Abstract
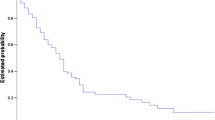
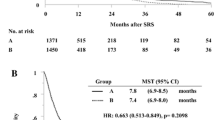
The risk of brain recurrence after whole-brain radiotherapy for metastatic disease has been infrequently reported, but quoted to be as high as 50%. These values are in the context of autopsy series or clinical trials and thus may not represent experience in routine clinical practice. This retrospective analysis was undertaken: (1) to confirm recursive analysis-based prognostic factors contributing to survival; and (2) to investigate efficacy of Gamma Knife Stereotactic Radiosurgery (GKSRS) in the poorest prognosis population. The records of 85 unselected, consecutive patients receiving whole-brain radiotherapy for brain metastases at Naval Medical Center San Diego were analyzed. Median dose of whole brain radiotherapy was 30 Gy in 10 fractions. These records were categorized by Radiation Therapy Oncology Group (RTOG) categories based on several prognostic factors. Further, analysis of 153 consecutive patients (178 treatments of 396 lesions) receiving GKSRS at the San Diego Gamma Knife Center was made for patients with Karnofsky Performance Status (KPS) < 70 (RTOG class 3). Twenty patients were identified. Median dose of GKSRS was 17.5 Gy at the 61% mean isodose line for all GKSRS patients. Six patients experienced clinical brain recurrences after whole-brain radiotherapy; the actuarial risk of clinical brain recurrence after whole-brain radio therapy approached 30% at 3 years, although few patients survived this long. Survival of patients after whole brain radiotherapy alone by RTOG category mirrored findings of other centers. Patients in class 3 (n = 26) had a median survival in our population of 59 days. For the 20 GKSRS patients with similar performance status and clinical follow-up, the median survival was longer, but not significantly so (162 days; p = 0.467). In the off-protocol setting, clinical brain recurrence of metastatic disease after whole-brain radiotherapy occurs not infrequently in patients with otherwise long survival. The RTOG criteria well describes an extremely poor-prognosis group of patients for whom the single fraction of stereotactic radiosurgery may optimize palliation as well as or better than longer courses of conventional palliative radiotherapy.
Similar content being viewed by others
REFERENCES
Wright DC; DeLaney TF; Buckner JC: Treatment of Metastatic Cancer. In DeVita VT, Hellman S, Rosenberg SA (eds), Cancer, Principles and Practice of Oncology 4th edn., Philadelphia, J.B. Lippincott, 1993, pp. 2170–2261
Gaspar L, Scott C, Rotman M, Asbell S, Phillips T, Wasserman T, McKenna WG, Byhardt R: Recursive partitioning analysis (RPA) of prognostic factors in three Radiation Therapy Oncology Group (RTOG) brain metastases trials. Intern J Radiat Oncol Biol Phys. 37:745–751, 1997
Johnson JD, Young B: Demographics of brain metastases. Neurosurg Clin N Amer 7:337–344, 1996
Borgelt B, Gelber R, Kramer S, Brady LW, Chang CH, Davis LW, Perez CA, Hendrickson FR: The palliation of brain metastases: Final results of the first two studies by the Radiation Therapy Oncology Group. Intern J Radiat Oncol Biol Phys 6:1–9, 1980
Agboola O, Benoit B, Cross C, Da Silva V, Esche B, Lesiuk H, Gonsalves C, Prognostic factors derived from recursive partitioning analysis (RPA)of Radiation Therapy Oncology Group (RTOG) brain metastases trials applied to surgically resected and irradiated brain metastastic cases. Intern J Radiat Oncol Biol Phys 42:155–159, 1998
Mehta M, Noyes, W, Craig B, Lamond J, Auchter R, French M, Johnson M, Levin A, Badie B, Robbins I, Kinsella T: A cost-effectiveness and cost-utility analysis of radiosurgery vs. resection for single-brain metastases. Intern J Radiat Oncol Biol Phys 39:445–454, 1997
Flickinger JC, Kondziolka D, Lundsford LD, Coffey RJ, Goodman ML, Shaw EG, Hudgins WR, Weiner R, Harsh GR, Sneed PK, Larson DA: A multi-institutional experience with stereotactic radiosurgery for solitary brain metastases. Intern J Radiat Oncol Biol Phys 28:797–802, 1994
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Johnstone, P.A.S., Dos Santos, F.M., Kent, C.S. et al. Poor-Prognosis Patients with Cancer Metastatic to Brain: Implications for Stereotactic Radiosurgery. Journal of Radiosurgery 3, 85–89 (2000). https://doi.org/10.1023/A:1009585601810
Issue Date:
DOI: https://doi.org/10.1023/A:1009585601810