Abstract
Introduction and Hypothesis
The objective was to develop a prediction model for urinary tract infection (UTI) after pelvic surgery.
Methods
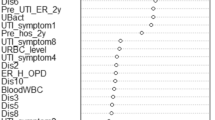
We utilized data from three tertiary care centers of women undergoing pelvic surgery. The primary outcome was a UTI within 8 weeks of surgery. Additional variables collected included procedural data, severity of prolapse, use of mesh, anti-incontinence surgery, EBL, diabetes, steroid use, estrogen use, postoperative catheter use, PVR, history of recurrent UTI, operative time, comorbidities, and postoperative morbidity including venous thromboembolism, surgical site infection. Two datasets were used for internal validation, whereas a third dataset was used for external validation. Algorithms that tested included the following: multivariable logistic regression, decision trees (DTs), naive Bayes (NB), random forest (RF), gradient boosting (GB), and multilayer perceptron (MP).
Results
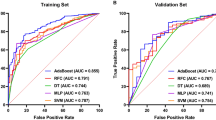
For the training dataset, containing both University of British Columbia and Mayo Clinic Rochester data, there were 1,657 patients, with 172 (10.4%) UTIs; whereas for the University of Calgary external validation data, there were a total of 392 patients with a UTI rate of 16.1% (n = 63). All models performed well; however, the GB, DT, and RF models all had an area under the curve (AUC) > 0.97. With external validation the model retained high discriminatory ability, DT: AUC = 0.88, RF: AUC = 0.88, and GB: AUC = 0.90.
Conclusions
A model with high discriminatory ability can predict UTI within 8 weeks of pelvic surgery. Future studies should focus on prospective validation and application of randomized trial models to test the utility of this model in the prevention of postoperative UTI.

Similar content being viewed by others
Data Availability
The data that support the findings of this study are available on request from the corresponding author, [DS], and pending approval from co-investigators. The data are not publicly available due to presence of protected health information.
References
Klevens RM, Edwards JR, Richards CL Jr, Horan TC, Gaynes RP, Pollock DA, Cardo DM. Estimating health care-associated infections and deaths in U.S. hospitals, 2002. Public Health Rep. 2007;122(2):160–6. https://doi.org/10.1177/003335490712200205.
Scott RD. The direct medical costs of healthcare-associated infections in U.S. Hospitals and the benefits of prevention. Accessed 1 June 2023
El-Nashar SA, Singh R, Schmitt JJ, et al. Urinary tract infection after hysterectomy for benign gynecologic conditions or pelvic reconstructive surgery. Obstet Gynecol. 2018;132(6):1347–57. https://doi.org/10.1097/AOG.0000000000002931.
Sutkin G, Alperin M, Meyn L, Wiesenfeld HC, Ellison R, Zyczynski HM. Symptomatic urinary tract infections after surgery for prolapse and/or incontinence. Int Urogynecol J. 2010;21:955–61.
Wei JT, Nygaard I, Richter HE, et al. A midurethral sling to reduce incontinence after vaginal prolapse repair. N Engl J Med. 2012;366:2358–67.
Fok CS, McKinley K, Mueller ER, et al. Day of surgery urine cultures identify urogynecologic patients at increased risk for postoperative urinary tract infection. J Urol. 2013;189:1721–4.
Falagas ME, Athanasiou S, Iavazzo C, Tokas T, Antsaklis A. Urinary tract infections after pelvic floor gynecological surgery: prevalence and effect of antimicrobial prophylaxis. A systematic review. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(8):1165–1172.
Beeler C, Dbeibo L, Yeap YL, et al. Real world utilization of nurse-driven urinary catheter removal protocol in patients with epidural pain catheters. Am J Infect Control. 2022;50(4):396–9. https://doi.org/10.1016/j.ajic.2021.09.011.
Sanaee MS, Hutcheon JA, Larouche M, Brown HL, Lee T, Geoffrion R. Urinary tract infection prevention after midurethral slings in pelvic floor reconstructive surgery: a systematic review and meta-analysis. Acta Obstet Gynecol Scand. 2019;98(12):1514–22. https://doi.org/10.1111/aogs.13661.
Dieter AA, Amundsen CL, Edenfield AL, et al. Oral antibiotics to prevent postoperative urinary tract infection. Obstet Gynecol. 2014;123(1):96–103. https://doi.org/10.1097/AOG.0000000000000024.
Foxman B, Cronenwett AE, Spino C, Berger MB, Morgan DM. Cranberry juice capsules and urinary tract infection after surgery: results of a randomized trial. Am J Obstet Gynecol. 2015;213(2):194.e1–8. https://doi.org/10.1016/j.ajog.2015.04.003.
Mooren ES, Liefers WJ, de Leeuw JW. Cranberries after pelvic floor surgery for urinary tract infection prophylaxis: a randomized controlled trial. Neurourol Urodyn. 2020;39(5):1543–9. https://doi.org/10.1002/nau.24391.
Collins GS, Reitsma JB, Altman DG, Moons KG. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. BMC Med. 2015;13(1):1.
Luo W, Phung D, Tran T, et al. Guidelines for developing and reporting machine learning predictive models in biomedical research: a multidisciplinary view. J Med Internet Res. 2016;18(12):e323.
Sanaee MS, Pan K, Lee T, Koenig NA, Geoffrion R. Urinary tract infection after clean-contaminated pelvic surgery: a retrospective cohort study and prediction model. Int Urogynecol J. 2020;31(9):1821–8. https://doi.org/10.1007/s00192-019-04119-0.
Gould CV, Umscheid CA, Agarwal RK, Kuntz G, Pegues DA. Healthcare Infection Control Practices Advisory Committee. Guideline for prevention of catheter-associated urinary tract infections 2009. Infect Control Hosp Epidemiol. 2010;31(4):319–26. https://doi.org/10.1086/651091.
Riley RD, Ensor J, Snell KIE, et al. Calculating the sample size required for developing a clinical prediction model. BMJ. 2020;18(368):m441. https://doi.org/10.1136/bmj.m441.
Thomas-White KJ, Gao X, Lin H, et al. Urinary microbes and postoperative urinary tract infection risk in urogynecologic surgical patients. Int Urogynecol J. 2018;29(12):1797–805. https://doi.org/10.1007/s00192-018-3767-3.
Flanagan JM, Read C, Shindul-Rothschild J. Factors associated with the rate of sepsis after surgery. Crit Care Nurse. 2020;40(5):e1–9. https://doi.org/10.4037/ccn2020171.
Agency for Healthcare Research and Quality. Estimating the additional hospital inpatient cost and mortality associated with selected hospital-acquired conditions. https://www.ahrq.gov/hai/pfp/haccost2017-results.html. Accessed 14 July 2023.
Centers for Disease Control and Prevention. Catheter associated urinary tract infections (CAUTI). https://www.cdc.gov/infectioncontrol/guidelines/cauti/index.html. Accessed 14 July 2023.
Burke JP. Infection control—a problem for patient safety. N Engl J Med. 2003;348(7):651–6. https://doi.org/10.1056/NEJMhpr020557.
Centers for Disease Control and Prevention. 2021 Urinary tract infection protocol change. https://www.cdc.gov/nhsn/pdfs/training/2021/uti-508.pdf. Accessed 15 July 2023.
Author information
Authors and Affiliations
Contributions
S. Yurick: project development, model development, manuscript writing; S. Ray: model development, manuscript writing; D. Sheyn: project development, model development, data collection, model development, manuscript writing; S. El-Nashar: data collection, manuscript writing, manuscript editing; E. Brennand: data collection, manuscript writing; S. Kim-Fine: data collection, manuscript writing; M. Sanaee: manuscript writing, manuscript editing; S. Regan: manuscript writing, manuscript editing; R. Geoffrion: data collection, manuscript writing; J. Occhino: data collection, manuscript writing; A. Hijaz: manuscript writing, manuscript editing.
Corresponding author
Ethics declarations
Conflicts of Interest
None.
Additional information
Handling Editor: G.Alessandro Digesu
Editor in Chief: Maria A. Bortolini
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yurick, S., Ray, S., El-Nashar, S. et al. Prediction of Postoperative Urinary Tract Infection Following Benign Gynecologic Surgery. Int Urogynecol J (2024). https://doi.org/10.1007/s00192-024-05773-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00192-024-05773-9