Abstract
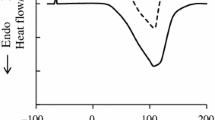
Since chitosan was identified as a hemostatic agent in the 1980s, “chitosan and platelets” has developed into a topic of intense interest. This chapter gives an overview of platelet biogenesis, composition, activation, and mechanisms implicated in chitosan–platelet interactions. Chitosan is a unique acid-soluble cationic glucosamine polysaccharide with tunable molecular weight, glucosamine/N-acetyl glucosamine content, and acetylation pattern. Platelets are small anuclear cells with anionic surfaces that are released to the blood stream by megakaryocytes that reside in bone marrow and the lung. Platelets are stocked with granules that contain a plethora of bioactive wound-healing and procoagulant factors. Upon activation by agonists, or adhesion to von Willebrand factor “strings” under shear stress, platelets aid in fibrin clot formation to seal off a wound and initiate wound repair. Purified platelets rapidly adhere to a variety of solid chitosan and chitin substrates but show inconsistent levels of activation in the absence of calcium. Chitosans with a positive charge state bind to platelets and potentiate alpha granule release in whole blood or recalcified platelet-rich plasma (PRP). Platelet activation kinetics were accelerated by higher chitosan deacetylation levels and molecular weight (95% vs. 80% deacetylated, 177 kDa vs. 102 kDa), but mis-timed platelet degranulation prior to thrombin activation led to weaker clot tensile strength. Neutral-soluble chitosans (oligomers, 50% reacetylated chitosans) do not activate platelets and hydrophobic butyryl-chitosan coatings inhibit platelet adhesion. Collective data suggest two mechanisms underlying chitosan–platelet interactions: (1) non-specific electrostatic binding of anionic platelets to positively charged chitosan surfaces, and (2) platelet binding to blood plasma factors adsorbed on chitosan or chitin surfaces. Future directions include deepening our understanding of the molecular basis for thrombocyte–chitosan interactions, and the performance of platelet-activating chitosan formulations in clinically relevant contexts where platelet physiology is altered by medications, trauma, or disease.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Khor E, Lim LY (2003) Implantable applications of chitin and chitosan. Biomaterials 24:2339–2349. https://doi.org/10.1016/S0142-9612(03)00026-7
Fong D, Grégoire-Gélinas P, Cheng AP, Mezheritsky T, Lavertu M, Sato S, Hoemann CD (2017) Lysosomal rupture induced by structurally distinct chitosans either promotes a type 1 IFN response or activates the inflammasome in macrophages. Biomaterials 129:127–138. https://doi.org/10.1016/j.biomaterials.2017.03.022
Chang KLB, Tsai G, Lee J, Fu W-R (1997) Heterogeneous N-deacetylation of chitin in alkaline solution. Carbohydr Res 303:327–332. https://doi.org/10.1016/S0008-6215(97)00179-1
Lamarque G, Viton C, Domard A (2004) Comparative study of the first heterogeneous deacetylation of α- and β-chitins in a multistep process. Biomacromolecules 5:992–1001. https://doi.org/10.1021/bm034498j
Vårum KM, Anthonsen MW, Grasdalen H, Smidsrød O (1991) 13C-N.m.r. studies of the acetylation sequences in partially N-deacetylated chitins (chitosans). Carbohydr Res 217:19–27. https://doi.org/10.1016/0008-6215(91)84113-S
Sashiwa H, Saimoto H, Shigemasa Y, Ogawa R, Tokura S (1991) Distribution of the acetamide group in partially deacetylated chitins. Carbohydr Polym 16:291–296. https://doi.org/10.1016/0144-8617(91)90114-R
Kubota N, Tatsumoto N, Sano T, Toya K (2000) A simple preparation of half N-acetylated chitosan highly soluble in water and aqueous organic solvents. Carbohydr Res 324:268–274. https://doi.org/10.1016/s0008-6215(99)00263-3
Fischer TH, Connolly R, Thatte HS, Schwaitzberg SS (2004) Comparison of structural and hemostatic properties of the poly-N-acetyl glucosamine Syvek Patch with products containing chitosan. Microsc Res Tech 63:168–174. https://doi.org/10.1002/jemt.20017
Thatte HS, Zagarins S, Khuri SF, Fischer TH (2004) Mechanisms of poly-N-acetyl glucosamine polymer-mediated hemostasis: platelet interactions. J Trauma 57:S13–S21. https://doi.org/10.1097/01.TA.0000136743.12440.89
Rinaudo M, Pavlov G, Desbrières J (1999) Influence of acetic acid concentration on the solubilization of chitosan. Polymer 40:7029–7032. https://doi.org/10.1016/S0032-3861(99)00056-7
Filion D, Lavertu M, Buschmann MD (2007) Ionization and solubility of chitosan solutions related to thermosensitive chitosan/glycerol-phosphate systems. Biomacromolecules 8:3224–3234. https://doi.org/10.1021/bm700520m
Hoemann CD, Guzmán-Morales J, Tran-Khanh N, Lavallée G, Jolicoeur M, Lavertu M (2013) Chitosan rate of uptake in HEK293 cells is influenced by soluble versus microparticle state and enhanced by serum-induced cell metabolism and lactate-based media acidification. Molecules 18:1015–1035. https://doi.org/10.3390/molecules18011015
Hoemann CD, Hurtig M, Rossomacha E, Sun J, Chevrier A, Shive MS, Buschmann MD (2005) Chitosan-glycerol phosphate/blood implants improve hyaline cartilage repair in ovine microfracture defects. J Bone Joint Surg 87:2671–2686. https://doi.org/10.2106/JBJS.D.02536
Marchand C, Bachand J, Périnêt J, Baraghis E, Lamarre M, Rivard GE, De Crescenzo G, Hoemann CD (2009) C3, C5, and factor B bind to chitosan without complement activation. J Biomed Mater Res 9999A. https://doi.org/10.1002/jbm.a.32638
Chevrier A, Darras V, Picard G, Nelea M, Veilleux D, Lavertu M, Hoemann CD, Buschman MD (2018) Injectable chitosan-platelet-rich plasma implants to promote tissue regeneration: in vitro properties, in vivo residence, degradation, cell recruitment and vascularization: chitosan-PRP injectable implants for tissue repair. J Tissue Eng Regen Med 12:217–228. https://doi.org/10.1002/term.2403
Hoemann CD, Guzmán-Morales J, Picard G, Chen G, Veilleux D, Chevrier A, Sim S, Garon M, Quenneville E, Lafantaisie-Favreau C-H, Buschmann MD, Hurtig MB (2020) Guided bone marrow stimulation for articular cartilage repair through a freeze-dried chitosan microparticle approach. Materialia 9:100609. https://doi.org/10.1016/j.mtla.2020.100609
Deprés-Tremblay G, Chevrier A, Tran-Khanh N, Nelea M, Buschmann MD (2017) Chitosan inhibits platelet-mediated clot retraction, increases platelet-derived growth factor release, and increases residence time and bioactivity of platelet-rich plasma in vivo. Biomed Mater 13:015005. https://doi.org/10.1088/1748-605X/aa8469
Cunha AG, Fernandes SCM, Freire CSR, Silvestre AJD, Neto CP, Gandini A (2008) What is the real value of Chitosan’s surface energy? Biomacromolecules 9:610–614. https://doi.org/10.1021/bm701199g
Onishi H, Machida Y (1999) Biodegradation and distribution of water-soluble chitosan in mice. Biomaterials 20:175–182. https://doi.org/10.1016/S0142-9612(98)00159-8
Aam BB, Heggset EB, Norberg AL, Sørlie M, Vårum KM, Eijsink VGH (2010) Production of Chitooligosaccharides and their potential applications in medicine. Mar Drugs 8:1482–1517. https://doi.org/10.3390/md8051482
George JN, Colman RW (2001) Platelets. In: Hemostasis & thrombosis: basic principles & clinical practice. 4th edn. Lippincott Williams & Wilkins, Baltimore, pp 381–386
Kuter DJ (2001) Megakaryopoiesis and thrombpoiesis. In: Williams hematology. 6th edn. McGraw-Hill, New York, pp 1339–1355
Cunin P, Nigrovic PA (2019) Megakaryocytes as immune cells. J Leukoc Biol 105:1111–1121. https://doi.org/10.1002/JLB.MR0718-261RR
Lefrancais E, Ortiz-Munoz G, Caudrillier A, Mallavia B, Liu F, Sayah D, Thornton E, Headley M, David T, Coughlin S, Krummel M, Leavitt A, Passegué E, Looney M (2017) The lung is a site of platelet biogenesis and a reservoir for hematopoietic progenitors. Nature 544. https://doi.org/10.1038/nature21706
Rapkiewicz AV, Mai X, Carsons SE, Pittaluga S, Kleiner DE, Berger JS, Thomas S, Adler NM, Charytan DM, Gasmi B, Hochman JS, Reynolds HR (2020) Megakaryocytes and platelet-fibrin thrombi characterize multi-organ thrombosis at autopsy in COVID-19: a case series. EClinicalMedicine 24:100434. https://doi.org/10.1016/j.eclinm.2020.100434
Lefrançais E, Looney MR (2019) Platelet biogenesis in the lung circulation. Physiology (Bethesda) 34:392–401. https://doi.org/10.1152/physiol.00017.2019
Ryan DH (2001) Examination of the blood. In: Williams hematology. 6th edn. McGraw-Hill, New York, pp 9–16
Owens AP, Mackman N (2011) Microparticles in hemostasis and thrombosis. Circ Res 108:1284–1297. https://doi.org/10.1161/CIRCRESAHA.110.233056
Alphonsus CS, Rodseth RN (2014) The endothelial glycocalyx: a review of the vascular barrier. Anaesthesia 69:777–784. https://doi.org/10.1111/anae.12661
Cramer EM (2001) Platelets and megakaryocytes: analtomy and structural organization. In: Hemostasis & thrombosis: basic principles & clinical practice. 4th edn. Lippincott Williams & Wilkins, Baltimore, pp 411–428
Ogasawara K, Ueki J, Takenaka M, Furihata K (1993) Study on the expression of ABH antigens on platelets. Blood 82:993–999. https://doi.org/10.1182/blood.V82.3.993.993
Cooling L (2015) Blood groups in infection and host susceptibility | clinical microbiology reviews. Clin Microbiol Rev 28:801–870. https://doi.org/10.1128/CMR.00109-14
Verhoef PA, Kannan S, Sturgill JL, Tucker EW, Morris PE, Miller AC, Sexton TR, Koyner JL, Hejal R, Brakenridge SC, Moldawer LL, Hotchkiss RS, Blood TM, Mazer MB, Bolesta S, Alexander SA, Armaignac DL, Shein SL, Jones C, Hoemann CD, Doctor A, Friess SH, Parker RI, Rotta AT, Remy KE, for the B. and T.S.C. of the R.S. for the S. of C.C (2021) Medicine, severe acute respiratory syndrome–associated coronavirus 2 infection and organ dysfunction in the ICU: opportunities for translational research. Critic Care Explor 3:e0374. https://doi.org/10.1097/CCE.0000000000000374
Stowell SR, Stowell CP (2019) Biologic roles of the ABH and Lewis histo-blood group antigens part II: thrombosis, cardiovascular disease and metabolism. Vox Sang 114:535–552. https://doi.org/10.1111/vox.12786
Brummel KE, Paradis SG, Butenas S, Mann KG (2002) Thrombin functions during tissue factor–induced blood coagulation. Blood 100:148–152. https://doi.org/10.1182/blood.V100.1.148
Rand MD, Lock JB, van’t Veer C, Gaffney DP, Mann KG (1996) Blood clotting in minimally altered whole blood. Blood 88:3432–3445
Fukami MH, Holmsen H, Kowalska A, Niewiarowski S (2001) Platelet secretion. In: Hemostasis & thrombosis: basic principles and clinical practice. 4th edn. Lippincott Williams & Wilkins, Baltimore, pp 561–573
Contreras-García A, D’Elía NL, Desgagné M, Lafantaisie-Favreau C-H, Rivard G-E, Ruiz J-C, Wertheimer MR, Messina P, Hoemann CD (2019) Synthetic anionic surfaces can replace microparticles in stimulating burst coagulation of blood plasma. Colloids Surf B Biointerfaces 175:596–605. https://doi.org/10.1016/j.colsurfb.2018.11.066
Rivera J, Lozano ML, Navarro-Nunez L, Vicente V (2009) Platelet receptors and signaling in the dynamics of thrombus formation. Haematologica 94:700–711. https://doi.org/10.3324/haematol.2008.003178
Lenting PJ, Christophe OD, Denis CV (2015) von Willebrand factor biosynthesis, secretion, and clearance: connecting the far ends. Blood 125:2019–2028. https://doi.org/10.1182/blood-2014-06-528406
Bryckaert M, Rosa J-P, Denis CV, Lenting PJ (2015) Of von Willebrand factor and platelets. Cell Mol Life Sci 72:307–326. https://doi.org/10.1007/s00018-014-1743-8
Parise LV, Smyth SS, Coller BS (2001) Platelet morphology, biochemistry, and function. In: Williams hematology. 6th edn. McGraw-Hill, New York, pp 1357–1408
Thierry B, Winnik FM, Merhi Y, Silver J, Tabrizian M (2003) Bioactive coatings of endovascular stents based on polyelectrolyte multilayers. Biomacromolecules 4:1564–1571. https://doi.org/10.1021/bm0341834
Schmitt A, Jouault H, Guichard J, Wendling F, Drouin A, Cramer EM (2000) Pathologic interaction between megakaryocytes and polymorphonuclear leukocytes in myelofibrosis. Blood 96:1342–1347. https://doi.org/10.1182/blood.V96.4.1342
Tanaka M, Aze Y, Shinomiya K, Fujita T (1996) Morphological observations of megakaryocytic emperipolesis in the bone marrow of rats treated with lipopolysaccharide. J Vet Med Sci 58:663–667. https://doi.org/10.1292/jvms.58.663
Cunin P, Bouslama R, Machlus KR, Martínez-Bonet M, Lee PY, Wactor A, Nelson-Maney N, Morris A, Guo L, Weyrich A, Sola-Visner M, Boilard E, Italiano JE, Nigrovic PA (2019) Megakaryocyte emperipolesis mediates membrane transfer from intracytoplasmic neutrophils to platelets. Elife 8:e44031. https://doi.org/10.7554/eLife.44031
Sun Y, Wu B, Yan S, Zhang J, Zhang R, Zhu S (2013) Preparation of hemostatic sponge used for dressing, involves preparing chitosan aqueous solution, injecting into mold, freezing chitosan aqueous solution in mold, freeze-drying frozen material and post-processing chitosan sponge. CN103028135-A, 2013–N96850
Kim C, Lee S, Lim J, Son Y, Kim K, Gin Y, Kim CH, Lee SJ, Lim IJ, Son YS (2017) Method of producing a porous chitosan scaffold comprises freeze-drying of an aqueous acidic solution having chitosan and a solvent, and neutralizing the aqueous acidic solution. WO2007111416-A1
Lafantaisie-Favreau C-H, Guzmán-Morales J, Sun J, Chen G, Harris A, Smith TD, Carli A, Henderson J, Stanish WD, Hoemann CD (2013) Subchondral pre-solidified chitosan/blood implants elicit reproducible early osteochondral wound-repair responses including neutrophil and stromal cell chemotaxis, bone resorption and repair, enhanced repair tissue integration and delayed matrix deposition. BMC Musculoskelet Disord 14:27. https://doi.org/10.1186/1471-2474-14-27
Ghazi Zadeh L, Chevrier A, Lamontagne M, Buschmann MD, Hoemann CD, Lavertu M (2019) Multiple platelet-rich plasma preparations can solubilize freeze-dried chitosan formulations to form injectable implants for orthopedic indications. Biomed Mater Eng 30:349–364. https://doi.org/10.3233/BME-191058
Benesch J, Tengvall P (2002) Blood protein adsorption onto chitosan. Biomaterials 23:2561–2568. https://doi.org/10.1016/S0142-9612(01)00391-X
Rao SB, Sharma CP (1997) Use of chitosan as a biomaterial: studies on its safety and hemostatic potential. J Biomed Mater Res 34:21–28
Hoemann CD, Hurtig M, Rossomacha E, Sun J, Chevrier A, Shive MS, Buschmann MD (2005) Chitosan-glycerol phosphate/blood implants improve hyaline cartilage repair in ovine microfracture defects. The Journal of Bone & Joint Surgery 87:2671–2686. https://doi.org/10.2106/JBJS.D.02536
del Conde I, Crúz MA, Zhang H, López JA, Afshar-Kharghan V (2005) Platelet activation leads to activation and propagation of the complement system. J Exp Med 201:871–879. https://doi.org/10.1084/jem.20041497
Uchimido R, Schmidt EP, Shapiro NI (2019) The glycocalyx: a novel diagnostic and therapeutic target in sepsis. Crit Care 23:16. https://doi.org/10.1186/s13054-018-2292-6
Ellies LG, Ditto D, Levy GG, Wahrenbrock M, Ginsburg D, Varki A, Le DT, Marth JD (2002) Sialyltransferase ST3Gal-IV operates as a dominant modifier of hemostasis by concealing asialoglycoprotein receptor ligands. Proc Natl Acad Sci U S A 99:10042–10047. https://doi.org/10.1073/pnas.142005099
Grewal PK, Uchiyama S, Ditto D, Varki N, Le DT, Nizet V, Marth JD (2008) The Ashwell receptor mitigates the lethal coagulopathy of sepsis. Nat Med 14:648–655. https://doi.org/10.1038/nm1760
Dang CV, Shin CK, Bell WR, Nagaswami C, Weisel JW (1989) Fibrinogen sialic acid residues are low affinity calcium-binding sites that influence fibrin assembly. J Biol Chem 264:15104–15108. https://doi.org/10.1016/S0021-9258(18)63817-7
Varki A, Schauer R (2009) Sialic acids. In: Varki A, Cummings RD, Esko JD, Freeze HH, Stanley P, Bertozzi CR, Hart GW, Etzler ME Essentials of glycobiology. 2nd edn. Cold Spring Harbor Laboratory Press, Cold Spring Harbor, http://www.ncbi.nlm.nih.gov/books/NBK1920/. Accessed 20 Mar 2021
Malette WG, Quigley HJ, Gaines RD, Johnson ND, Rainer WG (1983) Chitosan: a new hemostatic. Ann Thorac Surg 36:55–58. https://doi.org/10.1016/s0003-4975(10)60649-2
Klokkevold PR, Lew DS, Ellis DG, Bertolami CN (1991) Effect of chitosan on lingual hemostasis in rabbits. J Oral Maxillofac Surg 49:858–863. https://doi.org/10.1016/0278-2391(91)90017-G
Chou T-C, Fu E, Wu C-J, Yeh J-H (2003) Chitosan enhances platelet adhesion and aggregation. Biochem Biophys Res Commun 302:480–483. https://doi.org/10.1016/S0006-291X(03)00173-6
Okamoto Y, Yano R, Miyatake K, Tomohiro I, Shigemasa Y, Minami S (2003) Effects of chitin and chitosan on blood coagulation. Carbohydr Polym 53:337–342. https://doi.org/10.1016/S0144-8617(03)00076-6
Lin C-W, Lin J-C (2003) Characterization and blood coagulation evaluation of the water-soluble Chitooligosaccharides prepared by a facile fractionation method. Biomacromolecules 4:1691–1697. https://doi.org/10.1021/bm034129n
Hattori H, Ishihara M (2015) Changes in blood aggregation with differences in molecular weight and degree of deacetylation of chitosan. Biomed Mater 10:015014. https://doi.org/10.1088/1748-6041/10/1/015014
Whang HS, Kirsch W, Zhu YH, Yang CZ, Hudson SM (2005) Hemostatic agents derived from chitin and chitosan. J Macromol Sci C 45:309–323. https://doi.org/10.1080/15321790500304122
Behrens AM, Sikorski MJ, Kofinas P (2014) Hemostatic strategies for traumatic and surgical bleeding: hemostatic strategies for traumatic and surgical bleeding. J Biomed Mater Res 102:4182–4194. https://doi.org/10.1002/jbm.a.35052
Romani AA, Ippolito L, Riccardi F, Pipitone S, Morganti M, Baroni MC, Borghetti AF, Bettini R (2013) In vitro blood compatibility of novel hydrophilic chitosan films for vessel regeneration and repair. Adv Biomater Sci Biomed Appl. https://doi.org/10.5772/52706
Sundaram MN, Mony U, Varma PK, Rangasamy J (2021) Vasoconstrictor and coagulation activator entrapped chitosan based composite hydrogel for rapid bleeding control. Carbohydr Polym 258:117634. https://doi.org/10.1016/j.carbpol.2021.117634
Marchand C, Rivard G-E, Sun J, Hoemann CD (2009) Solidification mechanisms of chitosan–glycerol phosphate/blood implant for articular cartilage repair. Osteoarthr Cartil 17:953–960. https://doi.org/10.1016/j.joca.2008.12.002
Hoemann CD, Chen G, Marchand C, Tran-Khanh N, Thibault M, Chevrier A, Sun J, Shive MS, Fernandes MJG, Poubelle PE, Centola M, El-Gabalawy H (2010) Scaffold-guided subchondral bone repair: implication of neutrophils and alternatively activated Arginase-1+ macrophages. Am J Sports Med 38:1845–1856. https://doi.org/10.1177/0363546510369547
Bell AD, Hurtig MB, Quenneville E, Rivard G-É, Hoemann CD (2017) Effect of a rapidly degrading Presolidified 10 kDa chitosan/blood implant and subchondral marrow stimulation surgical approach on cartilage resurfacing in a sheep model. Cartilage 8:417–431. https://doi.org/10.1177/1947603516676872
Guzmán-Morales J, Lafantaisie-Favreau C-H, Chen G, Hoemann CD (2014) Subchondral chitosan/blood implant-guided bone plate resorption and woven bone repair is coupled to hyaline cartilage regeneration from microdrill holes in aged rabbit knees. Osteoarthr Cartil 22:323–333. https://doi.org/10.1016/j.joca.2013.12.011
Dwivedi G, Chevrier A, Hoemann CD, Buschmann MD (2019) Injectable freeze-dried chitosan-platelet-rich-plasma implants improve marrow-stimulated cartilage repair in a chronic-defect rabbit model. J Tissue Eng Regen Med 13:599–611. https://doi.org/10.1002/term.2814
Zhao X, Guo B, Wu H, Liang Y, Ma PX (2018) Injectable antibacterial conductive nanocomposite cryogels with rapid shape recovery for noncompressible hemorrhage and wound healing. Nat Commun 9:2784. https://doi.org/10.1038/s41467-018-04998-9
Ghavidel Mehr N, Hoemann CD, Favis BD (2015) Chitosan surface modification of fully interconnected 3D porous poly(ε-caprolactone) by the LbL approach. Polymer 64:112–121. https://doi.org/10.1016/j.polymer.2015.03.025
Mao C, Qiu Y, Sang H, Mei H, Zhu A, Shen J, Lin S (2004) Various approaches to modify biomaterial surfaces for improving hemocompatibility. Adv Colloid Interface Sci 110:5–17. https://doi.org/10.1016/j.cis.2004.02.001
Yatomi Y, Igarashi Y, Yang L, Hisano N, Qi R, Asazuma N, Satoh K, Ozaki Y, Kume S (1997) Sphingosine 1-phosphate, a bioactive sphingolipid abundantly stored in platelets, is a Normal constituent of human plasma and serum. J Biochem 121:969–973. https://doi.org/10.1093/oxfordjournals.jbchem.a021681
Jeon J-H, Kim Y-S, Choi E-J, Cheon S, Kim S, Kim J-S, Jang JS, Ha WS, Park ST, Park CS, Park K, Park B-K (2001) Implication of co-measured platelet factor 4 in the reliability of the results of the plasma transforming growth factor-β1 measurement. Cytokine 16:102–105. https://doi.org/10.1006/cyto.2001.0895
Erbel C, Korosoglou G, Ler P, Akhavanpoor M, Domschke G, Linden F, Doesch AO, Buss SJ, Giannitsis E, Katus HA, Gleissner CA (2015) CXCL4 plasma levels are not associated with the extent of coronary artery disease or with coronary plaque morphology. PLoS One 10:e0141693. https://doi.org/10.1371/journal.pone.0141693
Du Q, Li E, Liu Y, Xie W, Huang C, Song J, Zhang W, Zheng Y, Wang H, Wang Q (2018) CTAPIII/CXCL7: a novel biomarker for early diagnosis of lung cancer. Cancer Med 7:325–335. https://doi.org/10.1002/cam4.1292
Franciotta D, Zardini E, Ravaglia S, Piccolo G, Andreoni L, Bergamaschi R, Romani A, Tavazzi E, Naldi P, Ceroni M, Marchioni E (2006) Cytokines and chemokines in cerebrospinal fluid and serum of adult patients with acute disseminated encephalomyelitis. J Neurol Sci 247:202–207. https://doi.org/10.1016/j.jns.2006.05.049
Neubauer H, Petrak F, Zahn D, Pepinghege F, Hägele A-K, Pirkl P-A, Uhl I, Juckel G, Mügge A, Herpertz S (2013) Newly diagnosed depression is associated with increased beta-thromboglobulin levels and increased expression of platelet activation markers and platelet derived CD40-CD40L. J Psychiatr Res 47:865–871. https://doi.org/10.1016/j.jpsychires.2013.03.011
Roberts HR, Monroe DM III, Hoffman M (2001) Molecular biology and biochemistry of the coagulation factors and pathways of hemostasis. In: Williams hematology. 6th edn. McGraw-Hill, New York, pp 1409–1434
Butenas S, Mann KG (2002) Blood coagulation. Biochemistry (Mosc) 67:3–12. https://doi.org/10.1023/a:1013985911759
Miller CH, Haff E, Platt SJ, Rawlins P, Drews CD, Dilley AB, Evatt B (2003) Measurement of von Willebrand factor activity: relative effects of ABO blood type and race. J Thromb Haemost 1:2191–2197. https://doi.org/10.1046/j.1538-7836.2003.00367.x
Ruiz FA, Lea CR, Oldfield E, Docampo R (2004) Human platelet dense granules contain polyphosphate and are similar to Acidocalcisomes of bacteria and unicellular eukaryotes. J Biol Chem 279:44250–44257. https://doi.org/10.1074/jbc.M406261200
Klemm KM, Klein MJ (2017) Biochemical markers of bone metabolism (chapter 15). In: Henry’s clinical diagnosis and management by laboratory methods. 23rd edn. Elsevier, St Louis, pp 188–204
Acknowledgements
We thank Catherine Marchand for PF4 and TAT analyses and J. Guzmán-Morales and J. Sun for hybrid blood clot images. Funding: Canadian Institutes of Health Research Operating grant; Prima-Ortho grant; George Mason University start-up funds.
Competing interest statement: C. Hoemann is a shareholder and on the Scientific Advisory Board of Ortho RTi.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Hoemann, C.D., Rivard, G.E. (2021). Chitosan–Platelet Interactions. In: Jayakumar, R., Prabaharan, M. (eds) Chitosan for Biomaterials III. Advances in Polymer Science, vol 287. Springer, Cham. https://doi.org/10.1007/12_2021_86
Download citation
DOI: https://doi.org/10.1007/12_2021_86
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-83806-5
Online ISBN: 978-3-030-83807-2
eBook Packages: Chemistry and Materials ScienceChemistry and Material Science (R0)