Abstract
Introduction and hypothesis
Fecal incontinence (FI) has two primary subtypes: urgency fecal incontinence (UFI) and passive fecal leakage (PFL). The pathophysiology underlying the subtypes is incompletely understood.
Objectives
To compare the bowel habits, physical examinations and pelvic floor anatomical defects in patients with UFI-dominant FI versus patients with PFL-dominant FI.
Study design
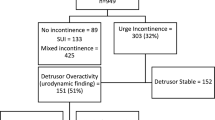
This is a retrospective cross-sectional study of female patients who presented with fecal incontinence symptoms to our tertiary urogynecology center. All subjects underwent a comprehensive history, physical examination, 3D-static pelvic floor ultrasound, and 2D-dynamic ultrasound of the posterior compartment. Patients with UFI-dominant FI were compared to patients with PFL-dominant FI.
Results
One hundred forty-five patients were included in the analysis; 57 categorized as UFI-dominant FI, 69 PFL-dominant FI and 19 categorized as having “both” leakage patterns. In comparing bowel habits, patient with UFI-dominant FI had more frequent bowel movements (15.5 ± SD 13.0/week vs. 10.9 ± SD 7.6 /week, p = 0.022) and were more likely to have loose stools (48.2% vs. 26.1%, p = 0.01). No statistically significant differences were observed in the prevalence of external anal sphincter defect (11.3% vs. 17.2%, p = 0.38) or internal anal sphincter defect (11.3% vs. 19%, p = 0.26) between groups. Finally, patients with UFI-dominant FI had a higher incidence of rectal hypermobility (loss of rectal support on Valsalva) (58% vs. 36.9%, p = 0.025).
Conclusion
Patients with urge-predominant FI have increased frequency of bowel movements, looser stools, and increased rectal folding diagnosed via dynamic ultrasound as compared to patients with passive-dominant FI.



Similar content being viewed by others
References
Bharucha AE, Zinsmeister AR, Locke GR, Seide BM, McKeon K, Schleck CD, et al. Prevalence and burden of fecal incontinence: a population-based study in women. Gastroenterology. 2005;129:42–9. https://doi.org/10.1053/j.gastro.2005.04.006.
Sharma A, Yuan L, Marshall RJ, Merrie AEH, Bissett IP. Systematic review of the prevalence of faecal incontinence. Br J Surg. 2016;103:1589–97. https://doi.org/10.1002/bjs.10298.
Whitehead WE, Borrud L, Goode PS, Meikle S, Mueller ER, Tuteja A, et al. Fecal incontinence in US adults: epidemiology and risk factors. Gastroenterology. 2009;137:512–7, 517.e1–2. https://doi.org/10.1053/j.gastro.2009.04.054.
Bezerra LRPS, Vasconcelos Neto JA, Vasconcelos CTM, Karbage SAL, Lima AC, Frota IPR, et al. Prevalence of unreported bowel symptoms in women with pelvic floor dysfunction and the impact on their quality of life. Int Urogynecology J. 2014;25:927–33. https://doi.org/10.1007/s00192-013-2317-2.
Rao SSC. Pathophysiology of adult fecal incontinence. Gastroenterology. 2004;126:S14–22. https://doi.org/10.1053/j.gastro.2003.10.013.
Pahwa AK, Khanijow KD, Harvie HS, Arya LA, Andy UU. Comparison of patient impact and clinical characteristics between urgency and passive fecal incontinence phenotypes. Female Pelvic Med Reconstr Surg. 2018. https://doi.org/10.1097/SPV.0000000000000603.
Hotouras A, Thaha MA, Boyle DJ, Allison ME, Currie A, Knowles CH, et al. Short-term outcome following percutaneous tibial nerve stimulation for faecal incontinence: a single-Centre prospective study. Colorectal Dis Off J Assoc Coloproctology G B Irel. 2012;14:1101–5. https://doi.org/10.1111/j.1463-1318.2011.02906.x.
Kamm MA. Faecal incontinence. BMJ. 1998;316:528–32. https://doi.org/10.1136/bmj.316.7130.528.
Engel AF, Kamm MA, Bartram CI, Nicholls RJ. Relationship of symptoms in faecal incontinence to specific sphincter abnormalities. Int J Color Dis. 1995;10:152–5. https://doi.org/10.1007/BF00298538.
Rostaminia G, White D, Quiroz LH, Shobeiri SA. 3D pelvic floor ultrasound findings and severity of anal incontinence. Int Urogynecology J. 2014;25:623–9. https://doi.org/10.1007/s00192-013-2278-5.
Rostaminia G, Abramowitch S, Chang C, Goldberg RP. Descent and hypermobility of the rectum in women with obstructed defecation symptoms. Int Urogynecology J. 2020;31:337–49. https://doi.org/10.1007/s00192-019-03934-9.
Barber MD, Kuchibhatla MN, Pieper CF, Bump RC. Psychometric evaluation of 2 comprehensive condition-specific quality of life instruments for women with pelvic floor disorders. Am J Obstet Gynecol. 2001;185:1388–95. https://doi.org/10.1067/mob.2001.118659.
van Delft KWM, Sultan AH, Thakar R, Shobeiri SA, Kluivers KB. Agreement between palpation and transperineal and endovaginal ultrasound in the diagnosis of levator ani avulsion. Int Urogynecology J. 2015;26:33–9. https://doi.org/10.1007/s00192-014-2426-6.
Shobeiri SA, Chesson RR, Gasser RF. The internal innervation and morphology of the human female levator ani muscle. Am J Obstet Gynecol. 2008;199:686.e1–6. https://doi.org/10.1016/j.ajog.2008.07.057.
Routzong MR, Abramowitch SD, Chang C, Goldberg RP, Rostaminia G. Obstructed defecation symptom severity and degree of rectal hypermobility and folding detected by dynamic ultrasound. Ultrasound Q Publish Ahead of Print. 2021. https://doi.org/10.1097/RUQ.0000000000000565.
Chan CLH, Scott SM, Williams NS, Lunniss PJ. Rectal hypersensitivity worsens stool frequency, urgency, and lifestyle in patients with urge fecal incontinence. Dis Colon Rectum. 2005;48:134–40. https://doi.org/10.1007/s10350-004-0774-x.
Hawkins AT, Olariu AG, Savitt LR, Gingipally S, Wakamatsu MM, Pulliam S, et al. Impact of rising grades of internal rectal intussusception on fecal continence and symptoms of constipation. Dis Colon Rectum. 2016;59:54–61. https://doi.org/10.1097/DCR.0000000000000510.
Yagi Y, Tsunoda A, Takahashi T, Kusanagi H. Rectoanal intussusception is very common in patients with fecal incontinence. J Anus Rectum Colon. 2018;2:162–7. https://doi.org/10.23922/jarc.2017-048.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pincus, J.B., Moss, N.P., Chang, C. et al. Pelvic floor architectural defects in female patients with urge fecal incontinence versus passive fecal leakage: a dynamic ultrasound study. Int Urogynecol J 33, 2133–2141 (2022). https://doi.org/10.1007/s00192-021-04919-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-04919-3