Abstract
Objective
Magnetic resonance imaging (MRI) findings in anterior cruciate ligament (ACL) injury are well known, but most published reviews show obvious examples of associated injuries and give little focus to paediatric patients. Here, we demonstrate the spectrum of MRI appearances at common sites of associated injury in adolescents with ACL tears, emphasising age-specific issues.
Methods
Pictorial review using images from children with surgically confirmed ACL tears after athletic injury.
Results
ACL injury usually occurs with axial rotation in the valgus near full extension. The MRI findings can be obvious and important to management (ACL rupture), subtle but clinically important (lateral meniscus posterior attachment avulsion), obvious and unimportant to management (femoral condyle impaction injury), or subtle and possibly important (medial meniscocapsular junction tear). Paediatric-specific issues of note include tibial spine avulsion, normal difficulty visualising a thin ACL and posterolateral corner structures, and differentiation between incompletely closed physis and impaction fracture.
Conclusion
ACL tear is only the most obvious sign of a complex injury involving multiple structures. Awareness of the spectrum of secondary findings illustrated here and the features distinguishing them from normal variation can aid in accurate assessment of ACL tears and related injuries, enabling effective treatment planning and assessment of prognosis.
Teaching points
• The ACL in children normally appears thin or attenuated, while thickening and oedema suggest tear.
• Displaced medial meniscal tears are significantly more common later post-injury than immediately.
• The meniscofemoral ligaments merge with the posterior lateral meniscus, complicating tear assessment.
• Tibial plateau impaction fractures can be difficult to distinguish from a partially closed physis.
• Axial MR sequences are more sensitive/specific than coronal for diagnosis of medial collateral ligament (MCL) injury.
Similar content being viewed by others
Introduction
Rupture of the anterior cruciate ligament (ACL) most commonly occurs as a result of a pivot-shift injury, requires substantial force to occur and is rarely a truly isolated event. At least half of ACL tears in young patients are accompanied by other injuries such as meniscal or ligament tears and bony contusions [1–3]. In non-contact injuries, the ACL is at greatest risk of injury when excessive valgus and knee axial rotation loads are combined near full knee extension [4–6], such as when the patient lands on the ground with their centre of gravity moving away from the landing limb. In addition to tearing the ACL, this type of injury places tensile load on the medial collateral ligament (MCL) and posteromedial corner structures, and leads to impaction and shear injuries in the lateral compartment.
The patterns of injury visible at magnetic resonance imaging (MRI) and their relation to specific injury mechanism and clinical outcomes in ACL injury have been well studied in children [3, 7] and adults [4, 6, 8, 9]. Early imaging reviews in the 1990s focused on the detection of ACL tears [10] or showed few images [11]. The actual ACL injury is generally easily detected [12, 13], particularly with improvements in MRI sequences, but some of the associated injuries remain subtle. Since these injuries may require treatment themselves, may alter the treatment plan when detected, or serve as markers of a poorer prognosis [1], it is important to identify them accurately. MR images in published studies are generally classic examples of obvious pathology [3, 4, 14], or focus only on the ACL itself and adult patterns [15]. Few studies have focused on ACL tears in paediatric patients [3, 7, 10, 11], a group in which this injury is being seen with increasing frequency [16]. In day-to-day practice, the distinction between normal and pathologic appearance of each structure at the knee can be difficult to make, particularly in adolescents. Therefore, the purpose of this pictorial review is to aid radiologists by demonstrating the spectrum of MR appearances at common sites of associated injury in children and teenagers with ACL tears, with emphasis on patterns specific to this age group.
ACL
Young children have weaker physes than ligaments, which can result in epiphyseal avulsion fractures at the anterior tibial spine near the ACL attachment rather than tearing of the ligament itself, for the same pivot-shift injury mechanism (Fig. 1) [3]. This review is limited to patients with ACL tears, but the search for associated injuries in a younger child with a tibial spine avulsion should follow the same pattern. The spectrum of ACL appearance from normal to completely torn is seen in Figs. 2 and 3. The normal ACL is composed of two bundles named for tibial attachment locations, anteromedial (dominant in knee flexion) and posterolateral (most active in extension) [17]. Partial tears can involve one or both bundles. In children the normal ACL can appear quite attenuated (Fig. 2b); in our experience a recently torn ACL is usually visibly thickened and oedematous, and a thin and appropriately oriented ligament without oedema is likely intact. In the last 110 cases at our institution, 7/48 (15 %) read by musculoskeletal radiologists and 26/62 (42 %) read by paediatric radiologists were initially reported as high-grade partial thickness ACL tears, while at later surgery all but one of these tears (99 %) was described as complete (Fig. 2c). Given the time delay between injury and surgery, it is possible that partial tears evolved to complete tears at surgery; however, the distinction between complete and partial tears is well known to be limited in reliability on MRI [18]. One challenge is that the torn ACL may form scar tissue that can mimic a partially intact ligament. A tear that appears to involve most of the ACL fibres is likely to be functionally complete, and we encourage reporting the tear in this fashion.
Tibial spine avulsion and Segond fracture. The arrow points to Segond fracture in each image. a Plain radiograph of a 16-year-old boy with a combination of injuries suggesting a pivot-shift impact mechanism. ACL was intact at surgery. b Coronal T1-weighted MRI in a different child also showing a tibial spine avulsion. c Segond fracture on coronal proton density (PD) MRI of a 15-year-old boy with ACL rupture. Note the lack of adjacent oedema, which is typical; these fractures are often subtle on MRI. Note also the fragment’s capsular attachment to the anterior oblique band of the lateral collateral ligament complex
Spectrum of ACL injury in sagittal plane (a–f). Proton-density (PD) images (with fat saturation [FS] except c and e) in paediatric patients age 13–16 years, showing (a) intact ACL, b intact but somewhat thin ACL, (c) our only surgically confirmed high grade partial tear of ACL, demonstrating lax fibres (arrow), (d) full thickness tear at midsubstance with some intact fibres near tibial attachment (arrow), (e) obvious full thickness tear (arrow), (f) full thickness tear with anteriorly flipped distal ligament fibres (arrow) and anterior tibial translation
Spectrum of ACL appearance in (a–c) coronal PD and (d–g) axial PD FS images. a Coronal image of intact ACL with two bundles barely distinguished from each other (arrow), (b) intact ACL with well separated bundles (arrow, middle) and (c) torn ACL. d Axial image of intact ACL with two bundles barely distinguished from each other (arrow), e intact ACL with well separated bundles (arrow), (f) torn ACL with some intact fibres at femoral attachment (arrow), (g) completely avulsed ACL (arrow)
Posteromedial corner
This region is the site of frequent, generally minor injury, either involving the meniscocapsular junction (Fig. 4b, c) or the peripheral “red” portion of the meniscus (Fig. 4d–i). The capsule posterior to the medial meniscus is usually only slightly higher in signal than adjacent tissue (Fig. 4a). In the posteromedial knee there is a confluence of structures (posterior oblique ligament, oblique popliteal ligament, and fibres of the semimembranosus tendon) that reinforce the posteromedial joint capsule. With valgus stress and knee rotation, capsular tension is transmitted to the meniscocapsular junction which places tensile stress on the periphery of the meniscus which can be subsequently torn [19]. The orientation (peripheral, vertical, and longitudinal) of this medial meniscal tear is typical after sports-related trauma. These tears account for most of the “false-positive” MRI diagnoses of meniscal tears, based on their absence (or interval healing) at later arthroscopy [20]. A likely explanation is that since the periphery of the meniscus is well vascularised, these tears heal well in the interval between MRI and surgery.
Spectrum of posteromedial corner injury on sagittal T2 FS images (image d is T2 GRE). a Intact meniscus: normal (left); increased signal at meniscocapsular junction representing minor strain, not meeting criteria for tear (middle; note the underlying tibial contusion); meniscocapsular junction tear, with no dark meniscal tissue posterior to the high-signal cleft (right). b Meniscal tears: horizontal extending to undersurface (left); oblique tear with tibial contusion (middle); displaced oblique tear with tibial contusion (right). c Meniscal tears: vertical tear (left); vertical and intrasubstance tear (middle); displaced complex tear, with vertical and horizontal components (right)
Medial meniscus—displaced tear
More serious injury to the medial meniscus is significantly more common later post ACL injury [1, 21, 22]. One possible explanation is that displaced flap tears or bucket handle tears of the medial meniscus may develop due to ongoing joint instability rather than occurring directly at time of initial injury. Bucket handle tears are recognised by a combination of findings (Fig. 5).
Medial meniscus bucket handle tears. Coronal PD images of left knees in three teenagers show (a) normal medial meniscal body, (b, c) bucket handle tears. In b and c, the straight arrows point to irregular, torn medial meniscal body which is smaller than normal, and the curved arrows show the flipped portion of the medial meniscus which appears as an unexpected low signal structure below the PCL in the intercondylar region. This is the “bucket-handle”, which connects to the remainder of the meniscus near the anterior and posterior attachments
Posterolateral corner
The posterolateral corner is an often overlooked site of soft tissue injury in patients with ACL tears. Injuries most commonly involve the popliteomeniscal fascicles (Fig. 6a, b), and the adjacent lateral meniscus (Fig. 6c) [23]. The popliteomeniscal fascicles are meniscocapsular extensions that blend with the popliteus and are considered functionally important stabilisers of the lateral meniscus, working in conjunction with the popliteus to prevent excessive lateral meniscal movement [24]. In adults, posterolateral corner injury implies a higher risk of ACL graft failure, likely due to the associated increased rotational instability [25]. This is likely also true in children but is not as well documented. Unfortunately, particularly in children these tiny structures are poorly seen, especially with motion artefact or a relatively large MRI field of view. The combination of regional oedema and non-visualisation of these tiny structures suggests, but does not confirm, a posterolateral corner injury. An abnormal superior popliteomeniscal fascicle serves as a useful clue for the detection of subtle lateral meniscal abnormalities and has been shown to be highly associated with a tear of the lateral meniscus, with reported positive predictive value 79 % and specificity 96 % [26].
Posterolateral corner on sagittal PD FS images. a Normal, with intact lateral meniscus, and superior and inferior popliteomeniscal struts (arrows). b Tear of the superior (arrow) and inferior popliteomeniscal struts, with intact meniscus but associated tibial and femoral marrow contusions. c Vertical tear of lateral meniscus (arrow), with irregular appearance of inferior popliteomeniscal strut suggesting incomplete tearing, marrow contusions similar in pattern to b, and a partly visualised lateral femoral condyle impaction fracture
Posterior lateral meniscus
The meniscofemoral ligament of Wrisberg and/or Humphrey, and rarely the oblique menisco-meniscal ligament, merge with the posterior lateral meniscus, complicating the assessment for tears. This has been well studied in adults [23, 27]. Practically speaking, if the ligament-to-meniscus attachment appears irregular or appears to extend to a slice where the fibula is also visible, a tear is likely present (Fig. 7).
Posterior lateral meniscus tear. a Sagittal PD image showing cleft between posterior third of lateral meniscus (arrow) and the meniscofemoral ligament of Wrisberg (arrowhead). These structures are normally separate medially, near the intercondylar notch (note that this slice contains the patellar tendon, curved arrow), but merge laterally. b Normal appearance on a more lateral slice, where fibular head is visible (curved arrow): the posterior lateral meniscus is a single triangular structure. c Oblique, mainly vertical undisplaced tear of the posterior lateral meniscus (arrow). The cleft is abnormal when present laterally on an image where the fibular head is visible. Note that Fig. 6c shows a displaced similar tear. d Complex tear of the same region of meniscus (arrow)
Posterior root of lateral meniscus
This portion of meniscus is difficult to assess at MRI, because the meniscus deviates abruptly anteriorly to reach its bony attachment and loses its usual triangular shape [28, 29]. In practice, the attachment is more anterior than one might expect, and if no low-signal structure can be seen directly attaching to bone, a tear is likely present (Fig. 8). A meniscal detachment in this location is important to detect because it renders the entire lateral meniscus unstable and substantially increases tibial loading, which could predispose to early osteoarthritis [30].
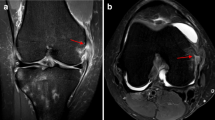
Posterior attachment of lateral meniscus. a Normal appearance on sagittal PD sequence as a low signal structure (circled), one slice lateral to its tibial spine attachment. b Increased signal and ill definition (circled), in keeping with undisplaced tearing. Note the normal meniscofemoral ligament of Wrisberg (arrow) extending across the intercondylar notch, and also the torn ACL. c Absent lateral meniscus at attachment to posterior slope of lateral intercondylar eminence (circled), with tiny low signal structures posterior to it (arrows), representing displaced meniscal flaps and meniscofemoral ligament of Wrisberg
Medial collateral ligament
Valgus positioning in most ACL injuries results in tensile stress on the medial collateral ligament, which can lead to an MCL tear (Fig. 9). For MR diagnosis, in our experience the axial sequence is more sensitive and specific than coronal sequences, where apparent ligament thickening is often due to volume averaging. The coronal plane is useful to determine location and extent of tear once diagnosed in the axial plane. The MCL was sprained (low or high grade) in 22 % of patients in a paediatric series [3]. In the last 110 cases of ACL tears at our institution, there were seven high grade MCL tears, four proximal at femoral attachment, one at midsubstance and two distal avulsions at tibial attachment. Although our numbers are small, this distribution differs from an adult series in which combined ACL and MCL ruptures more often completely tore the MCL tibial attachment (53 %) than the femoral attachment (26 %) [31]. The variation might be spurious, or due to differences in relative tension of ACL, MCL and joint capsule compared with adults. The MCL is a complex structure with two main layers visible at MRI, the superficial tibiofemoral layer and deep meniscofemoral and meniscotibial fibres firmly adherent to the medial meniscus [32]. Isolated tears of deep MCL fibres are diagnosed when the main superficial fibres are intact but no low-signal struts are visible joining the MCL to the medial meniscus. These tears can occur with ACL injury (Fig. 9b) and can also extend into the attached medial meniscus. Most MCL tears, whether involving deep and/or superficial fibres, are treated non-operatively, but it is important to recognise the location of injury within the MCL because proximal tears may adhere to the capsule and limit motion, requiring aggressive physiotherapy, while distal avulsions may require surgical intervention since the pes anserinus tendons can become entrapped between ligament and bone [33].
Medial collateral ligament on coronal PD images, reoriented as if all were left knees for comparative purposes. a Normal MCL, appearing slightly thicker proximally (arrow) than distally, which is typical. Also note the intact ACL (arrowhead). b A low-grade partial tear of deep MCL fibres including medial meniscofemoral ligament (arrow). Superficial fibres are intact (arrowhead). c High-grade sprain involving nearly the entire length of MCL; note normal appearing tibial attachment (arrow). d MCL rupture just distal to knee joint line (arrow). e A distal rupture near tibial attachment (arrow), with associated tears of deep fibres including meniscofemoral and meniscotibial ligaments (arrowheads)
Lateral femoral condyle
There is a normal shallow (less than 1.5 mm) cortical undulation in the lateral femoral condyle known as the lateral condylopatellar sulcus [34]. In the setting of ACL tear, abnormal subchondral signal (oedema acutely, and eventually sclerosis) at or near this sulcus represents contusion, while a focal angular depression together with abnormal signal indicates a fracture, at site of impaction on the lateral tibial plateau (Fig. 10). In our experience, on careful examination a focal abnormality of contour and/or signal is present in this location in most children with ACL tears, comparable to the 83 % rate reported in adults [35]. The overlying cartilage is necessarily injured to some degree, even if this is not obvious at arthroscopy or routine MRI sequences. One recent study in adults used T2 relaxation mapping to demonstrate a cartilage injury in every imaged patient with a torn ACL [36]. We expect this to also hold true in children, with unknown long-term implications.
Femoral condyle impaction injury. Panels of sagittal PD and PD FS images, in children except d. a Normal condylopatellar sulcus, a slight indentation in the condyle contour (arrows) without abnormal signal. b Contusion: subchondral marrow signal changes representing oedema (arrows), without cortical depression. c Impaction fracture: cortical depression (arrows) and oedema. Note also the large joint effusion. d Old impaction fracture: focal cortical depression and disruption (arrows), without subchondral signal change, in a 32-year-old woman who had an absent ACL and a history of prior football injury. There was also a tear of the posterior lateral meniscus, but the apparent cleft at the anterior aspect of the meniscus was a prominent transverse intermeniscal ligament rather than a tear
Tibial plateau: physis and fracture
There is often either contusion or an undisplaced fracture in subchondral bone at the lateral tibial plateau; less frequently, also at the medial tibial plateau. In teenagers this can be difficult to distinguish from a partially closed physis, especially since the site of the last portion of the physis to close is very near the most common fracture site (Fig. 11). A fracture is likely if the physis is separately visible and/or there is associated oedema. Like the femoral condyle impaction fracture, this fracture is not treated clinically, but suggests a high force impact mechanism.
Lateral tibial plateau partial fusion versus fracture. Sagittal and coronal PD images in three teens. a Normal partial closure of proximal tibial physis: similar to the distal tibial physis at the ankle, the lateral margin is last to fuse completely (arrow). Note the intact ACL. b Lateral tibial plateau fracture. On close inspection, the transverse low-signal band representing fracture (arrow) is slightly above the physis. Note also the corresponding femoral condylar impaction fracture (arrowhead). c Pseudo-fracture. On the coronal image, a transverse line just above the physis (arrow) resembles a fracture. On sagittal image, this corresponds to a point (circled), representing a vascular channel. Note the lack of visible ACL fibres, and the lateral femoral condyle impaction fracture (arrowhead)
Segond fracture
The Segond fracture is a subtle avulsion fracture from the lateral tibial plateau at the combined attachment site of the iliotibial tract and the anterior oblique band. The anterior oblique band is a capsular thickening that joins the fibular collateral ligament to the rim of the lateral tibial plateau where it merges with posterior fibres of the iliotibial tract [37]. Nearly all patients with Segond fractures have ACL tears [38] or tibial spine avulsion which is mechanically equivalent in younger children (Fig. 1). The fracture is usually produced by internal rotation and varus stress at the knee [38], which differs from the usual axial rotation/valgus mechanism of ACL tears, likely accounting for its relative rarity. It is subtle on both MRI and radiographs.
Other injuries
A discoid lateral meniscus is particularly prone to tear in association with an ACL tear (Fig. 12). As for the medial meniscus, it is our experience that bucket handle tears of the lateral meniscus are unusual in the early post injury period and more common months or years post untreated ACL tear. Lateral collateral ligament sprains are not expected with valgus ACL injury mechanism. Posterior cruciate ligament sprains in this setting generally indicate higher impact forces than associated with sports injury, such as motor vehicle collisions. Patellar dislocation or vascular injury are also rarely associated with ACL tears. As noted at the lateral femoral condyle, cartilage-specific sequences in adults show cartilage injury to be essentially always present in patients with ACL tears, even if often not obvious on routinely obtained MRI sequences [36]. We are not aware of a study confirming this in children.
Summary
This review demonstrates the spectrum of associated findings expected in paediatric ACL injury. Paediatric-specific issues for the radiologist to be aware of include: tibial spine avulsion instead of ACL rupture; a thin but intact ACL; normal poor visualisation of posterolateral corner structures; differentiation between incompletely closed physis and impaction fracture. The posterior lateral meniscus is particularly complex and should be studied in three regions (posterolateral corner, meniscofemoral ligament attachment and bony attachment). If an ACL tear is detected, the associated findings described here should be specifically sought and, conversely, observing one of these findings should increase the suspicion for an ACL tear.
It is important for the interpreting physician to remember that ACL tears are not isolated events, but only the most obvious sign of a complex knee injury involving multiple structures. A child with an ACL tear has a lifetime of loading ahead, and for optimal planning of surgical treatment and prediction of long-term clinical outcome, the radiologist should report the ACL tear with an integrated description of associated findings implying the likely injury mechanism.
References
Dumont GD, Hogue GD, Padalecki JR, Okoro N, Wilson PL (2012) Meniscal and chondral injuries associated with pediatric anterior cruciate ligament tears: relationship of treatment time and patient-specific factors. Am J Sports Med 40(9):2128–2133
Ahlden M, Samuelsson K, Sernert N, Forssblad M, Karlsson J, Kartus J (2012) The swedish national anterior cruciate ligament register: a report on baseline variables and outcomes of surgery for almost 18,000 patients. Am J Sports Med 40(10):2230–2235
Prince JS, Laor T, Bean JA (2005) MRI of anterior cruciate ligament injuries and associated findings in the pediatric knee: changes with skeletal maturation. AJR Am J Roentgenol 185(3):756–762
Remer EM, Fitzgerald SW, Friedman H, Rogers LF, Hendrix RW, Schafer MF (1992) Anterior cruciate ligament injury: MR imaging diagnosis and patterns of injury. Radiographics 12(5):901–915
Ireland ML (1999) Anterior cruciate ligament injury in female athletes: epidemiology. J Athl Train 34(2):150–154
Sanders TG, Medynski MA, Feller JF, Lawhorn KW (2000) Bone contusion patterns of the knee at MR imaging: footprint of the mechanism of injury. Radiographics 20(Spec No):S135–S151
Lee K, Siegel MJ, Lau DM, Hildebolt CF, Matava MJ (1999) Anterior cruciate ligament tears: MR imaging-based diagnosis in a pediatric population. Radiology 213(3):697–704
Bere T, Florenes TW, Krosshaug T et al (2011) Mechanisms of anterior cruciate ligament injury in world cup alpine skiing: a systematic video analysis of 20 cases. Am J Sports Med 39(7):1421–1429
MacMahon PJ, Palmer WE (2011) A biomechanical approach to MRI of acute knee injuries. AJR Am J Roentgenol 197(3):568–577
Zobel MS, Borrello JA, Siegel MJ, Stewart NR (1994) Pediatric knee MR imaging: pattern of injuries in the immature skeleton. Radiology 190(2):397–401
King SJ (1997) Magnetic resonance imaging of knee injuries in children. Eur Radiol 7(8):1245–1251
Munshi M, Davidson M, MacDonald PB, Froese W, Sutherland K (2000) The efficacy of magnetic resonance imaging in acute knee injuries. Clin J Sport Med 10(1):34–39
Major NM, Beard LN Jr, Helms CA (2003) Accuracy of MR imaging of the knee in adolescents. AJR Am J Roentgenol 180(1):17–19
Ho-Fung VM, Jaimes C, Jaramillo D (2011) MR imaging of ACL injuries in pediatric and adolescent patients. Clin Sports Med 30(4):707–726
Stevens KJ, Dragoo JL (2006) Anterior cruciate ligament tears and associated injuries. Top Magn Reson Imaging 17(5):347–362
Bales CP, Guettler JH, Moorman CT 3rd (2004) Anterior cruciate ligament injuries in children with open physes: evolving strategies of treatment. Am J Sports Med 32(8):1978–1985
Amis AA (2012) The functions of the fibre bundles of the anterior cruciate ligament in anterior drawer, rotational laxity and the pivot shift. Knee Surg Sports Traumatol Arthrosc 20(4):613–620
Van Dyck P, De Smet E, Veryser J et al (2012) Partial tear of the anterior cruciate ligament of the knee: injury patterns on MR imaging. Knee Surg Sports Traumatol Arthrosc 20(2):256–261
Chan KK, Resnick D, Goodwin D, Seeger LL (1999) Posteromedial tibial plateau injury including avulsion fracture of the semimembranous tendon insertion site: ancillary sign of anterior cruciate ligament tear at MR imaging. Radiology 211(3):754–758
De Smet AA, Nathan DH, Graf BK, Haaland BA, Fine JP (2008) Clinical and MRI findings associated with false-positive knee MR diagnoses of medial meniscal tears. AJR Am J Roentgenol 191(1):93–99
Millett PJ, Willis AA, Warren RF (2002) Associated injuries in pediatric and adolescent anterior cruciate ligament tears: does a delay in treatment increase the risk of meniscal tear? Arthroscopy 18(9):955–959
Lawrence JT, Argawal N, Ganley TJ (2011) Degeneration of the knee joint in skeletally immature patients with a diagnosis of an anterior cruciate ligament tear: is there harm in delay of treatment? Am J Sports Med 39(12):2582–2587
Laundre BJ, Collins MS, Bond JR, Dahm DL, Stuart MJ, Mandrekar JN (2009) MRI accuracy for tears of the posterior horn of the lateral meniscus in patients with acute anterior cruciate ligament injury and the clinical relevance of missed tears. AJR Am J Roentgenol 193(2):515–523
Peduto AJ, Nguyen A, Trudell DJ, Resnick DL (2008) Popliteomeniscal fascicles: anatomic considerations using MR arthrography in cadavers. AJR Am J Roentgenol 190(2):442–448
Vinson EN, Major NM, Helms CA (2008) The posterolateral corner of the knee. AJR Am J Roentgenol 190(2):449–458
Blankenbaker DG, De Smet AA, Smith JD (2002) Usefulness of two indirect MR imaging signs to diagnose lateral meniscal tears. AJR Am J Roentgenol 178(3):579–582
Vahey TN, Bennett HT, Arrington LE, Shelbourne KD, Ng J (1990) MR imaging of the knee: pseudotear of the lateral meniscus caused by the meniscofemoral ligament. AJR Am J Roentgenol 154(6):1237–1239
De Smet AA, Mukherjee R (2008) Clinical, MRI, and arthroscopic findings associated with failure to diagnose a lateral meniscal tear on knee MRI. AJR Am J Roentgenol 190(1):22–26
De Smet AA, Blankenbaker DG, Kijowski R, Graf BK, Shinki K (2009) MR diagnosis of posterior root tears of the lateral meniscus using arthroscopy as the reference standard. AJR Am J Roentgenol 192(2):480–486
Schillhammer CK, Werner FW, Scuderi MG, Cannizzaro JP (2012) Repair of lateral meniscus posterior horn detachment lesions: a biomechanical evaluation. Am J Sports Med 40(11):2604–2609
Noyes FR, Barber-Westin SD (1995) The treatment of acute combined ruptures of the anterior cruciate and medial ligaments of the knee. Am J Sports Med 23(4):380–389
De Maesenner M, Van Roy F, Lenchik L, Barbaix E, De Ridder F, Osteaux M (2000) Three layers of the medial capsular and supporting structures of the knee: MR imaging-anatomic correlation. Radiographics 20(Spec):S83–S89
Robins AJ, Newman AP, Burks RT (1993) Postoperative return of motion in anterior cruciate ligament and medial collateral ligament injuries. The effect of medial collateral ligament rupture location. Am J Sports Med 21(1):20–25
Pao DG (2001) The lateral femoral notch sign. Radiology 219(3):800–801
Speer KP, Spritzer CE, Bassett FH 3rd, Feagin JA Jr, Garrett WE Jr (1992) Osseous injury associated with acute tears of the anterior cruciate ligament. Am J Sports Med 20(4):382–389
Potter HG, Jain SK, Ma Y, Black BR, Fung S, Lyman S (2012) Cartilage injury after acute, isolated anterior cruciate ligament tear: immediate and longitudinal effect with clinical/MRI follow-up. Am J Sports Med 40(2):276–285
Gottsegen CJ, Eyer BA, White EA, Learch TJ, Forrester D (2008) Avulsion fractures of the knee: imaging findings and clinical significance. Radiographics 28(6):1755–1770
Campos JC, Chung CB, Lektrakul N et al (2001) Pathogenesis of the segond fracture: anatomic and MR imaging evidence of an iliotibial tract or anterior oblique band avulsion. Radiology 219(2):381–386
Conflict of interest
The authors declare no conflict of interest. No funding was received for this work. Institutional Review Board approval was obtained.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Jaremko, J.L., Guenther, Z.D., Jans, L.B.O. et al. Spectrum of injuries associated with paediatric ACL tears: an MRI pictorial review. Insights Imaging 4, 273–285 (2013). https://doi.org/10.1007/s13244-013-0250-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13244-013-0250-z