Abstract
Background
The impact of cancer on death of elderly kidney transplant recipients has been extensively investigated, but with conflicting results. Unlike their younger counterparts, in elderly kidney transplant recipients cardiovascular and infectious disease may outweigh cancer in causing the patient’s death.
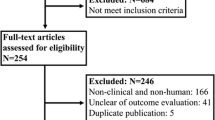
Methods
Using competing risk analysis on a large retrospective cohort of kidney transplant recipients, we estimated the cause-specific cumulative incidence and hazard of death in different age categories and calculated standardized mortality ratios (SMRs) to compare mortality rates with the general population.
Results
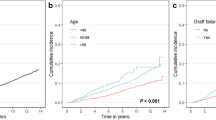
Six thousand seven hundred eighty-nine kidney transplant recipients were followed-up for a median of 9 years. Ten years after transplantation, in transplant recipients aged 20–39, 40–59, and 60+, the cumulative incidence of cancer-related death was 0.6 (95% confidence interval [CI]: 0.3–1.0), 2.9 (2.3–3.6) and 5.3% (3.5–7.5), whereas the SMR was 9.1 (5.5–15.0), 2.0 (1.6–2.5), and 0.8 (0.6–1.0), respectively. At variance with young recipients, the hazard and the cumulative incidence of cardiovascular-related death in elderly recipients was well above that of cancer-related death.
Conclusions
Relative to the general population, cancer-related death is increased in young but not in elderly kidney transplant recipients because of the more marked increased incidence of competing cause of death in the latter category.




Similar content being viewed by others
References
Vajdic CM, McDonald SP, McCredie MR et al (2006) Cancer incidence before and after kidney transplantation. JAMA 296:2823
Wong G, Chapman JR, Craig JC (2014) Death from cancer: a sobering truth for patients with kidney transplants. Kidney Int 85:1262
Farrugia D, Mahboob S, Cheshire J et al (2014) Malignancy-related mortality following kidney transplantation is common. Kidney Int 85:1395
Au EH, Chapman JR, Craig JC et al (2019) Overall and site-specific cancer mortality in patients on dialysis and after kidney transplant. J Am Soc Nephrol 30:471
Kiberd BA, Rose C, Gill JS (2009) Cancer mortality in kidney transplantation. Am J Transplant 9:1868
Vogelzang JL, van Stralen KJ, Noordzij M et al (2015) Mortality from infections and malignancies in patients treated with renal replacement therapy: data from the ERA-EDTA registry. Nephrol Dial Transplant 30:1028
Hecking M, Bieber BA, Ethier J et al (2014) Sex-specific differences in hemodialysis prevalence and practices and the male-to-female mortality rate: the dialysis outcomes and practice patterns study (DOPPS). PLOS Med 11:e1001750
Watschinger B, Budde K, Crespo M et al (2019) Pre-existing malignancies in renal transplant candidates-time to reconsider waiting times. Nephrol Dial Transplant 34:1292
Lim WH, Au E, Krishnan A, Wong G (2019) Assessment of kidney transplant suitability for patients with prior cancers: is it time for a rethink? Transpl Int 32:1223
Pham PT, Pham PA, Pham PC, Parikh S, Danovitch G (2010) Evaluation of adult kidney transplant candidates. Semin Dial 23:595
Marcen R (2009) Immunosuppressive drugs in kidney transplantation: impact on patient survival, and incidence of cardiovascular disease, malignancy, and infection. Drugs 69:2227
Noordzij M, Leffondré K, van Stralen KJ, Zoccali C, Dekker FW, Jager KJ (2013) When do we need competing risks methods for survival analysis in nephrology? Nephrol Dial Transplant 28:2670
Coviello V, Boggess M (2004) Cumulative incidence estimation in the presence of competing risks. Stata J 4:103
Gaynor JJ, Feuer EJ, Tan CC et al (1993) On the use of cause-specific failure probabilities: Examples from clinical oncology data. J Am Soc Stat Assoc 88:414
Fine JP, Gray RJ (1999) A proportional hazards model for the sub distribution of a competing risk. J Am Stat Assoc 94:496
Royston P, Parmar MKB (2002) Flexible parametric proportional-hazards and proportional-odds models for censored survival data, with application to prognostic modelling and estimation of treatment effects. Stat Med 21:2175
Kahwaji J, Bunnapradist S, Hsu JW, Idroos ML, Dudek R (2011) Cause of death with graft function among renal transplant recipients in an integrated healthcare system. Transplantation 91:225
Geissler EK (2015) Post-transplantation malignancies: here today, gone tomorrow? Nat Rev Clin Oncol 12:705
Acuna SA, Fernandes KA, Daly C et al (2016) Cancer mortality among recipients of solid-organ transplantation in Ontario, Canada. JAMA Oncol 2:463
Stoumpos S, Jardine AG, Mark PB (2015) Cardiovascular morbidity and mortality after kidney transplantation. Transplant Int 28:10
Liefeldt L, Budde K (2010) Risk factors for cardiovascular disease in renal transplant recipients and strategies to minimize risk. Transplant Int 23:1191–1204
Devine PA, Courtney AE, Maxwell AP (2019) Cardiovascular risk in renal transplant recipients. J Nephrol 32:389
Snyder JJ, Israni AK, Peng Y, Zhang L, Simon TA, Kasiske BL (2009) Rates of first infection following kidney transplant in the United States. Kidney Int 75:317–326
Au E, Wong G, Chapman JR (2018) Cancer in kidney transplant recipients. Nat Rev Nephrol 14:508
Rosso T, Bertuccio P, la Vecchia C, Negri E, Malvezzi M (2015) Cancer mortality trend analysis in Italy, 1980–2010, and predictions for 2015. Tumori 101:664
EBPG (European Expert Group on Renal Transplantation), European Renal Association (ERA-EDTA), European Society for Organ Transplantation (ESOT) (2000) European best practice guidelines for renal transplantation (part 1). Nephrol Dial Transpl 15:1
George J, Rapsomaniki E, Pujades-Rodriguez M et al (2015) How does cardiovascular disease first present in women and men? Incidence of 12 cardiovascular diseases in a contemporary cohort of 1 937 360 people. Circulation 132:1320
McClelland EE, Smith JM (2011) Gender specific differences in the immune response to infection. Arch Immunol Ther Exp 59:203
Adey DB (2013) Women and kidney transplantation. Adv Chronic Kidney Dis 20:427
Ramesh S, Mann MC, Holroyd-Leduc JM et al (2015) The effect of hormone therapy on all-cause and cardiovascular mortality in women with chronic kidney disease: protocol for a+ systematic review and meta-analysis. Syst Rev 4(44):2
Ahmed SB, Ramesh S (2016) Sex hormones in women with kidney disease. Nephrol Dial Transplant 31:1787
Attini R, Cabiddu G, Montersino B et al (2020) Contraception in chronic kidney disease: a best practice position statement by the Kidney and Pregnancy Group of the Italian Society of Nephrology. J Nephrol. https://doi.org/10.1007/s40620-020-00717-0
Noone AM, Pfeiffer RM, Dorgan JF et al (2019) Cancer-attributable mortality among solid organ transplant recipients in the United States: 1987 through 2014. Cancer 125:2647
Acknowledgements
We gratefully acknowledge Dr. Emanuele Crocetti and Dr. Stefano Ferretti from the AIRTUM, for having provided mortality rates of cancer in the general Italian population, and Dr. Matteo Malvezzi from the Mario Negri Institute of Pharmacological Research of Milano, for having provided mortality rates of squamous cell carcinoma of the skin in the general Italian population.
Funding
None.
Author information
Authors and Affiliations
Contributions
GT, UM, GZ and GG participated in research design, the writing of the paper, in the performance of the research and in data analysis. GT and UM contributed equally. RENM, LN, LB, FN, SS, EG, MC, PM, AP, IC, EM and MR participated in research design, in the performance of the research and revising the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest. No conflict of interest exists in the submission of this manuscript, and the manuscript is approved by all authors for publication. I would like to declare on behalf of my co-authors that the work described was original research, that has not been published previously, and is not under consideration for publication elsewhere, in whole or in part. And all the authors listed have approved the manuscript that is enclosed.
Ethical statement
All subjects were treated with standard care without intervention from this study. All data were obtained via electronic medical records and a database review and were de-identified (the patient’s name was replaced with an identification code, and the patient’s private information was deleted before the analysis) to protect patient privacy.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
40620_2020_847_MOESM1_ESM.pptx
Supplementary file1Figure S1. Sub-hazard ratios (SHRs) of death from each specific cause as predicted by the fitted multiple regression model of Fine and Gray for competing risk. Calendar year was fitted as a polynomial continuous variate. The reference value of SHR (i.e. SHR=1) was represented by age 40-59 and calendar year 2000. Dots do not represent SHRs of groups of actual patients but rather predicted SHR values of hypothetical patients in the selected age category and calendar year: the plot is meant to have a visual appraisal of the SHR estimates from an otherwise complex multiple regression model. Both calendar year and age category were statistically significant (P<0.001). SHR, Sub-hazard ratio (i.e. the ratio between hazards which are calculated including patients who already died from other causes to reflect the hazards the actually the observed cumulative incidences of CVD-related death in the presence of competing causes of death). Figure S2. Sub-hazard ratios (SHRs) of death from each specific cause as predicted by the fitted multiple regression model of Fine and Gray for competing risk. Calendar year was fitted as a polynomial continuous variate. The reference value of SHR (i.e. SHR=1) was represented by age 40-59 and calendar year 2000. Dots do not represent SHRs of groups of actual patients but rather predicted SHR values of hypothetical patients in the selected age category and calendar year: the plot is meant to have a visual appraisal of the SHR estimates from an otherwise complex multiple regression model. Both calendar year and age category were statistically significant (P<0.001); in addition, the interaction term between age category and polynomial calendar year was significant (P<0.001) meaning that the SHR did not consistently increase with age categories in all historical periods. SHR, Sub-hazard ratio (i.e. the ratio between hazards which are calculated including patients who already died from other causes to reflect the hazards the actually the observed cumulative incidences of cancer-related death in the presence of competing causes of death) (PPTX 206 kb)
Rights and permissions
About this article
Cite this article
Tessari, G., Maggiore, U., Zaza, G. et al. Mortality from cancer is not increased in elderly kidney transplant recipients compared to the general population: a competing risk analysis. J Nephrol 33, 1309–1319 (2020). https://doi.org/10.1007/s40620-020-00847-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-020-00847-5