Abstract
Background
A phase II clinical trial was conducted on colorectal cancer patients with only liver metastases (focal diameter exceeds 5 cm or the number of liver metastases is ≥5; H2·H3) to evaluate the liver resection rate and safety after 6 cycles of mFOLFOX6+bevacizumab (BV) therapy.
Methods
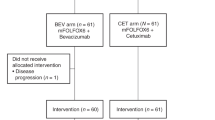
mFOLFOX6+BV therapy was applied for 6 cycles to the patients with H2·H3 liver only metastasis. Hepatectomy was considered after the sixth cycle as a rule, and was performed if possible. The primary endpoint was the curative hepatectomy rate (R0 resection rate).
Results
Forty-six patients were registered and 45 patients were included in the efficacy analysis. Of the 19 patients rated as unresectable before therapy, 18 completed 6 cycles of mFOLFOX6+BV therapy and subsequently underwent hepatectomy (16 were R0-resected). Of the 26 initially unresectable patients, 6 underwent hepatectomy (4 were RO-resected). The overall R0 resection rate was 44.4% (20/45). Chemotherapy-associated grade 3 or higher adverse events included neutrophil decreased (17.4%) and leukocyte decreased (8.7%), fatigue (6.5%) etc. Only hypertension (6.5%) and venous thromboembolism (2.2%) were BV-associated grade 3 or higher adverse events. Among the 25 patients who underwent hepatectomy, intraoperative/postoperative complications included grade 3 wound infections (2 cases), biloma, delayed wound healing and intraperitoneal abscess (each 1 case).
Conclusions
In colorectal cancer patients with liver-only metastases, mFOLFOX6+ BV therapy yielded a high hepatectomy rate and a high percentage of initially unresectable and subsequently resectable cases. The chemotherapy associated adverse events and hepatectomy complications were both within acceptable ranges.


Similar content being viewed by others
References
Watanabe T, Itabashi M, Shimada Y, et al. Japanese Society for Cancer of the Colon and Rectum: Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2010 for the treatment of colorectal cancer. Int J Clin Oncol. 2012;17:1–29.
Sugihara K, Uetake H. Therapeutic strategies for hepatic metastasis of colorectal cancer: overview. J Hepatobiliary Pancreat Sci. 2012;19:523–7.
Japanese Classification of Colorectal Carcinoma. Japanese society of cancer of the colon and rectum. Tokyo: Kanehara-Shuppan; 2009. p. 11.
Kato T, Yasui K, Hirai T, et al. Therapeutic results for hepatic metastasis of colorectal cancer with special reference to effectiveness of hepatectomy: analysis of prognostic factors for 763 cases recorded at 18 institutions. Dis Colon Rectum. 2003;46:S22–31.
Tournigand C, André T, Achille E, et al. FOLFIRI followed by FOLFOX6 or the reverse sequence in advanced colorectal cancer: a randomized GERCOR study. J Clin Oncol. 2004;22:229–37.
Hurwitz H, Fehrenbacher L, Novotny W, et al. Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med. 2004;350:2335–42.
Saltz LB, Clarke S, Díaz-Rubio E, et al. Bevacizumab in combination with oxaliplatin-based chemotherapy as first-line therapy in metastatic colorectal cancer: a randomized phase III study. J Clin Oncol. 2008;26:2013–9.
Van Cutsem E, Köhne CH, Hitre E, et al. Cetuximab and chemotherapy as initial treatment for metastatic colorectal cancer. N Engl J Med. 2009;360:1408–17.
Bokemeyer C, Bondarenko I, Makhson A, et al. Fluorouracil, leucovorin, and oxaliplatin with and without cetuximab in the first-line treatment of metastatic colorectal cancer. J Clin Oncol. 2009;27:663–71.
Douillard JY, Siena S, Cassidy J, et al. Randomized, phase III trial of panitumumab with infusional fluorouracil, leucovorin, and oxaliplatin (FOLFOX4) versus FOLFOX4 alone as first-line treatment in patients with previously untreated metastatic colorectal cancer: the PRIME study. J Clin Oncol. 2010;28:4697–705.
Nordlinger B, Sorbye H, Glimelius B, et al; EORTC Gastro-Intestinal Tract Cancer Group; Cancer Research UK; Arbeitsgruppe Lebermetastasen und-tumoren in der Chirurgischen Arbeitsgemeinschaft Onkologie (ALM-CAO); Australasian Gastro-Intestinal Trials Group (AGITG); Fédération Francophone de Cancérologie Digestive (FFCD). Perioperative chemotherapy with FOLFOX4 and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC Intergroup trial 40983): a randomised controlled trial. Lancet. 2008;371:1007–16.
Adam R, Delvart V, Pascal G, et al. Rescue surgery for unresectable colorectal liver metastases downstaged by chemotherapy: a model to predict long-term survival. Ann Surg. 2004;240:644–57.
Folprecht G, Gruenberger T, Bechstein WO, et al. Tumour response and secondary resectability of colorectal liver metastases following neoadjuvant chemotherapy with cetuximab: the CELIM randomised phase 2 trial. Lancet Oncol. 2010;11:38–47.
Folprecht G, Gruenberger T, Bechstein W, et al. Cetuximab and chemotherapy in the treatment of patients with initially “non-resectable” colorectal (CRC) liver metastases—long term follow up of the CELIM trial. J Clin Oncol. 2013;31:abstr 3538.
Wong R, Cunningham D, Barbachano Y, et al. A multicentre study of capecitabine, oxaliplatin plus bevacizumab as perioperative treatment of patients with poor-risk colorectal liver-only metastases not selected for upfront resection. Ann Oncol. 2011;22:2042–8.
Garufi C, Torsello A, Tumolo S, et al. Cetuximab plus chronomodulated irinotecan, 5-fluorouracil, leucovorin and oxaliplatin as neoadjuvant chemotherapy in colorectal liver metastases: POCHER trial. Br J Cancer. 2010;103:1542–7.
Common Terminology Criteria for Adverse Events v3.0 (CTCAE). 2006. http://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/ctcaev3.pdf#search=‘Common+Terminology+Criteria+for+Adverse+Events+v3.0+ %28CTCAE %29′. Accessed 14 Nov 2014.
Nordlinger B, Van Cutsem E, Gruenberger T, et al; European Colorectal Metastases Treatment Group; Sixth International Colorectal Liver Metastases Workshop. Combination of surgery and chemotherapy and the role of targeted agents in the treatment of patients with colorectal liver metastases: recommendations from an expert panel. Ann Oncol. 2009;20:985–92.
Acknowledgment
The authors express their gratitude to the 25 facilities for their cooperation with case registration.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Uetake, H., Yasuno, M., Ishiguro, M. et al. A Multicenter Phase II Trial of mFOLFOX6 Plus Bevacizumab to Treat Liver-Only Metastases of Colorectal Cancer that are Unsuitable for Upfront Resection (TRICC0808). Ann Surg Oncol 22, 908–915 (2015). https://doi.org/10.1245/s10434-014-4094-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-014-4094-7