Buttgereit J, Bader M, Santos RA, Alenina N. Ablation of angiotensin (1-7) receptor Mas in C57Bl/6 mice causes endothelial dysfunction. J Am Soc Hypertens. 2008;2:418–24.
Rentzsch B, Todiras M, Iliescu R, Popova E, Campos LA, Oliveira ML, Baltatu OC, Santos RA, Bader M. Transgenic ACE2 overexpression in vessels of SHRSP rats reduces blood pressure and improves endothelial function. Hypertension. 2008;52:967–73.
Rey-Parra GJ, Vadivel A, Coltan L, Hall A, Eaton F, Schuster M, Loibner H, Penninger JM, Kassiri Z, Oudit GY, Thebaud B. Angiotensin converting enzyme 2 abrogates bleomycin-induced lung injury. J Mol Med (Berl). 2012;90:637.
Sahara M, Ikutomi M, Morita T, Minami Y, Nakajima T, Hirata Y, Nagai R, Sata M. Deletion of angiotensin-converting enzyme 2 promotes the development of atherosclerosis and arterial neointima formation. Cardiovasc Res. 2014;101:236–46.
Sahr A, Wolke C, Maczewsky J, Krippeit-Drews P, Tetzner A, Drews G, Venz S, Gurtler S, van den Brandt J, Berg S, Doring P, Dombrowski F, Walther T, Lendeckel U. The angiotensin-(1-7)/Mas Axis improves pancreatic beta-cell function in vitro and in vivo. Endocrinology. 2016;157:4677–90.
Santos RA, Castro CH, Gava E, Pinheiro SVB, Almeida AP, Paula DR, Cruz JS, Ramos AS, Rosa KT, Irigoyen MC, Bader M, Alenina N, Ferreira AJ. Impairment of in vitro and in vivo heart function in angiotensin-(1-7) receptor Mas knockout mice. Hypertension. 2006;47:996–1002.
Santos RA, Ferreira AJ, Nadu AP, Braga AN, Almeida AP, Campagnole-Santos MJ, Baltatu O, Iliescu R, Reudelhuber TL, Bader M. Expression of an angiotensin-(1-7)-producing fusion protein produces cardioprotective effects in rats. Physiol Genomics. 2004;17:292–9.
Santos RA, Simoes e Silva AC, Maric C, DMR S, Machado RP, de Buhr I, Heringer-Walther S, SVB P, Lopes MT, Bader M, Mendes EP, Lemos VS, Campagnole-Santos MJ, Schultheiss HP, Speth R, Walther T. Angiotensin-(1-7) is an endogenous ligand for the G-protein coupled receptor Mas. Proc Natl Acad Sci U S A. 2003;100:8258–63.
Santos RAS, Sampaio WO, Alzamora AC, Motta-Santos D, Alenina N, Bader M, Campagnole-Santos MJ. The ACE2/angiotensin-(1-7)/MAS Axis of the renin-angiotensin system: focus on angiotensin-(1-7). Physiol Rev. 2018;98:505–53.
Santos SHS, Braga JF, Mario EG, Porto LCJ, Botion LM, Alenina N, Bader M, Santos RA. Improved lipid and glucose metabolism in transgenic rats with increased circulating angiotensin-(1-7). Arterioscler Thromb Vasc Biol. 2010;30:953–61.
Santos SHS, Fernandes LR, Mario EG, Ferreira AVM, Porto LCJ, Alvarez-Leite JI, Botion LM, Bader M, Alenina N, Santos RA. Mas deficiency in FVB/N in mice produces marked changes in lipid and glycemic metabolism. Diabetes. 2008;57:340–7.
Schuchard J, Winkler M, Stolting I, Schuster F, Vogt FM, Barkhausen J, Thorns C, Santos RA, Bader M, Raasch W. Lack of weight gain after angiotensin AT1 receptor blockade in diet-induced obesity is partly mediated by an angiotensin-(1-7)/Mas-dependent pathway. Br J Pharmacol. 2015;172:3764–78.
Shi TT, Yang FY, Liu C, Cao X, Lu J, Zhang XL, Yuan MX, Chen C, Yang JK. Angiotensin-converting enzyme 2 regulates mitochondrial function in pancreatic beta-cells. Biochem Biophys Res Commun. 2018;495:860–6.
Shiota A, Yamamoto K, Ohishi M, Tatara Y, Ohnishi M, Maekawa Y, Iwamoto Y, Takeda M, Rakugi H. Loss of ACE2 accelerates time-dependent glomerular and tubulointerstitial damage in streptozotocin-induced diabetic mice. Hypertens Res. 2010;33:298–307.
Shoemaker R, Yiannikouris F, Thatcher S, Cassis L. ACE2 deficiency reduces beta-cell mass and impairs beta-cell proliferation in obese C57BL/6 mice. Am J Physiol Endocrinol Metab. 2015;309:E621–31.
Silva AR, Aguilar EC, Alvarez-Leite JI, da Silva RF, Arantes RM, Bader M, Alenina N, Pelli G, Lenglet S, Galan K, Montecucco F, Mach F, Santos SH, Santos RA. Mas receptor deficiency is associated with worsening of lipid profile and severe hepatic steatosis in ApoE knockout mice. Am J Physiol Regul Integr Comp Physiol. 2013;305:R1323–30.
Silveira KD, Barroso LC, Vieira AT, Cisalpino D, Lima CX, Bader M, Arantes RM, Dos Santos RA, Simoes-E-Silva AC, Teixeira MM. Beneficial effects of the activation of the Angiotensin-(1-7) MAS receptor in a murine model of adriamycin-induced nephropathy. PLoS One. 2013;8:e66082.
Singer D, Camargo SM, Ramadan T, Schafer M, Mariotta L, Herzog B, Huggel K, Wolfer D, Werner S, Penninger JM, Verrey F. Defective intestinal amino acid absorption in Ace2 null mice. Am J Physiol Gastrointest Liver Physiol. 2012;303:G686–95.
Souza LL, Duchene J, Todiras M, Azevedo LCP, Costa-Neto CM, Alenina N, Santos RA, Bader M. Receptor Mas protects mice against hypothermia and mortality induced by endotoxemia. Shock. 2014;41:331–6.
Sriramula S, Xia H, Xu P, Lazartigues E. Brain-targeted angiotensin-converting enzyme 2 overexpression attenuates neurogenic hypertension by inhibiting cyclooxygenase-mediated inflammation. Hypertension. 2015;65:577–86.
Steckelings UM, Paulis L, Unger T, Bader M. Emerging drugs which target the renin-angiotensin-aldosterone system. Expert Opin Emerg Drugs. 2011;16:619–30.
Thatcher SE, Zhang X, Howatt DA, Yiannikouris F, Gurley SB, Ennis T, Curci JA, Daugherty A, Cassis LA. Angiotensin-converting enzyme 2 decreases formation and severity of angiotensin II-induced abdominal aortic aneurysms. Arterioscler Thromb Vasc Biol. 2014;34:2617–23.
Thomas MC, Pickering RJ, Tsorotes D, Koitka A, Sheehy K, Bernardi S, Toffoli B, Nguyen-Huu TP, Head GA, Fu Y, Chin-Dusting J, Cooper ME, Tikellis C. Genetic Ace2 deficiency accentuates vascular inflammation and atherosclerosis in the ApoE knockout mouse. Circ Res. 2010;107:888–97.
Tikellis C, Brown R, Head GA, Cooper ME, Thomas MC. Angiotensin-converting enzyme 2 mediates hyperfiltration associated with diabetes. Am J Physiol Renal Physiol. 2014;306:F773–80.
Tseng CT, Huang C, Newman P, Wang N, Narayanan K, Watts DM, Makino S, Packard MM, Zaki SR, Chan TS, Peters CJ. Severe acute respiratory syndrome coronavirus infection of mice transgenic for the human angiotensin-converting enzyme 2 virus receptor. J Virol. 2007;81:1162–73.
Vasam G, Joshi S, Thatcher SE, Bartelmez SH, Cassis LA, Jarajapu YP. Reversal of bone marrow Mobilopathy and enhanced vascular repair by Angiotensin-(1-7) in diabetes. Diabetes. 2017;66:505–18.
Vickers C, Hales P, Kaushik V, Dick L, Gavin J, Tang J, Godbout K, Parsons T, Baronas E, Hsieh F, Acton S, Patane M, Nichols A, Tummino P. Hydrolysis of biological peptides by human angiotensin-converting enzyme-related carboxypeptidase. J Biol Chem. 2002;277:14838–43.
Walther T, Balschun D, Voigt JP, Fink H, Zuschratter W, Birchmeier C, Ganten D, Bader M. Sustained long term potentiation and anxiety in mice lacking the Mas protooncogene. J Biol Chem. 1998;273:11867–73.
Walther T, Voigt JP, Fink H, Bader M. Sex specific behavioural alterations in Mas-deficient mice. Behav Brain Res. 2000;107:105–9.
Wang L, de Kloet AD, Pati D, Hiller H, Smith JA, Pioquinto DJ, Ludin JA, Oh SP, Katovich MJ, Frazier CJ, Raizada MK, Krause EG. Increasing brain angiotensin converting enzyme 2 activity decreases anxiety-like behavior in male mice by activating central Mas receptors. Neuropharmacology. 2016;105:114–23.
Wang LA, de Kloet AD, Smeltzer MD, Cahill KM, Hiller H, Bruce EB, Pioquinto DJ, Ludin JA, Katovich MJ, Raizada MK, Krause EG. Coupling corticotropin-releasing-hormone and angiotensin converting enzyme 2 dampens stress responsiveness in male mice. Neuropharmacology. 2018;133:85–93.
Wang LP, Fan SJ, Li SM, Wang XJ, Gao JL, Yang XH. Protective role of ACE2-Ang-(1-7)-Mas in myocardial fibrosis by downregulating KCa3.1 channel via ERK1/2 pathway. Pflugers Arch. 2016;468:2041–51.
Wang W, McKinnie SM, Farhan M, Paul M, McDonald T, McLean B, Llorens-Cortes C, Hazra S, Murray AG, Vederas JC, Oudit GY. Angiotensin-converting enzyme 2 metabolizes and partially inactivates Pyr-Apelin-13 and Apelin-17: physiological effects in the cardiovascular system. Hypertension. 2016;68:365–77.
Wang XL, Iwanami J, Min LJ, Tsukuda K, Nakaoka H, Bai HY, Shan BS, Kan-No H, Kukida M, Chisaka T, Yamauchi T, Higaki A, Mogi M, Horiuchi M. Deficiency of angiotensin-converting enzyme 2 causes deterioration of cognitive function. NPJ Aging Mech Dis. 2016;2:16024.
Wang Y, Qian C, Roks AJ, Westermann D, Schumacher SM, Escher F, Schoemaker RG, Reudelhuber TL, Van Gilst WH, Schultheiss HP, Tschope C, Walther T. Circulating rather than cardiac angiotensin-(1-7) stimulates cardioprotection after myocardial infarction. Circ Heart Fail. 2010;3:286–93.
Wang Y, Shoemaker R, Powell D, Su W, Thatcher S, Cassis L. Differential effects of Mas receptor deficiency on cardiac function and blood pressure in obese male and female mice. Am J Physiol Heart Circ Physiol. 2017;312:H459–68.
Wang Y, Shoemaker R, Thatcher SE, Batifoulier-Yiannikouris F, English VL, Cassis LA. Administration of 17beta-estradiol to ovariectomized obese female mice reverses obesity-hypertension through an ACE2-dependent mechanism. Am J Physiol Endocrinol Metab. 2015;308:E1066–75.
Wong DW, Oudit GY, Reich H, Kassiri Z, Zhou J, Liu QC, Backx PH, Penninger JM, Herzenberg AM, Scholey JW. Loss of angiotensin-converting enzyme-2 (Ace2) accelerates diabetic kidney injury. Am J Pathol. 2007;171:438–51.
Wysocki J, Ortiz-Melo DI, Mattocks NK, Xu K, Prescott J, Evora K, Ye M, Sparks MA, Haque SK, Batlle D, Gurley SB. ACE2 deficiency increases NADPH-mediated oxidative stress in the kidney. Physiol Rep. 2014;2:e00264.
Xia H, de Queiroz TM, Sriramula S, Feng Y, Johnson T, Mungrue IN, Lazartigues E. Brain ACE2 overexpression reduces DOCA-salt hypertension independently of endoplasmic reticulum stress. Am J Physiol Regul Integr Comp Physiol. 2015;308:R370–8.
Xia H, Sriramula S, Chhabra KH, Lazartigues E. Brain angiotensin-converting enzyme type 2 shedding contributes to the development of neurogenic hypertension. Circ Res. 2013;113:1087–96.
Xia H, Suda S, Bindom S, Feng Y, Gurley SB, Seth D, Navar LG, Lazartigues E. ACE2-mediated reduction of oxidative stress in the central nervous system is associated with improvement of autonomic function. PLoS One. 2011;6:e22682.
Xiao L, Gao L, Lazartigues E, Zucker IH. Brain-selective overexpression of angiotensin-converting enzyme 2 attenuates sympathetic nerve activity and enhances baroreflex function in chronic heart failure. Hypertension. 2011;58:1057–65.
Xu P, Goncalves ACC, Todiras M, Rabelo LA, Sampaio WO, Moura MM, Santos SS, Luft FC, Bader M, Gross V, Alenina N, Santos RA. Endothelial dysfunction and elevated blood pressure in Mas gene-deleted mice. Hypertension. 2008;51:574–80.
Xu X, Quiambao AB, Roveri L, Pardue MT, Marx JL, Rohlich P, Peachey NS, Al Ubaidi MR. Degeneration of cone photoreceptors induced by expression of the Mas1 protooncogene. Exp Neurol. 2000;163:207–19.
Xuan X, Gao F, Ma X, Huang C, Wang Y, Deng H, Wang S, Li W, Yuan L. Activation of ACE2/angiotensin (1-7) attenuates pancreatic beta cell dedifferentiation in a high-fat-diet mouse model. Metabolism. 2018;81:83–96.
Yamaleyeva LM, Pulgar VM, Lindsey SH, Yamane L, Varagic J, McGee C, da Silva M, Lopes BP, Gurley SB, Brosnihan KB. Uterine artery dysfunction in pregnant ACE2 knockout mice is associated with placental hypoxia and reduced umbilical blood flow velocity. Am J Physiol Endocrinol Metab. 2015;309:E84–94.
Yamamoto K, Ohishi M, Katsuya T, Ito N, Ikushima M, Kaibe M, Tatara Y, Shiota A, Sugano S, Takeda S, Rakugi H, Ogihara T. Deletion of angiotensin-converting enzyme 2 accelerates pressure overload-induced cardiac dysfunction by increasing local angiotensin II. Hypertension. 2006;47:718–26.
Yang XH, Deng W, Tong Z, Liu YX, Zhang LF, Zhu H, Gao H, Huang L, Liu YL, Ma CM, Xu YF, Ding MX, Deng HK, Qin C. Mice transgenic for human angiotensin-converting enzyme 2 provide a model for SARS coronavirus infection. Comp Med. 2007;57:450–9.
Yang XH, Wang YH, Wang JJ, Liu YC, Deng W, Qin C, Gao JL, Zhang LY. Role of angiotensin-converting enzyme (ACE and ACE2) imbalance on tourniquet-induced remote kidney injury in a mouse hindlimb ischemia-reperfusion model. Peptides. 2012;36:60–70.
Yoshikawa N, Yoshikawa T, Hill T, Huang C, Watts DM, Makino S, Milligan G, Chan T, Peters CJ, Tseng CT. Differential virological and immunological outcome of severe acute respiratory syndrome coronavirus infection in susceptible and resistant transgenic mice expressing human angiotensin-converting enzyme 2. J Virol. 2009;83:5451–65.
Zhang J, Dong J, Martin M, He M, Gongol B, Marin TL, Chen L, Shi X, Yin Y, Shang F, Wu Y, Huang HY, Zhang J, Zhang Y, Kang J, Moya EA, Huang HD, Powell FL, Chen Z, Thistlethwaite PA, Yuan ZY, Shyy JY. AMPK phosphorylation of ACE2 in endothelium mitigates pulmonary hypertension. Am J Respir Crit Care Med. 2018;198:509.
Zhang ZZ, Cheng YW, Jin HY, Chang Q, Shang QH, Xu YL, Chen LX, Xu R, Song B, Zhong JC. The sirtuin 6 prevents angiotensin II-mediated myocardial fibrosis and injury by targeting AMPK-ACE2 signaling. Oncotarget. 2017;8:72302–14.
Zheng J, Li G, Chen S, Bihl J, Buck J, Zhu Y, Xia H, Lazartigues E, Chen Y, Olson JE. Activation of the ACE2/Ang-(1-7)/Mas pathway reduces oxygen-glucose deprivation-induced tissue swelling, ROS production, and cell death in mouse brain with angiotensin II overproduction. Neuroscience. 2014;273:39–51.
Zheng JL, Li GZ, Chen SZ, Wang JJ, Olson JE, Xia HJ, Lazartigues E, Zhu YL, Chen YF. Angiotensin converting enzyme 2/Ang-(1-7)/Mas axis protects brain from ischemic injury with a tendency of age-dependence. CNS Neurosci Ther. 2014;20:452–9.
Zhong J, Guo D, Chen CB, Wang W, Schuster M, Loibner H, Penninger JM, Scholey JW, Kassiri Z, Oudit GY. Prevention of angiotensin II-mediated renal oxidative stress, inflammation, and fibrosis by angiotensin-converting enzyme 2. Hypertension. 2011;57:314–22.
Zou Z, Yan Y, Shu Y, Gao R, Sun Y, Li X, Ju X, Liang Z, Liu Q, Zhao Y, Guo F, Bai T, Han Z, Zhu J, Zhou H, Huang F, Li C, Lu H, Li N, Li D, Jin N, Penninger JM, Jiang C. Angiotensin-converting enzyme 2 protects from lethal avian influenza a H5N1 infections. Nat Commun. 2014;5:3594.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Alenina, N., Bader, M. (2019). Genetic Models. In: Santos, R. (eds) Angiotensin-(1-7). Springer, Cham. https://doi.org/10.1007/978-3-030-22696-1_3
Download citation
DOI: https://doi.org/10.1007/978-3-030-22696-1_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-22695-4
Online ISBN: 978-3-030-22696-1
eBook Packages: MedicineMedicine (R0)