Abstract
The kappa opioid receptor (KOR) and its endogenous ligands dynorphins (DYN) have been implicated in the development or symptomatology of a variety of neuropsychiatric disorders. This review covers a brief history of the development of KOR agonists and antagonists, their effects in healthy volunteers, and the potential role of DYN/KOR dysfunction in schizophrenia and major depressive disorder from a translational perspective. The potential role of DYN/KOR dysfunction in schizophrenia is based on several lines of evidence. Selective KOR agonists induce affective states in healthy volunteers with similarities to the symptoms of schizophrenia. Studies have shown increased DYN in patients with schizophrenia, although the data have been mixed. Finally, meta-analytic data have shown that opioid antagonists are associated with reductions in the symptoms of schizophrenia. The potential role of DYN/KOR dysfunction in major depressive disorder is also based on a combination of preclinical and clinical data. Selective KOR agonists have shown pro-depressive effects in human volunteers, while selective KOR antagonists have shown robust efficacy in several preclinical models of antidepressant activity. Small studies have shown that nonselective KOR antagonists may have efficacy in treatment-resistant depression. Additionally, recent clinical data have shown that the KOR may be an effective target for treating anhedonia, a finding relevant to both schizophrenia and depression. Finally, recommendations are provided for translating preclinical models for schizophrenia and major depressive disorder into the clinic.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
The kappa opioid receptor (KOR) and its endogenous ligands dynorphins (DYN) (Chavkin and Goldstein 1981; Chavkin et al. 1982) have been implicated in the development or symptomatology of a variety of neuropsychiatric disorders including schizophrenia, depression, anxiety, and substance use disorders (cocaine, alcohol, opiate, and nicotine) (Browne and Lucki 2019; Callaghan et al. 2018; Clark and Abi-Dargham 2019; Jacobson et al. 2020; Koob and Volkow 2010; Li et al. 2016; Lutz and Kieffer 2013; Zhang et al. 2007). Indeed, there is already a large body of supporting clinical evidence for an effect of nonselective KOR antagonists on these disorders although the evidence is mixed. Despite strong preclinical evidence for a therapeutic effect of targeting KORs, there have been a number of failed attempts at translating preclinical models into clinical results and there are currently no United States Food and Drug Administration (FDA) or European Medicines Agency (EMA) approved therapeutics that selectively target the KOR.
In this review I will cover the evidence for involvement of DYN and KOR in two neuropsychiatric disorders: schizophrenia and major depressive disorder (MDD). This review will take a translational perspective and will cover the different clinical successes and failures of targeting the KOR with a focus on potential clinical strategies for translating preclinical evidence into the clinic.
2 KOR Agonists in Preclinical Models and Healthy Volunteers
In preclinical models selective KOR agonists including U50488 (Vonvoigtlander et al. 1983) and U69593 (Lahti et al. 1985) have been shown to produce depressive-like and anxiogenic effects on a number of behavioral screening tests for depression. Historically, it was during the development of new analgesics when the first selective KOR agonists were tested in humans. During this time, the selective KOR agonist spiradoline was also advanced into clinical trials for Parkinson’s disease (Giuffra et al. 1993). Selective KOR agonists were shown to produce negative affective states including cognitive deficits, confusion, dysphoria, anxiety (Pfeiffer et al. 1986), and psychotomimetic side effects that included visual hallucinations, auditory disturbances (hearing real voices as distorted (Walsh et al. 2001)), full auditory hallucinations (hearing voices that were not present (Resnick et al. 1971)), and paranoid delusions of persecution (Walsh et al. 2001). In one notable example, 10 min after an acute injection of the selective KOR agonist enadoline a healthy volunteer became aggressive during a delusion that the staff were attempting to harm him by conspiring to “ruin his mind” (Walsh et al. 2001). These side effects have been reported across a number of clinical trials of synthetic selective KOR agonists including MR 2033/2034 (Pfeiffer et al. 1986), enadoline (Hunter et al. 1990; Reece et al. 1994; Walsh et al. 2001), niravoline (Gadano et al. 2000), bremazocine (Dortch-Carnes and Potter 2005), and spiradoline (Giuffra et al. 1993; Wadenberg 2003). Salvinorin A, a naturally occurring selective KOR agonist isolated from the psychoactive sage plant Salvia divinorum (Roth et al. 2002), produced psychotomimetic effects in both open label (Addy 2012) and double-blind placebo-controlled studies (MacLean et al. 2013; Maqueda et al. 2016). One such study also reported cognitive disruption (difficulty concentrating) (Addy 2012). Additionally, less selective KOR agonist/mu opioid receptor (MOR) antagonists cyclazocine (4.0 mg daily) and ketocyclazocine (0.6–1.2 mg daily) produce cognitive deficits, detachment, and paranoia including multiple reports of feelings of being watched, visual hallucinations which included seeing “monsters,” and auditory hallucinations of voices (Hanlon et al. 1975; Kumor et al. 1986; Resnick et al. 1971).
There are some exceptions to the dysphoric and psychotomimetic effects of KOR agonists in healthy volunteers using low dosages. Fink and colleagues (Fink et al. 1970) described two studies of a range of doses of cyclazocine (0.2–3.0 mg daily) to treat depressive symptoms. In 10 patients with depressive symptoms, cyclazocine produced an antidepressant effect over 3–8 months. In a second group, 19 patients, who had treatment-resistant symptoms of depression from a variety of different primary psychiatric diagnoses, were treated with cyclazocine for 1–34 weeks. Over this time period, 10 patients showed improvements in depressive symptoms although the authors note a narrow therapeutic index. Side effects included dysphoria, visual hallucinations, and auditory hallucinations in some patients (Fink et al. 1970). In most cases the side effects occurred with dosages above 1.4 mg, however, two patients experienced side effects at the lowest dosages.
Additionally, salvinorin A has a long history of medicinal and religious use by the indigenous Mazatec people (Maqueda 2018). Low dose salvinorin A from Salvia divinorum tea has been reported to have an antidepressant effect in a case report (Hanes 2001). Consistent with this, preclinical studies have shown that low dosages of salvinorin A produce anxiolytic effects (Braida et al. 2009) and conditioned place preference in mice (Braida et al. 2008).
2.1 Selective KOR Antagonists
KOR antagonists fit into two categories broadly: long-acting noncompetitive antagonists, also referred to as receptor inactivating, which cause permanent inactivation of the KOR and also activate c-Jun terminal kinase (JNK) (Bruchas et al. 2007; Schattauer et al. 2017); and short-acting competitive antagonists which cause temporary blockade of the KOR and do not activate JNK. One proposed mechanism for their long duration of effect is their very long half-life in the brain (Kishioka et al. 2013; Patkar et al. 2013). However, their effects can be blocked by pretreatment with a rapidly cleared short-acting competitive KOR antagonist indicating that the long duration of effects may not be due to their long half-lives in the brain (Bruchas et al. 2007). Béguin and Cohen (2009) provide a thorough review of the history of KOR antagonist development. Unlike KOR agonists, which exert acute effects within minutes, KOR antagonists have not shown acute effects on baseline mood when administered to healthy volunteers (Reed et al. 2018). Preclinical studies have shown that KOR antagonists do not have inherently rewarding effects as shown by a lack of effect on intracranial self-stimulation (Mague et al. 2003; Todtenkopf et al. 2004).
The first long-acting KOR antagonist, norbinaltorphimine (norBNI) was rationally designed from two naltrexone derived pharmacophores linked with a spacer (Portoghese et al. 1987). It displays unusual pharmacokinetics and KOR blockade. norBNI levels have been shown to last 21 days from a single injection (Horan et al. 1992; Jones and Holtzman 1992; Kishioka et al. 2013; Patkar et al. 2013). NorBNI was never administered to humans although it remains among the most widely used KOR antagonist for preclinical research. Interestingly, one recent study has shown that small dosages approximately 100-fold less than a typical dosage can build up to a cumulative effective dose over a 1-month period of daily administration (Chavkin et al. 2019). As the effects of a full dosage of receptor inactivating KOR antagonists cannot be rapidly reversed, this may represent a safer dosing protocol for antagonists in this class.
The second long acting KOR antagonist, 5′-guanidinonaltrindole (5’-GNTI) was developed as a more potent and selective norBNI derivative (Jones et al. 1998), although it has low bioavailability through oral administration. Its analogue 5′-acetamidinoethylnaltrindole (ANTI) has improved lipophilicity and is orally active (Stevens et al. 2000). 5’-GNTI and ANTI were also never developed beyond use in preclinical models and have not been administered to humans.
Finally, (3R)-7-hydroxy-N-((1S)-1-[[(3R,4R)-4-(3-hydroxyphenyl)-3,4-dimethyl-1-piperidinyl]methyl]-2-methylpropyl)-1,2,3,4-tetrahydro-3-isoquinolinecarboxamide (JDTic), a long acting receptor inactivating small molecule, was developed at the Research Triangle Institute (Thomas et al. 2001). The first selective KOR antagonist to enter the clinic, it also showed unusual pharmacokinetics with a long half-life of ~9 days (Munro et al. 2012). Unfortunately, it was discontinued in phase 1 when two participants exhibited several beats of ventricular tachycardia, a finding that was also observed in non-human primates (Buda et al. 2015). However, questions remained as to whether JDTic was responsible for these effects (Chavkin and Martinez 2015).
JNJ-67953964/LY2456302 (Rorick-Kehn et al. 2014) is the first short-acting selective KOR antagonist to show efficacy in a clinical trial in humans (Krystal et al. 2019). The compound was formerly known as LY2456302, CERC-501, and OpraKappa. Two related compounds, LY2444296 and LY2795050, are in preclinical use, but were not advanced into the clinic (Butelman et al. 2019; Valenza et al. 2017). A second clinical stage short-acting KOR antagonist is BTRX-140 (Guerrero et al. 2019). Other small molecule antagonists include AZ-MTAB, for which development was discontinued due to hERG liability (Brugel et al. 2010), and PF-04455242 (Grimwood et al. 2011), which was discontinued in phase 1 when toxicity issues in preclinical animal models were discovered (Urbano et al. 2014). There are also a number of preclinical short-acting peptide KOR antagonists including zyklophin (Aldrich et al. 2009) and [d-Trp]CJ-15,208 (Eans et al. 2013), a derivative of CJ-15,208 which was discovered by Pfizer Japan from the fungus, Ctenomyces serratus (Saito et al. 2002).
2.2 Nonselective Opioid Antagonists
Naloxone, naltrexone, nalmefene, and buprenorphine are nonselective opioid antagonists that have shown efficacy in a variety of psychiatric conditions in humans. Naloxone, naltrexone, and nalmefene have historically been thought to be pan-opioid antagonists at the KOR, MOR, and delta opioid receptor (DOR), while buprenorphine has been shown to be a KOR antagonist and MOR partial agonist (Toll et al. 1998). However, some studies have shown evidence for partial KOR agonist effects of nalmefene and naltrexone (Butelman et al. 2020). Of note, neither naltrexone nor nalmefene has been shown to produce psychotomimetic effects, indicating that any partial agonism of the KOR is too weak to trigger this mechanism. Importantly, the psychotomimetic effects induced by KOR agonists can be blocked, and rapidly be reversed by treatment with naloxone (Jasinski et al. 1968; Watson et al. 1978) and naltrexone (Maqueda et al. 2016).
3 Therapeutic Targeting of the DYN/KOR System in Schizophrenia
Schizophrenia, a debilitating illness with a prevalence of 0.749% worldwide (Moreno-Kustner et al. 2018), is characterized by positive, negative, and cognitive symptoms. The positive symptoms comprise hallucinations, delusions, and disorganization in speech and behavior, and the negative symptoms comprise flattened affect and social withdrawal. The cognitive symptoms comprise deficits in memory and cognitive function (Association 2013; Nuechterlein et al. 2004).
There are a large number of FDA- and EMA-approved antipsychotics, and a meta-analysis has revealed some variability in efficacy and tolerability (Huhn et al. 2019), however, these only treat the positive symptoms of schizophrenia and there are currently no FDA- or EMA-approved drugs for the treatment of negative or cognitive symptoms. Additionally, approximately 30% of patients do not respond to first line antipsychotic therapy (Kane et al. 1988), representing an enormous unmet medical need.
3.1 Evidence for Abnormal DYN Signaling in Schizophrenia
There is some evidence for disruption of DYN signaling in schizophrenia with at least three studies examining DYN levels, and a number of other studies looking at other opioid peptides in the cerebrospinal fluid (CSF) of patients with schizophrenia. In the first study of DYN levels in schizophrenia, Zhang et al. (1985) measured DYN (type unspecified) in the CSF of 35 first-break medication-free patients with schizophrenia and 35 neurological patients with a wide variety of neurological diseases including tumors. They found that the DYN levels in patients with schizophrenia were significantly lower than the patients with neurological diseases, however this study did not include a healthy control group. In contrast, the second study by Heikkilä et al. (1990) examined DYN A levels from the CSF of 10 unmedicated patients with schizophrenia, 10 patients with other psychiatric conditions, and 10 healthy controls. They found significantly higher DYN A levels in the unmedicated patients with schizophrenia, compared to the healthy control group and a trend effect when compared with the patients with other psychiatric illnesses. The average DYN A levels in the patients with schizophrenia showed a decrease after 1 month of treatment with antipsychotics but this did not reach statistical significance. Interestingly, there was a significant correlation between the level of DYN A and symptoms assessed via the Brief Psychiatric Rating Scale (BPRS) with higher levels of DYN A associated with worse psychopathology. Following this study, Lindtrom (1996) performed a 5-year longitudinal study of 120 patients with schizophrenia. This study measured CSF DYN A levels in medication-free patients upon admission (including 66 patients who had never been treated). After biomarker collection antipsychotic therapy was initiated and patients were followed for 5 years. Outcomes were assessed at 1, 3, and 5 years via the Strauss-Carpenter outcome scale. Lindtrom reported that higher DYN A levels at admission were significantly associated with worse outcomes at 5 years. He also found that negative symptom severity at admission, but not positive symptom severity was also associated with worse 5-year outcomes. Finally, regarding other opioid peptides that have been shown to interact with the KOR (Fricker et al. 2020), a number of studies in the late 1970s have found increased beta-endorphin and other unspecified opioid peptides referred to as “endorphins” in patients with schizophrenia compared to healthy volunteers (Domschke et al. 1979; Lindström et al. 1986; Lindtröm et al. 1978), although the data have been mixed with at least one study finding no differences (Ross et al. 1979).
3.2 Preclinical Evidence from Selective KOR Agonists
As covered previously, in healthy volunteers KOR agonists produce acute psychotomimetic effects including paranoid delusions and auditory hallucinations that have similarities to the positive symptoms of schizophrenia. They also produce negative affective states, including dysphoria and cognitive disruption, which may have similarities to the negative and cognitive symptoms of schizophrenia.
While the positive symptoms of schizophrenia are not clearly able to be modeled in rodents, KOR agonists produce depressive-like symptoms in rodents that may have translational relevance to the negative symptoms of schizophrenia. KOR agonists are aversive to rodents as measured by conditioned place aversion (Bals-Kubik et al. 1993). Acute administration of U50488 (Dogra et al. 2016) or salvinorin A (Butelman et al. 2019) has both been shown to produce depressive-like effects on rodent measures of anhedonia. Further testing with salvinorin A shows that these measures can be reversed by treatment with short-acting KOR antagonists LY2444296 and LY2795050 (Butelman et al. 2019). U69593 has been shown to reduce rewarding effects of positive stimuli as measured by an increase in the intracranial self-stimulation (ICSS) threshold in rats, an effect that can be blocked by KOR antagonist ANTI (Todtenkopf et al. 2004). Selective KOR antagonist JNJ-67953964/LY2456302 has also shown efficacy at reducing anhedonia in patients with clinically significant anhedonia, suggesting a potential role for KOR antagonists in treating anhedonia in the context of the negative symptoms of schizophrenia (Krystal et al. 2019).
Finally, KOR agonists produce disruptions in cognition in both rodents and non-human primates that may have translational relevance to the cognitive symptoms of schizophrenia. Acute administration of U50,488 has been shown to disrupt cognition measured via prepulse inhibition (PPI) (Bortolato et al. 2005), the 5-choice serial reaction time task (5CSRTT) in rats (Shannon et al. 2007), and the differential reinforcement of low response rate task (DRL) in mice (Abraham et al. 2018). Salvinorin A has also been shown to disrupt PPI in mice (Yan et al. 2009). However, one study found that U50,488, U69,593, and salvinorin A did not have any effect on PPI in rats (Tejeda et al. 2010). Additionally, U69593 and GR89,696 (Shannon et al. 2007) and salvinorin A (Braida et al. 2011) have also been shown to disrupt performance on the 5CSRTT in rats. In non-human primates, enadoline causes disruption in cognition measured with the cognitive performance task (Davis et al. 1992). Finally, naltrexone (Shannon et al. 2007) was shown to reverse, and JDTic (Nemeth et al. 2010) and norBNI (Abraham et al. 2018) have all been shown to block the cognitive deficits induced by acute administration of KOR agonists in rodents.
3.3 Treatment with Nonselective Opioid Antagonists Is Significantly Associated with Reductions in the Symptoms of Schizophrenia
To date, there have been more clinical trials of nonselective opioid antagonists for schizophrenia than any other mood disorder, with over 50 clinical trials as well as a number of case reports spanning 4 nonselective opioid antagonists: buprenorphine, nalmefene, naloxone, and naltrexone (Clark et al. 2020). The premise for these studies was based on an initial study performed by Gunne and colleagues in 1977 who reported an acute antipsychotic effect of naloxone injection in 4 out of 6 patients with schizophrenia (Gunne et al. 1977). This high-profile finding set off a number of clinical trials attempting to replicate the results with a variety of different designs, drugs, and clinical endpoints.
The findings from these studies included acute antipsychotic effects reported in short trials and effects on negative symptoms in longer trials. Despite these interesting findings from a relatively large number of trials, many of them had very small sample sizes, and did not contain placebo controls. Overall, approximately half of these trials did not find any significant effect which makes it difficult to derive any definitive results from any individual trial (Clark and Abi-Dargham 2019). To address this, a recent meta-analysis was conducted on the double-blind placebo-controlled trials of opioid antagonists in patients with schizophrenia (Clark et al. 2020). Pooling the trials together resulted in a dataset of 434 patients from 30 trials. When combining the data from the four different opioid antagonists (buprenorphine, nalmefene, naloxone, and naltrexone) they found a significant effect of all drugs combined on the symptoms of schizophrenia combined across all clinical scales (comprising positive, negative, and general). Additionally, a significant effect of all drugs on the positive symptoms (measured by pooling results from scales that only measured positive symptoms such as hallucinations or delusions) was found. Finally, significant effects on hallucinations and delusions individually were found suggesting a potential antipsychotic effect. Unfortunately, there were not enough trials to power the analysis on negative symptoms, and while a large effect size was found using Hedge’s g (Hedges and Olkin 1985) (g = 0.66) it did not reach significance due to underpowering.
Most of the trials assessed (22 out of 30) utilized opioid antagonists as adjunctive therapy which suggests they may have efficacy in this setting. However, a moderator analysis of trials that reported information where chlorpromazine equivalents could be calculated suggested that the effect size was reduced when combined with higher dosages of antipsychotics. Since the average dose was quite high (avg 773 mg per patient) it remains to be seen whether optimal efficacy would be achieved through adjunctive therapy or monotherapy. It is hypothesized that the potential efficacy of nonselective opioid antagonists for treating schizophrenia is due to their ability to reduce signaling through the KOR. However, effects on the MOR and DOR cannot be ruled out and one recent positron emission tomography (PET) study has reported changes in the MOR system in patients with schizophrenia (Ashok et al. 2019).
While this meta-analysis shows a significant association between opioid antagonists and reductions in the symptoms of schizophrenia, definitive conclusions cannot be drawn until opioid antagonists have been trialed in large randomized double-blind placebo-controlled trials.
3.4 Conclusions and Recommendations for Translating Preclinical Findings to the Clinic
Based on the entirety of these data discussed here, there is strong rationale for advancing nonselective opioid antagonists into well-powered randomized double-blind placebo-controlled trials in patients with schizophrenia. However, it is proposed that selective KOR antagonists could be more effective, as off- target effects on the MOR may limit the efficacy of nonselective KOR antagonists in treating the negative symptoms. Future trials will be necessary to examine the appropriate duration of treatment and whether monotherapy or adjunctive therapy with standard of care antipsychotics would be more effective. Many of the clinical trials of nonselective opioid antagonists suggest there may be an acute antipsychotic effect, but due to the mixed data no definitive conclusions can be drawn.
As schizophrenia is a heterogeneous disorder, it is possible that DYN/KOR dysfunction affects a subpopulation of patients who might benefit most from therapeutic targeting of this system. Genetic studies have been limited with one study finding a significant interaction between a polymorphism of pDYN gene and a polymorphism of the dopamine receptor 3 gene DRD3 in 114 patients with schizophrenia compared to 138 healthy controls (Ventriglia et al. 2002). Another study in 250 patients with schizophrenia found a significant association of a pDYN polymorphism with population susceptibility to schizophrenia (Zhang et al. 2004). PET imaging with KOR selective radiotracers may help determine whether there is overactivation of the KOR system in patients with schizophrenia. Additional future studies should also re-examine whether there is elevated DYN in the CSF of patients with schizophrenia as this may provide a potential biomarker.
There are a number of preclinical studies that could provide important translational information. It has been hypothesized that DYN/KOR dysfunction may play a role in the symptoms of schizophrenia through modulating dopamine signaling and potentiating D2 receptor super-sensitivity (Clark and Abi-Dargham 2019). For review of the potential circuitry involved, please see (Shekhar 2019). It would be useful to perform preclinical studies combining KOR antagonists with different standard of care antipsychotics and measure effects on behavior as well as on cortical and striatal dopamine levels via in vivo microdialysis. Additionally, for preclinical modeling of the effects of overactive DYN/KOR, chronic administration of selective KOR agonists may provide a more useful picture of effects on dopamine than studies utilizing a single administration paradigm.
4 Therapeutic Targeting of the DYN/KOR System in Major Depressive Disorder
Major depressive disorder (MDD) is a neuropsychiatric illness with a lifetime prevalence of 20.6% in the USA (Hasin et al. 2018). Approximately 35% of patients experience a recurrent disease course (Eaton et al. 2008). Symptoms defined in the DSM-5 include depressed mood, anhedonia, appetite changes, sleep disturbances, fatigue, and cognitive dysfunction such as problems with memory, psychomotor changes, feelings of worthlessness or excessive guilt, and suicidal ideation or behavior (Association 2013).
Current first line pharmacotherapy is often selective serotonin reuptake inhibitors (SSRIs) (Marcus and Olfson 2010), however SSRIs have a slow onset of action and efficacy is often achieved over several weeks to months (Nierenberg et al. 2000). The DYN/KOR system has been shown to be an attractive target for the treatment of MDD (Browne and Lucki 2019; Callaghan et al. 2018; Jacobson et al. 2020; Li et al. 2016; Lutz and Kieffer 2013; Zhang et al. 2007). Here I will review the clinical and preclinical evidence for potential DYN/KOR dysfunction in MDD from a translational perspective.
4.1 Preclinical Evidence for KOR Antidepressant Activity
As previously mentioned, KOR agonists produce negative affective states in healthy volunteers that may have similarities to the symptoms that occur in MDD. There is also a wealth of preclinical data supporting a potential antidepressant effect of KOR antagonists. Much of the preclinical evidence comes from studies utilizing the forced swim test (FST) developed in rodent models (Porsolt et al. 1977). Both tricyclic and SSRI antidepressants reduce immobility on the FST (Detke et al. 1995).
Consistent with their depressive-like effects in humans, selective KOR agonists increase depressive-like behavior on the FST and reduce time to immobility and total immobility time as shown by U69593 in rats (Mague et al. 2003), U50488 in mice (Dogra et al. 2016), and salvinorin A in rats (Carlezon et al. 2006).
A link between stressful conditions and increased DYN/KOR signaling has been demonstrated as stress via exposure to the FST increases pDYN mRNA levels (Chartoff et al. 2009; Reed et al. 2012). pDYN knock out (KO) mice exposed to the repeated FST do not show increased immobility whereas wild type (WT) mice show increased immobility on repeated exposure (McLaughlin et al. 2003). Rats exposed to the FST, the learned helplessness (LH) model of depression, or immobilization stress showed increased dynorphin A and B in different brain regions including the hippocampus and the nucleus accumbens core (NAc) (Shirayama et al. 2004). DYN signaling may be necessary for negative associations with stressful aversive conditions as norBNI and pDYN KO both blocked conditioned aversion to a neutral odorant cue paired with stress via the FST (Land et al. 2008).
4.2 KOR Antagonists Show Efficacy in the FST Anti-depressant Screening Test
Both long- and short-acting KOR antagonists have been shown to reduce depressive-like behavior in the FST as measured by increased latency to immobility or reduced total immobility time. Studies have shown that intracerebroventricular (ICV) infusion of either norBNI (Mague et al. 2003; Pliakas et al. 2001) or 5’-GNTI (Mague et al. 2003) decreased immobility in the FST in a dose-dependent manner in rats. Additionally, systemic norBNI reduces immobility in the FST in mice (Falcon et al. 2016; Laman-Maharg et al. 2018; McLaughlin et al. 2003) and rats (Reed et al. 2012). Similarly, JDTic reduced immobility at higher dosages tested in the FST in rats; however, in this specific experiment, both norBNI and desipramine had no effect (Beardsley et al. 2005). Systemic ANTI decreases immobility in the FST in rats while systemic 5’-GNTI had no effect likely due to its poor bioavailability (Mague et al. 2003).
Short-acting KOR antagonists have shown similar effects to long-acting KOR antagonists in the FST, suggesting that this paradigm is not dependent on the receptor inactivating effects of long-acting KOR antagonists. PF-04455242 (Grimwood et al. 2011), JNJ-67953964 / LY2456302 (Rorick-Kehn et al. 2014; Wang et al. 2017), LY2444296 (Butelman et al. 2019; Huang et al. 2016a), and LY2795050 (Butelman et al. 2019) all reduce immobility in the FST. Additionally, the reduced time to immobility produced by JNJ-67953964/LY2456302 was shown to be of a similar magnitude to a therapeutic dosage of tricyclic antidepressant imipramine (Rorick-Kehn et al. 2014). Although there are some conflicting data, one study found that LY2444296 did not alter immobility time in the FST in rats (Valenza et al. 2017).
4.3 Other Preclinical Models of Depression and Anxiety
In addition to the robust effects observed in the FST, both competitive and noncompetitive KOR antagonists have shown efficacy in other preclinical models of depression and anxiety. Two tests of anxiety include the elevated plus maze (EPM) (Pellow et al. 1985) and the open field (OF) test (Hall 1934). In the EPM the evidence is mixed. Both short-acting JNJ-67953964/LY2456302 (Wang et al. 2017) and long-acting norBNI (Huang et al. 2016b; Knoll et al. 2007) and JDTic (Knoll et al. 2007) increased entries into the open arms and time spent in the open arms in mice (Wang et al. 2017), while zyklophin had no effect in mice (Huang et al. 2016b) and LY2444296 had no effect in either mice (Huang et al. 2016b) or rats (Valenza et al. 2017). In the novelty-induced hypophagia test of anxiety in mice LY2444296, zyklophin, and norBNI all decreased latency to palatable food consumption in novel, but not training, cages (Huang et al. 2016b). Pretreatment with norBNI and JDTic reduced learned fear in the fear-potentiated startle paradigm (Knoll et al. 2007) and norBNI infusion into hippocampus and NAc reduced escape failure on the LH paradigm (Shirayama et al. 2004). Additionally, both norBNI and pDYN KO blocked conditioned aversion to foot shock (Land et al. 2008).
4.4 Nonselective KOR Antagonists as Antidepressants: Evidence from Buprenorphine and ALKS-5461
Buprenorphine has been hypothesized to exert its antidepressant activity primarily through blocking the KOR. Chronic mild stress induces changes in pDYN mRNA and KOR (Oprk1) mRNA that are normalized with 7 days of buprenorphine (Falcon et al. 2016). Studies in rodent models of WT mice and opioid receptor KO have shown that the antidepressant effects of buprenorphine in the FST and unpredictable chronic mild stress (UCMS) are mediated through the KOR in mice (Falcon et al. 2016). The ability of buprenorphine to reduce measures of anhedonia and anxiety is blocked in KOR KO mice, but not in MOR KO or DOR KO mice. Additionally, buprenorphine did not produce additional antidepressant effects beyond those already achieved by pretreatment with the selective KOR antagonist norBNI. In contrast, pretreatment with MOR antagonist clocinnamox did not affect the antidepressant effects of a dose of buprenorphine indicating that the antidepressant effects of buprenorphine are mediated through the KOR (Falcon et al. 2016).
While these studies suggest that antidepressant activity of buprenorphine may be mediated through the KOR, other preclinical studies have identified some different effects between buprenorphine and selective KOR antagonists. The KOR antagonist DIPPA reduces anxiety-like behaviors in both Wistar Kyoto and Sprague Dawley (SD) rat strains (Carr and Lucki 2010), while buprenorphine reduces immobility in the FST only in the Wistar Kyoto rats, but not SD rats (Browne et al. 2015), suggesting that selective KOR antagonists may have advantages over nonselective KOR antagonists. However, in mice exposed to chronic social defeat as a model for post-traumatic stress disorder (PTSD), 7-day treatment with either buprenorphine or the SSRI fluoxetine reversed social deficits, while JNJ-67953964/LY2456302 had no effect (Browne et al. 2018). However, this finding may be limited to this specific KOR antagonist, or other factors related to the experimental paradigm, since other studies have shown that norBNI (McLaughlin et al. 2006), JDTic (Wells et al. 2017), and PF-04455242 (Grimwood et al. 2011) all reduce stress-like behaviors induced by exposures to chronic social defeat stress.
It is important to consider the antidepressant effects of buprenorphine in humans although the dataset is small. The first trial of 0.2 mg sublingual buprenorphine (Emrich et al. 1982) utilized a double-blind crossover design with a variable time period of 1–2 weeks in 10 patients diagnosed with depression. The symptoms of patients significantly improved on buprenorphine and became worse again during the second placebo period. There were also several open label studies that showed efficacy as an antidepressant (Bodkin et al. 1995; Kosten et al. 1990), including patients with treatment-resistant depression (Karp et al. 2014; Nyhuis et al. 2008).
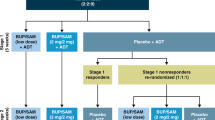
As buprenorphine is a MOR partial agonist, it has potential to form dependence in patients (Lewis 1985). The functional KOR antagonist ALKS 5461, a combination of buprenorphine and the MOR antagonist samidorphan was created to harness the antidepressant potential of buprenorphine without the potential for dependence (Ehrich et al. 2015). ALKS 5461 ultimately completed five trials FORWARD1–5, which have been systematically reviewed (Peckham et al. 2018). While ALKS 5461 initially showed efficacy in phase 2, the large effect size observed in phase 2 did not translate to phase 3. Out of three phase 3 trials, one failed (ClinicalTrials.gov Identifier: NCT02158546), and the effect sizes in the largest phase 3 trial were small (ClinicalTrials.gov Identifier: NCT02218008). Ultimately the FDA rejected the application to approve the drug. However, due to the lack of selectivity for the KOR, limited conclusions can be drawn from ALKS-5461 to the potential efficacy of selective KOR antagonists in MDD.
4.5 KOR Antagonists Treatment of Anhedonia
Anhedonia, the inability to experience pleasure, is a symptom that occurs across multiple psychiatric disorders including MDD and schizophrenia. On two preclinical models of anhedonia, the sucrose preference test and the social interaction test, U50488 increased measures of anhedonia that were resistant to treatment with SSRIs (Dogra et al. 2016). U69,593 increases the ICSS threshold in rats, indicating a reduction in the ability to experience pleasurable stimulation (Todtenkopf et al. 2004). Similarly, salvinorin A has been shown to produce anhedonic effects in mice such as reduced self-grooming, an effect that is reversed by short-acting KOR antagonists LY244296 and LY2795050 (Butelman et al. 2019).
JNJ-67953964/LY2456302 was advanced into the NIMH Fast-Fail Trials in Mood and Anxiety Spectrum Disorders (FAST-MAS) program for the treatment of anhedonia. It was trialed in 89 patients with clinically significant anhedonia measured via the Snaith–Hamilton Pleasure Scale (SHAPS) score. Approximately 80% of the patients had a primary diagnosis of MDD with 20% having other mood disorders. Patients were randomized to either JNJ-67953964/LY2456302 or placebo (Krystal et al. 2019). The primary outcome measure was the mean fMRI ventral striatal activation, an imaging biomarker relevant to anhedonia, measured during a reward anticipation task. The drug produced statistically significant activation of the ventral striatum on fMRI and improved clinical measures of anhedonia measured by a significant reduction on the SHAPS (secondary endpoint). There were no significant effects on the Hamilton Depression Rating Scale (HAM-D) or the Hamilton Anxiety Rating Scale (HAM-A) (exploratory endpoints). Although this was a relatively small trial, the effects on the SHAPS score for anhedonia are consistent with preclinical models predicting efficacy in this symptom domain and support a potential role for KOR antagonists as targeted treatments for anhedonia. Finally, while there were no effects shown on HAM-D, only 80% of patients had major depressive disorder and there was no specified minimum HAM-D score for enrollment, and so no conclusions can be drawn on potential efficacy in MDD from this study.
4.6 KOR Antagonists as Monotherapy vs Adjunctive Therapy
There is evidence that SSRIs and KOR antagonists may exert their antidepressant effects through distinct pathways. In mice, deficits induced by U50488 on preclinical models of anhedonia in the sucrose preference and social interaction tests could be blocked by norBNI and the tricyclic antidepressant imipramine, but not by SSRIs fluoxetine or citalopram, suggesting that KOR agonists induce symptoms of anhedonia that are mediated through different pathways than those acted on by SSRIs (Dogra et al. 2016). Similarly, in one experiment, both norBNI and JDTic reduced anxiety-like behavior on the EPM while SSRIs had no effect, however, SSRIs were found to be effective in the OF model while both norBNI and JDTic had no effect in this paradigm (Knoll et al. 2007). This suggests that SSRIs may modulate different depressive-like and anxiety-like symptomatology than KOR antagonists and that KOR antagonists may help patients who do not fully respond to SSRIs.
Additionally, synergistic antidepressant-like effects were found in the FST in mice when a subtherapeutic dosage of JNJ-67953964/LY2456302 was administered with a subtherapeutic dosage of either SSRI citalopram or the tricyclic antidepressant imipramine (Rorick-Kehn et al. 2014). This suggests the possibility that KOR antagonists may show optimal efficacy when used as adjunctive treatments with current standard of care SSRIs.
KOR antagonists JNJ-67953964/LY2456302 and BTRX-140 are currently being investigated in two ongoing clinical trials in MDD. JNJ-67953964 / LY2456302 is being trialed as an adjunctive treatment for patients who have had an incomplete response to current serotonin-norepinephrine reuptake inhibitor (SNRI) or SSRI therapy. In this case, 10 mg JNJ-67953964/LY2456302, a KOR selective dosage (Rorick-Kehn et al. 2015) that was previously shown on PET imaging to provide 94% occupancy at the KOR at 2.5 h and 72% at 24 h from a single dosage (Naganawa et al. 2016), is added to the patient’s baseline SSRI or SNRI for 6 weeks following a placebo run-in period. The primary endpoint is the change on the Montgomery–Åsberg Depression Rating Scale (MADRS) (ClinicalTrials.gov Identifier: NCT03559192). In contrast, BTRX-140 is being trialed as a monotherapy for 8 weeks with a primary endpoint as the HAM-D (ClinicalTrials.gov Identifier: NCT04221230).
4.7 Sex Differences
One potential issue that may impact the ability to translate preclinical findings to the clinic is the observed sex differences in response to KOR antagonists in rodents. Female rats have been shown to be less sensitive than male rats to the depressive-like effects of KOR agonists (Russell et al. 2014) and female guinea pigs are less sensitive than male guinea pigs to the effects on pain (Wang et al. 2011). One experiment found that the antidepressant effects of norBNI on the FST in two different strains of male mice were not found in females (Laman-Maharg et al. 2018). Interestingly, one PET imaging study of naltrexone in humans reported a higher KOR availability in men than in women (Vijay et al. 2016). Whether any of the sex differences observed in animals will translate humans will need to be addressed in larger trials.
4.8 Conclusions and Recommendations for Translation
The preclinical data reviewed here show that both long- and short-acting KOR antagonists have shown efficacy across a variety of preclinical antidepressant screening tests as monotherapies. Furthermore, they have also been shown to have synergistic efficacy when combined with tricyclic and SSRI antidepressants, suggesting that additional efficacy may be achieved as adjunctive therapies.
While the data with nonselective KOR antagonist buprenorphine are relatively small and many of the studies were open label, significant efficacy was found in treatment-resistant populations, including those resistant to both pharmacotherapy and electroconvulsive therapy (ECT) (Nyhuis et al. 2008). This is consistent with the preclinical data showing that KOR agonists induce depressive-like phenotypes that are resistant to treatment with SSRIs, and it is conceivable that KOR antagonists may represent a potential treatment for patients with treatment-resistant depression. While ALKS 5461 showed mixed results in phase 3 ranging from low effect sizes to lack of effect, this may be due to the MOR antagonist activity of samidorphan.
Finally, KOR antagonists may have specific efficacy on anhedonia, a symptom present in multiple different neuropsychiatric disorders, including MDD and the negative symptoms of schizophrenia. KOR agonists have been shown to induce anhedonic behavioral phenotypes in rodent models that can be reversed by KOR antagonists and this effect has been successfully translated in one trial in humans. The results of ongoing phase 2 trials of KOR antagonists may help answer outstanding questions, such as whether effects on anhedonia will hold up in larger trials, whether there are specific patient populations with DYN/KOR dysfunction, whether efficacy will vary between in men and women, and whether differences will be seen between monotherapy and adjunctive therapy.
References
Abraham AD, Fontaine HM, Song AJ, Andrews MM, Baird MA, Kieffer BL, Land BB, Chavkin C (2018) κ-Opioid receptor activation in dopamine neurons disrupts behavioral inhibition. Neuropsychopharmacology 43:362
Addy PH (2012) Acute and post-acute behavioral and psychological effects of salvinorin a in humans. Psychopharmacology 220:195–204
Aldrich JV, Patkar KA, McLaughlin JP (2009) Zyklophin, a systemically active selective kappa opioid receptor peptide antagonist with short duration of action. Proc Natl Acad Sci U S A 106:18396–18401
Ashok AH, Myers J, Marques TR, Rabiner EA, Howes OD (2019) Reduced mu opioid receptor availability in schizophrenia revealed with [11 C]-carfentanil positron emission tomographic imaging. Nat Commun 10:1–9
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders (DSM-5®), American Psychiatric Publishing
Bals-Kubik R, Ableitner A, Herz A, Shippenberg TS (1993) Neuroanatomical sites mediating the motivational effects of opioids as mapped by the conditioned place preference paradigm in rats. J Pharmacol Exp Ther 264:489–495
Beardsley PM, Howard JL, Shelton KL, Carroll FI (2005) Differential effects of the novel kappa opioid receptor antagonist, JDTic, on reinstatement of cocaine-seeking induced by footshock stressors vs cocaine primes and its antidepressant-like effects in rats. Psychopharmacology 183:118
Bodkin JA, Zornberg GL, Lukas SE, Cole JO (1995) Buprenorphine treatment of refractory depression. J Clin Psychopharmacol 15:49–57
Bortolato M, Aru GN, Frau R, Orrù M, Fà M, Manunta M, Puddu M, Mereu G, Gessa GL (2005) Kappa opioid receptor activation disrupts prepulse inhibition of the acoustic startle in rats. Biol Psychiatry 57:1550–1558
Braida D, Limonta V, Capurro V, Fadda P, Rubino T, Mascia P, Zani A, Gori E, Fratta W, Parolaro D (2008) Involvement of κ-opioid and endocannabinoid system on Salvinorin A-induced reward. Biol Psychiatry 63:286–292
Braida D, Capurro V, Zani A, Rubino T, Viganò D, Parolaro D, Sala M (2009) Potential anxiolytic-and antidepressant-like effects of salvinorin A, the main active ingredient of Salvia divinorum, in rodents. Br J Pharmacol 157:844–853
Braida D, Donzelli A, Martucci R, Capurro V, Sala M (2011) Learning and memory impairment induced by salvinorin A, the principal ingredient of Salvia divinorum, in wistar rats. Int J Toxicol 30:650–661
Browne CA, Lucki I (2019) Targeting opioid dysregulation in depression for the development of novel therapeutics. Pharmacol Ther 201:51–76
Browne CA, van Nest DS, Lucki I (2015) Antidepressant-like effects of buprenorphine in rats are strain dependent. Behav Brain Res 278:385–392
Browne CA, Falcon E, Robinson SA, Berton O, Lucki I (2018) Reversal of stress-induced social interaction deficits by buprenorphine. Int J Neuropsychopharmacol 21:164–174
Bruchas MR, Yang T, Schreiber S, DeFino M, Kwan SC, Li S, Chavkin C (2007) Long-acting κ opioid antagonists disrupt receptor signaling and produce noncompetitive effects by activating c-Jun N-terminal kinase. J Biol Chem 282:29803–29811
Brugel TA, Smith RW, Balestra M, Becker C, Daniels T, Hoerter TN, Koether GM, Throner SR, Panko LM, Folmer JJ (2010) Discovery of 8-azabicyclo [3.2.1] octan-3-yloxy-benzamides as selective antagonists of the kappa opioid receptor. Part 1. Bioorg Med Chem Lett 20:5847–5852
Buda JJ, Carroll FI, Kosten TR, Swearingen D, Walters BB (2015) A double-blind, placebo-controlled trial to evaluate the safety, tolerability, and pharmacokinetics of single, escalating oral doses of JDTic. Neuropsychopharmacology 40:2059–2065
Butelman ER, McElroy BD, Prisinzano TE, Kreek MJ (2019) Impact of pharmacological manipulation of the κ-opioid receptor system on self-grooming and Anhedonic-like behaviors in male mice. J Pharmacol Exp Ther 370:1–8
Butelman ER, Fry RS, Kimani R, Reed B, Kreek MJ (2020) Neuroendocrine effects of naltrexone versus nalmefene in humans. Hum Psychopharmacol 35:e2726
Callaghan CK, Rouine J, O'Mara SM (2018) Potential roles for opioid receptors in motivation and major depressive disorder. Prog Brain Res 239:89–119
Carlezon WA, Béguin C, DiNieri JA, Baumann MH, Richards MR, Todtenkopf MS, Rothman RB, Ma Z, Lee DY-W, Cohen BM (2006) Depressive-like effects of the κ-opioid receptor agonist salvinorin A on behavior and neurochemistry in rats. J Pharmacol Exp Ther 316:440–447
Carr GV, Lucki I (2010) Comparison of the kappa-opioid receptor antagonist DIPPA in tests of anxiety-like behavior between Wistar Kyoto and Sprague Dawley rats. Psychopharmacology 210:295–302
Chartoff EH, Papadopoulou M, MacDonald ML, Parsegian A, Potter D, Konradi C, Carlezon WA (2009) Desipramine reduces stress-activated Dynorphin expression and CREB phosphorylation in NAc tissue. Mol Pharmacol 75:704–712
Chavkin C, Goldstein A (1981) Demonstration of a specific dynorphin receptor in Guinea pig ileum myenteric plexus. Nature 291:591–593
Chavkin C, Martinez D (2015) Kappa antagonist JDTic in phase 1 clinical trial. Neuropsychopharmacology 40:2057–2058
Chavkin C, James IF, Goldstein A (1982) Dynorphin is a specific endogenous ligand of the kappa opioid receptor. Science 215:413–415
Chavkin C, Cohen JH, Land BB (2019) Repeated administration of norbinaltorphimine produces cumulative kappa opioid receptor inactivation. Front Pharmacol 10:88
Clark SD, Abi-Dargham A (2019) The role of dynorphin and the kappa opioid receptor in the symptomatology of schizophrenia: a review of the evidence. Biol Psychiatry 86:502–511
Clark SD, Van Snellenberg JX, Lawson JM, Abi-Dargham A (2020) Opioid antagonists are associated with a reduction in the symptoms of schizophrenia: a meta-analysis of controlled trials. Neuropsychopharmacology:1–12
Davis RE, Callahan MJ, Dickerson M, Downs DA (1992) Pharmacologic activity of CI-977, a selective kappa opioid agonist, in rhesus monkeys. J Pharmacol Exp Ther 261:1044–1049
Detke MJ, Rickels M, Lucki I (1995) Active behaviors in the rat forced swimming test differentially produced by serotonergic and noradrenergic antidepressants. Psychopharmacology 121:66–72
Dogra S, Kumar A, Umrao D, Sahasrabuddhe AA, Yadav PN (2016) Chronic kappa opioid receptor activation modulates NR2B: implication in treatment resistant depression. Sci Rep 6:33401
Domschke W, Dickschas A, Mitznegg P (1979) CSF β-endorphin in schizophrenia. Lancet 313:1024
Dortch-Carnes J, Potter DE (2005) Bremazocine: a κ-opioid agonist with potent analgesic and other pharmacologic properties. CNS Drug Rev 11:195–212
Eans SO, Ganno ML, Reilley KJ, Patkar KA, Senadheera SN, Aldrich JV, McLaughlin JP (2013) The macrocyclic tetrapeptide [D-T rp] CJ-15,208 produces short-acting κ opioid receptor antagonism in the CNS after oral administration. Br J Pharmacol 169:426–436
Eaton WW, Shao H, Nestadt G, Lee BH, Bienvenu OJ, Zandi P (2008) Population-based study of first onset and chronicity in major depressive disorder. Arch Gen Psychiatry 65:513–520
Ehrich E, Turncliff R, Du Y, Leigh-Pemberton R, Fernandez E, Jones R, Fava M (2015) Evaluation of opioid modulation in major depressive disorder. Neuropsychopharmacology 40:1448–1455
Emrich H, Vogt P, Herz A (1982) Possible antidepressive effects of opioids: action of buprenorphine. Ann N Y Acad Sci 398:108–112
Falcon E, Browne CA, Leon RM, Fleites VC, Sweeney R, Kirby LG, Lucki I (2016) Antidepressant-like effects of buprenorphine are mediated by kappa opioid receptors. Neuropsychopharmacology 41:2344–2351
Fink M, Simeon J, Itil TM, Freedman AM (1970) Clinical antidepressant activity of cyclazocine--a narcotic antagonist. Clin Pharmacol Ther 11:41–48
Fricker LD, Margolis EB, Gomes I, Devi LA (2020) Five decades of research on opioid peptides: current knowledge and unanswered questions. Mol Pharmacol 98:96–108
Gadano A, Moreau R, Pessione F, Trombino C, Giuily N, Sinnassamy P, Valla D, Lebrec D (2000) Aquaretic effects of niravoline, a κ-opioid agonist, in patients with cirrhosis. J Hepatol 32:38–42
Giuffra M, Mouradian M, Davis T, Ownby J, Chase T (1993) Dynorphin agonist therapy of Parkinson’s disease. Clin Neuropharmacol 16:444–447
Grimwood S, Lu Y, Schmidt AW, Vanase-Frawley MA, Sawant-Basak A, Miller E, McLean S, Freeman J, Wong S, McLaughlin JP (2011) Pharmacological characterization of 2-methyl-N-((2′-(pyrrolidin-1-ylsulfonyl) biphenyl-4-yl) methyl) propan-1-amine (PF-04455242), a high-affinity antagonist selective for κ-opioid receptors. J Pharmacol Exp Ther 339:555–566
Guerrero M, Urbano M, Kim E-K, Gamo AM, Riley S, Abgaryan L, Leaf N, Van Orden LJ, Brown SJ, Xie JY (2019) Design and synthesis of a novel and selective kappa opioid receptor (KOR) antagonist (BTRX-335140), vol 62. ACS Publications, p 1761
Gunne L-M, Lindström L, Terenius L (1977) Naloxone-induced reversal of schizophrenic hallucinations. J Neural Transm 40:13–19
Hall CS (1934) Emotional behavior in the rat. I. Defecation and urination as measures of individual differences in emotionality. J Comp Psychol 18:385
Hanes KR (2001) Antidepressant effects of the herb Salvia divinorum: a case report. J Clin Psychopharmacol 21:634–635
Hanlon TE, McCabe OL, Savage C, Kurland AA (1975) A controlled comparison of cyclazocine and naloxone treatment of the paroled narcotic addict. Int Pharmacopsychiatry 10:240–250
Hasin DS, Sarvet AL, Meyers JL, Saha TD, Ruan WJ, Stohl M, Grant BF (2018) Epidemiology of adult DSM-5 major depressive disorder and its specifiers in the United States. JAMA Psychiat 75:336–346
Hedges L, Olkin I (1985) Statistical models for meta-analysis. Academic Press, New York
Heikkilä L, Rimón R, Ternius L (1990) Dynorphin A and substance P in the cerebrospinal fluid of schizophrenic patients. Psychiatry Res 34:229–236
Horan P, Taylor J, Yamamura HI, Porreca F (1992) Extremely long-lasting antagonistic actions of nor-binaltorphimine (nor-BNI) in the mouse tail-flick test. J Pharmacol Exp Ther 260:1237–1243
Huang P, Tunis J, Parry C, Tallarida R, Liu-Chen L-Y (2016a) Synergistic antidepressant-like effects between a kappa opioid antagonist (LY2444296) and a delta opioid agonist (ADL5859) in the mouse forced swim test. Eur J Pharmacol 781:53–59
Huang P, Yakovleva T, Aldrich JV, Tunis J, Parry C, Liu-Chen LY (2016b) Two short-acting kappa opioid receptor antagonists (zyklophin and LY2444296) exhibited different behavioral effects from the long-acting antagonist norbinaltorphimine in mouse anxiety tests. Neurosci Lett 615:15–20
Huhn M, Nikolakopoulou A, Schneider-Thoma J, Krause M, Samara M, Peter N, Arndt T, Bäckers L, Rothe P, Cipriani A (2019) Comparative efficacy and tolerability of 32 oral antipsychotics for the acute treatment of adults with multi-episode schizophrenia: a systematic review and network meta-analysis. Lancet 394:939–951
Hunter J, Leighton G, Meecham K, Boyle S, Horwell D, Rees D, Hughes J (1990) CI-977, a novel and selective agonist for the κ-opioid receptor. Br J Pharmacol 101:183–189
Jacobson ML, Browne CA, Lucki I (2020) Kappa opioid receptor antagonists as potential therapeutics for stress-related disorders. Annu Rev Pharmacol Toxicol 60:615–636
Jasinski DR, Martin WR, Sapira JD (1968) Antagonism of the subjective, behavioral, pupillary, and respiratory depressant effects of cyclazocine by naloxone. Clin Pharmacol Ther 9:215–222
Jones DN, Holtzman SG (1992) Long term kappa-opioid receptor blockade following nor-binaltorphimine. Eur J Pharmacol 215:345–348
Jones RM, Hjorth SA, Schwartz TW, Portoghese PS (1998) Mutational evidence for a common κ antagonist binding pocket in the wild-type κ and mutant μ [K303E] opioid receptors. J Med Chem 41:4911–4914
Kane J, Honigfeld G, Singer J, Meltzer H (1988) Clozapine for the treatment-resistant schizophrenic: a double-blind comparison with chlorpromazine. Arch Gen Psychiatry 45:789–796
Karp JF, Butters MA, Begley AE, Miller MD, Lenze EJ, Blumberger DM, Mulsant BH, Reynolds CF 3rd (2014) Safety, tolerability, and clinical effect of low-dose buprenorphine for treatment-resistant depression in midlife and older adults. J Clin Psychiatry 75:e785–e793
Kishioka S, Kiguchi N, Kobayashi Y, Yamamoto C, Saika F, Wakida N, Ko MC, Woods JH (2013) Pharmacokinetic evidence for the long-lasting effect of nor-binaltorphimine, a potent kappa opioid receptor antagonist, in mice. Neurosci Lett 552:98–102
Knoll AT, Meloni EG, Thomas JB, Carroll FI, Carlezon WA (2007) Anxiolytic-like effects of κ-opioid receptor antagonists in models of unlearned and learned fear in rats. J Pharmacol Exp Ther 323:838–845
Koob GF, Volkow ND (2010) Neurocircuitry of addiction. Neuropsychopharmacology 35:1051–1051
Kosten TR, Morgan C, Kosten TA (1990) Depressive symptoms during buprenorphine treatment of opioid abusers. J Subst Abus Treat 7:51–54
Krystal AD, Pizzagalli DA, Mathew SJ, Sanacora G, Keefe R, Song A, Calabrese J, Goddard A, Goodman W, Lisanby SH (2019) The first implementation of the NIMH FAST-FAIL approach to psychiatric drug development. Nat Rev Drug Discov 18:82
Kumor KM, Haertzen CA, Johnson RE, Kocher T, Jasinski D (1986) Human psychopharmacology of ketocyclazocine as compared with cyclazocine, morphine and placebo. J Pharmacol Exp Ther 238:960–968
Lahti RA, Mickelson MM, McCall JM, Von Voigtlander PF (1985) [3H] U-69593 a highly selective ligand for the opioid κ receptor. Eur J Pharmacol 109:281–284
Laman-Maharg A, Williams AV, Zufelt MD, Minie VA, Ramos-Maciel S, Hao R, Ordoñes Sanchez E, Copeland T, Silverman JL, Leigh A (2018) Sex differences in the effects of a kappa opioid receptor antagonist in the forced swim test. Front Pharmacol 9:93
Land BB, Bruchas MR, Lemos JC, Xu M, Melief EJ, Chavkin C (2008) The dysphoric component of stress is encoded by activation of the dynorphin κ-opioid system. J Neurosci 28:407–414
Lewis J (1985) Buprenorphine. Drug Alcohol Depend 14:363–372
Li W, Sun H, Chen H, Yang X, Xiao L, Liu R, Shao L, Qiu Z (2016) Major depressive disorder and kappa opioid receptor antagonists. Trans Perioper Pain Med 1:4
Lindstrom L (1996) Clinical and biological markers for outcome in schizophrenia. Nature Publishing Group
Lindström LH, Besev G, Gunne LM, Terenius L (1986) CSF levels of receptor-active endorphins in schizophrenic patients: correlations with symptomalogy and monoamine metabolites. Psychiatry Res 19:93–100
Lindtröm L, Winderlöv E, Gunne LM, Wahlström A, Terenius L (1978) Endorphins in human cerebrospinal fluid: clinical correlations to some psychotic states. Acta Psychiatr Scand 57:153–164
Lutz P-E, Kieffer BL (2013) Opioid receptors: distinct roles in mood disorders. Trends Neurosci 36:195–206
MacLean KA, Johnson MW, Reissig CJ, Prisinzano TE, Griffiths RR (2013) Dose-related effects of salvinorin A in humans: dissociative, hallucinogenic, and memory effects. Psychopharmacology 226:381–392
Mague SD, Pliakas AM, Todtenkopf MS, Tomasiewicz HC, Zhang Y, Stevens WC, Jones RM, Portoghese PS, Carlezon WA (2003) Antidepressant-like effects of κ-opioid receptor antagonists in the forced swim test in rats. J Pharmacol Exp Ther 305:323–330
Maqueda AE (2018) The use of Salvia divinorum from a Mazatec perspective plant medicines, healing and psychedelic science. Springer, Berlin, pp 55–70
Maqueda AE, Valle M, Addy PH, Antonijoan RM, Puntes M, Coimbra J, Ballester MR, Garrido M, González M, Claramunt J (2016) Naltrexone but not ketanserin antagonizes the subjective, cardiovascular, and neuroendocrine effects of salvinorin-A in humans. Int J Neuropsychopharmacol 19:pyw016
Marcus SC, Olfson M (2010) National trends in the treatment for depression from 1998 to 2007. Arch Gen Psychiatry 67:1265–1273
McLaughlin JP, Marton-Popovici M, Chavkin C (2003) κ opioid receptor antagonism and prodynorphin gene disruption block stress-induced behavioral responses. J Neurosci 23:5674–5683
McLaughlin JP, Li S, Valdez J, Chavkin TA, Chavkin C (2006) Social defeat stress-induced behavioral responses are mediated by the endogenous kappa opioid system. Neuropsychopharmacology 31:1241–1248
Moreno-Kustner B, Martin C, Pastor L (2018) Prevalence of psychotic disorders and its association with methodological issues. A systematic review and meta-analyses. PLoS One 13:e0195687
Munro TA, Berry LM, Van’t Veer A, Béguin C, Carroll FI, Zhao Z, Carlezon WA, Cohen BM (2012) Long-acting κ opioid antagonists nor-BNI, GNTI and JDTic: pharmacokinetics in mice and lipophilicity. BMC Pharmacol 12:5
Naganawa M, Dickinson GL, Zheng M-Q, Henry S, Vandenhende F, Witcher J, Bell R, Nabulsi N, Lin S-F, Ropchan J (2016) Receptor occupancy of the κ-opioid antagonist LY2456302 measured with positron emission tomography and the novel radiotracer 11C-LY2795050. J Pharmacol Exp Ther 356:260–266
Nemeth CL, Paine TA, Rittiner JE, Béguin C, Carroll FI, Roth BL, Cohen BM, Carlezon WA (2010) Role of kappa-opioid receptors in the effects of salvinorin A and ketamine on attention in rats. Psychopharmacology 210:263–274
Nierenberg AA, Farabaugh AH, Alpert JE, Gordon J, Worthington JJ, Rosenbaum JF, Fava M (2000) Timing of onset of antidepressant response with fluoxetine treatment. Am J Psychiatry 157:1423–1428
Nuechterlein KH, Barch DM, Gold JM, Goldberg TE, Green MF, Heaton RK (2004) Identification of separable cognitive factors in schizophrenia. Schizophr Res 72:29–39
Nyhuis PW, Gastpar M, Scherbaum N (2008) Opiate treatment in depression refractory to antidepressants and electroconvulsive therapy. J Clin Psychopharmacol 28:593–595
Patkar KA, Wu J, Ganno ML, Singh HD, Ross NC, Rasakham K, Toll L, McLaughlin JP (2013) Physical presence of nor-binaltorphimine in mouse brain over 21 days after a single administration corresponds to its long-lasting antagonistic effect on κ-opioid receptors. J Pharmacol Exp Ther 346:545–554
Peckham AM, De La Cruz A, Dufresne RL (2018) Kappa opioid receptor antagonism: are opioids the answer for treatment resistant depression? Mental Health Clin 8:175–183
Pellow S, Chopin P, File SE, Briley M (1985) Validation of open: closed arm entries in an elevated plus-maze as a measure of anxiety in the rat. J Neurosci Methods 14:149–167
Pfeiffer A, Brantl V, Herz A, Emrich HM (1986) Psychotomimesis mediated by k opiate receptors. Science 233:774–776
Pliakas AM, Carlson RR, Neve RL, Konradi C, Nestler EJ, Carlezon WA (2001) Altered responsiveness to cocaine and increased immobility in the forced swim test associated with elevated cAMP response element-binding protein expression in nucleus accumbens. J Neurosci 21:7397–7403
Porsolt RD, Le Pichon M, Jalfre M (1977) Depression: a new animal model sensitive to antidepressant treatments. Nature 266:730–732
Portoghese PS, Lipkowski A, Takemori A (1987) Bimorphinans as highly selective, potent. Kappa. Opioid receptor antagonists. J Med Chem 30:238–239
Reece PA, Sedman AJ, Rose S, Wright DS, Dawkins R, Rajagopalan R (1994) Diuretic effects, pharmacokinetics, and safety of a new centrally acting kappa-opioid agonist (CI-977) in humans. J Clin Pharmacol 34:1126–1132
Reed B, Fang N, Mayer-Blackwell B, Chen S, Yuferov V, Zhou Y, Kreek MJ (2012) Chromatin alterations in response to forced swimming underlie increased prodynorphin transcription. Neuroscience 220:109–118
Reed B, Butelman ER, Fry RS, Kimani R, Kreek MJ (2018) Repeated administration of opra kappa (LY2456302), a novel, short-acting, selective KOP-r antagonist, in persons with and without cocaine dependence. Neuropsychopharmacology 43:739–750
Resnick RB, Fink M, Freedman AM (1971) Cyclazocine treatment of opiate dependence: a progress report. Compr Psychiatry 12:491–502
Rorick-Kehn LM, Witkin JM, Statnick MA, Eberle EL, McKinzie JH, Kahl SD, Forster BM, Wong CJ, Li X, Crile RS (2014) LY2456302 is a novel, potent, orally-bioavailable small molecule kappa-selective antagonist with activity in animal models predictive of efficacy in mood and addictive disorders. Neuropharmacology 77:131–144
Rorick-Kehn LM, Witcher JW, Lowe SL, Gonzales CR, Weller MA, Bell RL, Hart JC, Need AB, McKinzie JH, Statnick MA (2015) Determining pharmacological selectivity of the kappa opioid receptor antagonist LY2456302 using pupillometry as a translational biomarker in rat and human. Int J Neuropsychopharmacol 18
Ross M, Berger PA, Goldstein A (1979) Plasma beta-endorphin immunoreactivity in schizophrenia. Science 205:1163–1164
Roth BL, Baner K, Westkaemper R, Siebert D, Rice KC, Steinberg S, Ernsberger P, Rothman RB (2002) Salvinorin A: a potent naturally occurring nonnitrogenous κ opioid selective agonist. Proc Natl Acad Sci 99:11934–11939
Russell SE, Rachlin AB, Smith KL, Muschamp J, Berry L, Zhao Z, Chartoff EH (2014) Sex differences in sensitivity to the depressive-like effects of the kappa opioid receptor agonist U-50488 in rats. Biol Psychiatry 76:213–222
Saito T, Hirai H, Y-J KIM, Kojima Y, Matsunaga Y, Nishida H, Sakakibara T, Suga O, Sujaku T, Kojima N (2002) CJ-15, 208, a novel kappa opioid receptor antagonist from a fungus, Ctenomyces serratus ATCC15502. J Antibiot 55:847–854
Schattauer SS, Land BB, Reichard KL, Abraham AD, Burgeno LM, Kuhar JR, Phillips PE, Ong SE, Chavkin C (2017) Peroxiredoxin 6 mediates Gαi protein-coupled receptor inactivation by cJun kinase. Nat Commun 8:1–14
Shannon HE, Eberle EL, Mitch CH, McKinzie DL, Statnick MA (2007) Effects of kappa opioid receptor agonists on attention as assessed by a 5-choice serial reaction time task in rats. Neuropharmacology 53:930–941
Shekhar A (2019) Role of kappa opioid receptors in symptoms of schizophrenia: what is the neurobiology? Biol Psychiatry 86:494–496
Shirayama Y, Ishida H, Iwata M, Hazama GI, Kawahara R, Duman RS (2004) Stress increases dynorphin immunoreactivity in limbic brain regions and dynorphin antagonism produces antidepressant-like effects. J Neurochem 90:1258–1268
Stevens WC, Jones RM, Subramanian G, Metzger TG, Ferguson DM, Portoghese PS (2000) Potent and selective indolomorphinan antagonists of the kappa-opioid receptor. J Med Chem 43:2759–2769
Tejeda HA, Chefer VI, Zapata A, Shippenberg TS (2010) The effects of kappa-opioid receptor ligands on prepulse inhibition and CRF-induced prepulse inhibition deficits in the rat. Psychopharmacology 210:231–240
Thomas JB, Atkinson RN, Rothman RB, Fix SE, Mascarella SW, Vinson NA, Xu H, Dersch CM, Lu Y-F, Cantrell BE (2001) Identification of the first trans-(3 R, 4 R)-dimethyl-4-(3-hydroxyphenyl) piperidine derivative to possess highly potent and selective opioid κ receptor antagonist activity. J Med Chem 44:2687–2690
Todtenkopf MS, Marcus JF, Portoghese PS, Carlezon WA (2004) Effects of κ-opioid receptor ligands on intracranial self-stimulation in rats. Psychopharmacology 172:463–470
Toll L, Berzetei-Gurske I, Polgar W, Brandt S, Adapa I, Rodriguez L, Schwartz R, Haggart D, O’brien A, White A (1998) Standard binding and functional assays related to medications development division testing for potential cocaine and opiate narcotic treatment medications. NIDA Res Monogr 178:440–466
Urbano M, Guerrero M, Rosen H, Roberts E (2014) Antagonists of the kappa opioid receptor. Bioorg Med Chem Lett 24:2021–2032
Valenza M, Butelman ER, Kreek MJ (2017) Effects of the novel relatively short-acting kappa opioid receptor antagonist LY2444296 in behaviors observed after chronic extended-access cocaine self-administration in rats. Psychopharmacology 234:2219–2231
Ventriglia M, Chiavetto LB, Bonvicini C, Tura G, Bignotti S, Racagni G, Gennarelli M (2002) Allelic variation in the human prodynorphin gene promoter and schizophrenia. Neuropsychobiology 46:17–21
Vijay A, Wang S, Worhunsky P, Zheng MQ, Nabulsi N, Ropchan J (2016) PET imaging reveals sex differences in kappa opioid receptor availability in humans, in vivo. Am J Nucl Med Mol Imaging 6:205–214
Vonvoigtlander P, Lahti R, Ludens J (1983) U-50,488: a selective and structurally novel non-Mu (kappa) opioid agonist. J Pharmacol Exp Ther 224:7–12
Wadenberg ML (2003) A review of the properties of Spiradoline: a potent and selective k-opioid receptor agonist. CNS Drug Rev 9:187–198
Walsh SL, Strain EC, Abreu ME, Bigelow GE (2001) Enadoline, a selective kappa opioid agonist: comparison with butorphanol and hydromorphone in humans. Psychopharmacology 157:151–162
Wang Y-J, Rasakham K, Huang P, Chudnovskaya D, Cowan A, Liu-Chen L-Y (2011) Sex difference in κ-opioid receptor (KOPR)-mediated behaviors, brain region KOPR level and KOPR-mediated guanosine 5′-O-(3-[35S] thiotriphosphate) binding in the Guinea pig. J Pharmacol Exp Ther 339:438–450
Wang J, Song Q, Xu A, Bao Y, Xu Y, Zhu Q (2017) Design, synthesis and biological evaluation of aminobenzyloxyarylamide derivatives as selective κ opioid receptor antagonists. Eur J Med Chem 130:15–25
Watson SJ, Berger PA, Akil H, Mills MJ, Barchas JD (1978) Effects of naloxone on schizophrenia: reduction in hallucinations in a subpopulation of subjects. Science 201:73–76
Wells AM, Ridener E, Bourbonais CA, Kim W, Pantazopoulos H, Carroll FI, Kim K-S, Cohen BM, Carlezon WA (2017) Effects of chronic social defeat stress on sleep and circadian rhythms are mitigated by kappa-opioid receptor antagonism. J Neurosci 37:7656–7668
Yan F, Bikbulatov RV, Mocanu V, Dicheva N, Parker CE, Wetsel WC, Mosier PD, Westkaemper RB, Allen JA, Zjawiony JK (2009) Structure-based design, synthesis, and biochemical and pharmacological characterization of novel salvinorin A analogues as active state probes of the κ-opioid receptor. Biochemistry 48:6898–6908
Zhang A, Zhou G, Xi G, Gu N, Xia Z, Yao J, Chang J, Webber R, Potkin S (1985) Lower CSF level of dynorphin (1–8) immunoreactivity in schizophrenic patients. Neuropeptides 5:553–556
Zhang CS, Tan Z, Lu L, Wu SN, He Y, Gu NF, Feng GY, He L (2004) Polymorphism of prodynorphin promoter is associated with schizophrenia in Chinese population. Acta Pharmacol Sin 25:1022–1026
Zhang H, Shi Y-G, Woods JH, Watson SJ, Ko M-C (2007) Central κ-opioid receptor-mediated antidepressant-like effects of nor-Binaltorphimine: behavioral and BDNF mRNA expression studies. Eur J Pharmacol 570:89–96
Acknowledgements
Dr. Dustin Tetzl, MD for editorial assistance.
Funding Sources
None.
Disclosures
Dr. Clark and Dr. Tetzl are employed by, receive salary from, and own stock in Terran Biosciences Inc.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2020 The Author(s)
About this chapter
Cite this chapter
Clark, S.D. (2020). The Role of Dynorphin and the Kappa Opioid Receptor in Schizophrenia and Major Depressive Disorder: A Translational Approach. In: Liu-Chen, LY., Inan, S. (eds) The Kappa Opioid Receptor. Handbook of Experimental Pharmacology, vol 271. Springer, Cham. https://doi.org/10.1007/164_2020_396
Download citation
DOI: https://doi.org/10.1007/164_2020_396
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-89073-5
Online ISBN: 978-3-030-89074-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)