Abstract
Study design
This study is a single-center retrospective radiographic review.
Objectives
The objective of this study is to evaluate a novel measurement parameter, mandibular slope (MS), as a measure of horizontal gaze.
Introduction
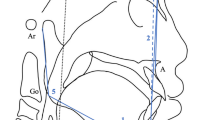
Assessment of sagittal spinal alignment is essential in the evaluation of spinal deformity patients. Ability to achieve a horizontal gaze, a parameter of sagittal alignment, is needed for the performance of daily activities. Standard measures of horizontal gaze, including the gold-standard chin–brow to vertical angle (CBVA) and the surrogate measures McGregor’s line (McGS) and Chamberlain’s line (CS), require high-quality imaging, precise head positioning, and reliance on difficult to view visual landmarks. A novel measurement parameter, MS, utilizing the caudal margin of the mandible on standard lateral spine radiographs is proposed.
Methods
90 radiographs from spine deformity patients with or without spinal implants from a single center were evaluated. Three spine surgery fellows independently measured CBVA, McGS, CS, and MS at two timepoints at least one week apart to assess accuracy and reliability. MS was measured as the angle created by the inferior edge of the mandibular body and the horizontal. Formulas for calculating CBVA based on the above parameters were derived and compared to the actual CBVA.
Results
Mean age was 49.7 years, 76 females and 14 males. CBVA correlated with CS, McGS, and MS, r = 0.85, 0.81, and 0.80, respectively (p < 0.001). Standard error between real CBVA and calculated CBVA using CS (0.4 ± 4.79) and McGS (0.4 ± 3.9) was higher than that calculated using MS (− 0.2 ± 4.3). ICC demonstrated the highest inter-observer reliability with MS (0.999). MS had the highest intra-observer reliabilities 0.975, 0.981, and 0.988 (p < 0.001); CS and McGS also demonstrated high intra-observer reliability.
Conclusions
MS is a promising measure of horizontal gaze that correlates highly with CBVA, has excellent intra- and inter-observer reliability with CBVA, and is easily measured using standard lateral spine radiographs.





Similar content being viewed by others
References
Schwab FJ, Patel A, Ungar B et al (2010) adult spinal deformity—postoperative standing imbalance. How much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine 35:2224–2231
Schwab FJ, Lafage V, Patel A et al (2009) Sagittal plane considerations and the pelvis in the adult patient. Spine 34:1828–1833
Gelb DE, Lenke LG, Bridwell KH et al (1995) An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine 20:1351–1358
Blondel B, Schwab FJ, Bess S et al (2013) Posterior global malalignment after osteotomy for sagittal plane deformity: it happens and here is why. Spine 38:E394–E401
Glassman SD, Bridwell K, Dimar JR et al (2005) The impact of positive sagittal balance in adult spinal deformity. Spine 30:2024–2029
Simmons ED, DiStefano RJ, Yheng Y et al (2006) Thirty-six years experience of cervical extension osteotomy in Ankylosing Spondylitis. Spine 31:3006–3012
Dubousset J (1994) Three-dimensional analysis of the scoliotic deformity. In: Weinstein SL (ed) Pediatric spine and practice. Raven Press, New York, p 1994
Simmons E (1992) Ankylosing spondylitis: surgical considerations. Spine, 3rd edn. WB Saunders, Philadelphia
Suk K, Kim K, Lee S et al (2003) Significance of chin-brow vertical angle in correction of kyphotic deformity of ankylosing spondylitis patients. Spine 28:2001–2005
Sengupta D, Khazim R, Grevitt M et al (2001) Flexion osteotomy of the cervical spine. Spine 26:1068–1072
Lafage R, Challier V, Liabaud B et al (2016) Natural head posture in the setting of sagittal spinal deformity: validation of chin-brow vertical angle, slope of line of sight, and McGregor’s slope with health—related quality of life. Neurosurgery 79(1):108–115
Moses MJ, Tishelman JC, Zhou PL et al (2019) McGregor’s slope and slope of line of sight: two surrogate markers for chin–brow vertical angle in the setting of cervical spine pathology. Spine J 19(9):1512–1517
Laennec J, Saillant G, Saidi K et al (1997) Surgery of the deformities in ankylosing spondylitis: Our experience of lumbar osteotomies in 31 patients. Eur Spine J 6:222–232
Lafage R, Challier V, Lisbaud B et al (2016) Natural head posture in the setting of sagittal spinal deformity: validation of chin–brow vertical angle, slope of line of sight, and McGregor’s Slope with health-related quality of life. Neurosurgery 79(1):108–115
Shoda N, Takeshita K, Sheichi A et al (2004) Measurement of occipitocervical angle. Spine 29:E204–E208
Akbar M, Terran J, Ames C et al (2013) Use of surgimap spine in sagittal plane analysis, osteotomy planning, and correction calculation. Neurosurg Clin N Am 24(2):163–172
Vila-Casademunt A, Pellisé F, Acaroglu E et al (2015) The reliability of sagittal pelvic parameters: the effect of lumbosacral instrumentation and measurement experience. Spine 40(4):E253–E258
Booth K, Bridwell K, Lenke L et al (1999) Complications and predictive factors for the successful treatment of flatback deformity (fixed sagittal imbalance). Spine 24:1712–1720
Lafage V, Schwab F, Skalli W et al (2008) Standing balance and sagittal plane spinal deformity: analysis of spinopelvic and gravity line parameters. Spine 33:1572–1578
Smith J, Shaffrey C, Lafage V et al (2012) Spontaneous improvement of cervical alignment after correction of global sagittal balance following pedicle subtraction osteotomy. J Neurosurg Spine 17:300–307
Sheer J, Tang J, Smith J et al (2013) Cervical spine alignment, sagittal deformity, and clinical implications: a review. J Neurosurg Spine 19:141–159
Legaye J, Duval-Beaupere G, Hecquet J, Marty C (1998) Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 7(2):99–103
Funding
No research funding was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Buckland reports personal fees from Nuvasive, personal fees from Stryker K2M, personal fees from Medtronic, personal fees from EOS Imaging, outside the submitted work. Dr. Errico reports personal fees from Stryker/K2M, personal fees from Altus, from null, outside the submitted work. Dr. Lafage reports other from Nemaris, outside the submitted work. Dr. Lafage reports personal fees from NuVasive Inc., other from International Spine Society Group, personal fees from Globus Medical, Inc., personal fees from The Permanente Medical Group, other from European Spine Journal, personal fees from DePuy Synthes Spine, outside the submitted work. Dr. Lonner reports grants and non-financial support from Grant from Depuy Synthes to Setting Scoliosis Straight Foundation in Support of the Harms Study Group's research, personal fees, non-financial support and other from Depuy Synthes, personal fees and other from Zimmer Biomet, personal fees and non-financial support from Apifix, other from Paradigm Spine, other from Spine Search, other from SRS Spine Deformity Journal, outside the submitted work. Dr. Protopsaltis reports personal fees from Globus, personal fees from Stryker K2M, personal fees from Medicrea, personal fees from Altus, personal fees from Innovasis, outside the submitted work. The other co-authors have no disclosures.
Ethical approval
This study was approved by the Institutional Review Board at Mount Sinai Beth Israel.
Informed consent to participate/publication
Informed consent for this study was not required as this was a retrospective radiographic review. Institutional Review Board approval was granted for this waiver of consent. Consent for publication for this study was not required as this was a retrospective radiographic review. Institutional Review Board approval was granted for this waiver of consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
George, S., Spiegel, M., Protopsaltis, T. et al. Mandibular slope: a reproducible and simple measure of horizontal gaze. Spine Deform 8, 893–899 (2020). https://doi.org/10.1007/s43390-020-00137-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-020-00137-x