Abstract
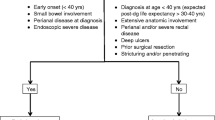
Despite increasing use of immunosuppressants and anti-tumor necrosis factor (TNF) agents, approximately half of Crohn’s disease (CD) patients still require surgery within 10 years after diagnosis. Surgery is not curative as postoperative relapse is very frequent in the absence of prophylactic treatment. Screening for known risk factors for postoperative recurrence allows patients to be stratified in order to consider appropriate therapy. A subsequent endoscopic evaluation and reassessment of treatment is currently the best strategy. Analyses of pooled data indicate that 5-aminosalicylic acid and thiopurines have only slight efficacy to prevent postoperative recurrence in CD. Nitroimidazole antibiotics are modestly effective, but long-term toxicity limits their use in clinical practice. Recently, anti-TNF agents have demonstrated the best efficacy profile to prevent endoscopic recurrence after surgery. As new treatment algorithms evolve towards increasing use of anti-TNF agents, this drives increased costs of management. However, this may be offset by the more widespread use of biosimilar versions of the anti-TNF agents. The increasing number of patients with previous exposure to numerous immunosuppressants and biologics at the time of surgery is a new challenge in postoperative management of CD, for which further data on new biologics are eagerly awaited.

Similar content being viewed by others
References
Rutgeerts P, Geboes K, Vantrappen G, et al. Predictability of the postoperative course of Crohn’s disease. Gastroenterology. 1990;99:956–63.
Gionchetti P, Dignass A, Danese S, et al. 3rd European evidence-based consensus on the diagnosis and management of Crohn’s disease 2016: part 2: surgical management and special situations. J. Crohns Colitis. 2017;11:135–49.
Bouguen G, Peyrin-Biroulet L. Surgery for adult Crohn’s disease: what is the actual risk? Gut. 2011;60:1178–81.
Peyrin-Biroulet L, Loftus EV Jr, Colombel J-F, et al. The natural history of adult Crohn’s disease in population-based cohorts. Am J Gastroenterol. 2010;105:289–97.
Peyrin-Biroulet L, Harmsen WS, Tremaine WJ, et al. Surgery in a population-based cohort of Crohn’s disease from Olmsted County, Minnesota (1970–2004). Am J Gastroenterol. 2012;107:1693–701.
Ma C, Moran GW, Benchimol EI, et al. Surgical rates for Crohn’s disease are decreasing: a population-based time trend analysis and validation study. Am J Gastroenterol. 2017;112:1840–8.
Peyrin-Biroulet L, Oussalah A, Williet N, et al. Impact of azathioprine and tumour necrosis factor antagonists on the need for surgery in newly diagnosed Crohn’s disease. Gut. 2011;60:930–6.
Khanna R, Bressler B, Levesque BG, et al. Early combined immunosuppression for the management of Crohn’s disease (REACT): a cluster randomised controlled trial. Lancet. 2015;386:1825–34.
Rutgeerts P, Geboes K, Vantrappen G, et al. Natural history of recurrent Crohn’s disease at the ileocolonic anastomosis after curative surgery. Gut. 1984;25:665–72.
Buisson A, Chevaux J-B, Allen PB, et al. Review article: the natural history of postoperative Crohn’s disease recurrence. Aliment Pharmacol Ther. 2012;35:625–33.
Solberg IC, Vatn MH, Høie O, et al. Clinical course in Crohn’s disease: results of a Norwegian population-based ten-year follow-up study. Clin Gastroenterol Hepatol. 2007;5:1430–8.
Binder V, Hendriksen C, Kreiner S. Prognosis in Crohn’s disease-based on results from a regional patient group from the county of Copenhagen. Gut. 1985;26:146–50.
Regueiro M, Kip KE, Schraut W, et al. Crohn’s disease activity index does not correlate with endoscopic recurrence one year after ileocolonic resection. Inflamm Bowel Dis. 2011;17:118–26.
De Cruz P, Kamm MA, Hamilton AL, et al. Crohn’s disease management after intestinal resection: a randomised trial. Lancet. 2015;385:1406–17.
Vuitton L, Marteau P, Sandborn WJ, et al. IOIBD technical review on endoscopic indices for Crohn’s disease clinical trials. Gut. 2016;65:1447–55.
Rivière P, Vermeire S, Irles-Depe M, et al. No change in determining Crohn’s disease recurrence or need for endoscopic or surgical intervention with modification of the Rutgeerts’ scoring system. Clin Gastroenterol Hepatol. 2019;17:1643–5.
Bayart P, Duveau N, Nachury M, et al. Ileal or anastomotic location of lesions does not impact rate of postoperative recurrence in Crohn’s disease patients classified i2 on the Rutgeerts score. Dig Dis Sci. 2016;61:2986–92.
Hirten RP, Ungaro RC, Castaneda D, et al. Anastomotic ulcers after ileocolic resection for Crohn’s disease are common and predict recurrence. Inflamm Bowel Dis. 2019. https://doi.org/10.1093/ibd/izz224.
Pouillon L, Amicone C, Remen T, Louis E, Maes S, Reenaers C, Germain A, Baumann C, Bossuyt P, Peyrin-Biroulet L. Risk of late post-operative recurrence of Crohn’s disease in endoscopic remission after ileocaecal resection: a 10-year multicenter experience. United Eur Gastroenterol J. 2019;7(8):330.
Koilakou S, Sailer J, Peloschek P, et al. Endoscopy and MR enteroclysis: equivalent tools in predicting clinical recurrence in patients with Crohn’s disease after ileocolic resection. Inflamm Bowel Dis. 2010;16:198–203.
Baillet P, Cadiot G, Goutte M, et al. Faecal calprotectin and magnetic resonance imaging in detecting Crohn’s disease endoscopic postoperative recurrence. World J Gastroenterol. 2018;24:641–50.
Pons Beltrán V, Nos P, Bastida G, et al. Evaluation of postsurgical recurrence in Crohn’s disease: a new indication for capsule endoscopy? Gastrointest Endosc. 2007;66:533–40.
Biancone L, Calabrese E, Petruzziello C, et al. Wireless capsule endoscopy and small intestine contrast ultrasonography in recurrence of Crohn’s disease. Inflamm Bowel Dis. 2007;13:1256–65.
Wright EK, Kamm MA, De Cruz P, et al. Measurement of fecal calprotectin improves monitoring and detection of recurrence of Crohn’s disease after surgery. Gastroenterology. 2015;148(938–947):e1.
Boschetti G, Laidet M, Moussata D, et al. Levels of fecal calprotectin are associated with the severity of postoperative endoscopic recurrence in asymptomatic patients with Crohn’s disease. Am J Gastroenterol. 2015;110:865–72.
Buisson A, Chevaux J-B, Bommelaer G, et al. Diagnosis, prevention and treatment of postoperative Crohn’s disease recurrence. Dig Liver Dis. 2012;44:453–60.
Timmer A, Sutherland LR, Martin F. Oral contraceptive use and smoking are risk factors for relapse in Crohn’s disease. The Canadian Mesalamine for Remission of Crohn’s Disease Study Group. Gastroenterology. 1998;114:1143–50.
Simillis C, Yamamoto T, Reese GE, et al. A meta-analysis comparing incidence of recurrence and indication for reoperation after surgery for perforating versus nonperforating Crohn’s disease. Am J Gastroenterol. 2008;103:196–205.
Ng SC, Lied GA, Arebi N, et al. Clinical and surgical recurrence of Crohn’s disease after ileocolonic resection in a specialist unit. Eur J Gastroenterol Hepatol. 2009;21:551–7.
McLeod RS, Wolff BG, Ross S, et al. Recurrence of Crohn’s disease after ileocolic resection is not affected by anastomotic type: results of a multicenter, randomized, controlled trial. Dis Colon Rectum. 2009;52:919–27.
Auzolle C, Nancey S, Tran-Minh M-L, et al. Male gender, active smoking and previous intestinal resection are risk factors for post-operative endoscopic recurrence in Crohn’s disease: results from a prospective cohort study. Aliment Pharmacol Ther. 2018;48:924–32.
Yamamoto T. Factors affecting recurrence after surgery for Crohn’s disease. World J Gastroenterol. 2005;11:3971–9.
Cañete F, Mañosa M, Casanova MJ, et al. Adalimumab or infliximab for the prevention of early postoperative recurrence of crohn disease: results from the ENEIDA registry. Inflamm Bowel Dis. 2019;25:1862–70.
Simillis C, Jacovides M, Reese GE, et al. Meta-analysis of the role of granulomas in the recurrence of Crohn disease. Dis Colon Rectum. 2010;53:177–85.
Ferrante M, de Hertogh G, Hlavaty T, et al. The value of myenteric plexitis to predict early postoperative Crohn’s disease recurrence. Gastroenterology. 2006;130:1595–606.
Sokol H, Polin V, Lavergne-Slove A, et al. Plexitis as a predictive factor of early postoperative clinical recurrence in Crohn’s disease. Gut. 2009;58:1218–25.
Bressenot A, Chevaux J-B, Williet N, et al. Submucosal plexitis as a predictor of postoperative surgical recurrence in Crohn’s disease. Inflamm Bowel Dis. 2013;19:1654–61.
Decousus S, Boucher A-L, Joubert J, et al. Myenteric plexitis is a risk factor for endoscopic and clinical postoperative recurrence after ileocolonic resection in Crohn’s disease. Dig Liver Dis. 2016;48:753–8.
Lemmens B, de Buck van Overstraeten A, Arijs I, et al. Submucosal plexitis as a predictive factor for postoperative endoscopic recurrence in patients with Crohn’s disease undergoing a resection with ileocolonic anastomosis: results from a prospective single-centre study. J. Crohns Colitis. 2017;11:212–20.
Ng SC, Lied GA, Kamm MA, et al. Predictive value and clinical significance of myenteric plexitis in Crohn’s disease. Inflamm Bowel Dis. 2009;15:1499–507.
Hammoudi N, Cazals-Hatem D, Auzolle C, et al. Association between microscopic lesions at ileal resection margin and recurrence after surgery in patients with Crohn’s disease. Clin Gastroenterol Hepatol. 2020;18:141–9.
Regueiro M, Feagan BG, Zou B, et al. Infliximab reduces endoscopic, but not clinical, recurrence of Crohn’s disease after ileocolonic resection. Gastroenterology. 2016;150:1568–78.
Collins M, Sarter H, Gower-Rousseau C, et al. Previous exposure to multiple anti-TNF is associated with decreased efficiency in preventing postoperative Crohn’s disease recurrence. J Crohns Colitis. 2017;11:281–8.
Brignola C, Cottone M, Pera A, et al. Mesalamine in the prevention of endoscopic recurrence after intestinal resection for Crohn’s disease. Italian Cooperative Study Group. Gastroenterology. 1995;108:345–9.
McLeod RS, Wolff BG, Steinhart AH, et al. Prophylactic mesalamine treatment decreases postoperative recurrence of Crohn’s disease. Gastroenterology. 1995;109:404–13.
Florent C, Cortot A, Quandale P, et al. Placebo-controlled clinical trial of mesalazine in the prevention of early endoscopic recurrences after resection for Crohn’s disease. Groupe d’Etudes Thérapeutiques des Affections Inflammatoires Digestives (GETAID). Eur. J. Gastroenterol. Hepatol. 1996;8:229–33.
Lochs H, Mayer M, Fleig WE, et al. Prophylaxis of postoperative relapse in Crohn’s disease with mesalamine: European Cooperative Crohn’s disease study VI. Gastroenterology. 2000;118:264–73.
Hanauer SB, Korelitz BI, Rutgeerts P, et al. Postoperative maintenance of Crohn’s disease remission with 6-mercaptopurine, mesalamine, or placebo: a 2-year trial. Gastroenterology. 2004;127:723–9.
Caprilli R, Andreoli A, Capurso L, et al. Oral mesalazine (5-aminosalicylic acid; Asacol) for the prevention of post-operative recurrence of Crohn’s disease Gruppo Italiano per lo Studio del Colon e del Retto (GISC). Aliment Pharmacol Ther. 1994;8:35–43.
Caprilli R, Cottone M, Tonelli F, et al. Two mesalazine regimens in the prevention of the post-operative recurrence of Crohn’s disease: a pragmatic, double-blind, randomized controlled trial. Aliment Pharmacol Ther. 2003;17:517–23.
Savarino E, Bodini G, Dulbecco P, et al. Adalimumab is more effective than azathioprine and mesalamine at preventing postoperative recurrence of Crohn’s disease: a randomized controlled trial. Am J Gastroenterol. 2013;108:1731–42.
Gjuladin-Hellon T, Gordon M, Iheozor-Ejiofor Z, et al. Oral 5-aminosalicylic acid for maintenance of surgically-induced remission in Crohn’s disease. Cochrane Database Syst. Rev. 2019;6:CD008414.
Doherty G, Bennett G, Patil S, et al. Interventions for prevention of post-operative recurrence of Crohn’s disease. Cochrane Database Syst Rev Online. 2009;CD006873.
Singh S, Garg SK, Pardi DS, et al. Comparative efficacy of pharmacologic interventions in preventing relapse of Crohn’s disease after surgery: a systematic review and network meta-analysis. Gastroenterology. 2015;148:64–76.
Ewe K, Herfarth C, Malchow H, et al. Postoperative recurrence of Crohn’s disease in relation to radicality of operation and sulfasalazine prophylaxis: a multicenter trial. Digestion. 1989;42:224–32.
Ford AC, Khan KJ, Talley NJ, et al. 5-aminosalicylates prevent relapse of Crohn’s disease after surgically induced remission: systematic review and meta-analysis. Am J Gastroenterol. 2011;106:413–20.
Ewe K, Böttger T, Buhr HJ, et al. Low-dose budesonide treatment for prevention of postoperative recurrence of Crohn’s disease: a multicentre randomized placebo-controlled trial. German Budesonide Study Group. Eur J Gastroenterol Hepatol. 1999;11:277–82.
Hellers G, Cortot A, Jewell D, et al. Oral budesonide for prevention of postsurgical recurrence in Crohn’s disease. The IOIBD Budesonide Study Group. Gastroenterology. 1999;116:294–300.
Rutgeerts P, Hiele M, Geboes K, et al. Controlled trial of metronidazole treatment for prevention of Crohn’s recurrence after ileal resection. Gastroenterology. 1995;108:1617–21.
Rutgeerts P, Van Assche G, Vermeire S, et al. Ornidazole for prophylaxis of postoperative Crohn’s disease recurrence: a randomized, double-blind, placebo-controlled trial. Gastroenterology. 2005;128:856–61.
Glick LR, Sossenheimer PH, Ollech JE, et al. Low-dose metronidazole is associated with a decreased rate of endoscopic recurrence of crohn’s disease after ileal resection: a retrospective Cohort study. J. Crohns Colitis. 2019;13:1158–62.
Herfarth HH, Katz JA, Hanauer SB, et al. Ciprofloxacin for the prevention of postoperative recurrence in patients with Crohn’s disease: a randomized, double-blind, placebo-controlled pilot study. Inflamm Bowel Dis. 2013;19:1073–9.
Ardizzone S, Maconi G, Russo A, et al. Randomised controlled trial of azathioprine and 5-aminosalicylic acid for treatment of steroid dependent ulcerative colitis. Gut. 2006;55:47–53.
Herfarth H, Tjaden C, Lukas M, et al. Adverse events in clinical trials with azathioprine and mesalamine for prevention of postoperative recurrence of Crohn’s disease. Gut. 2006;55:1525–6.
D’Haens GR, Vermeire S, Van Assche G, et al. Therapy of metronidazole with azathioprine to prevent postoperative recurrence of Crohn’s disease: a controlled randomized trial. Gastroenterology. 2008;135:1123–9.
Nos P, Hinojosa J, Aguilera V, et al. Azathioprine and 5-ASA in the prevention of postoperative recurrence of Crohn’s disease. Gastroenterol Hepatol. 2000;23:374–8.
Mowat C, Arnott I, Cahill A, et al. Mercaptopurine versus placebo to prevent recurrence of Crohn’s disease after surgical resection (TOPPIC): a multicentre, double-blind, randomised controlled trial. Lancet Gastroenterol. Hepatol. 2016;1:273–82.
Peyrin-Biroulet L, Deltenre P, Ardizzone S, et al. Azathioprine and 6-mercaptopurine for the prevention of postoperative recurrence in Crohn’s disease: a meta-analysis. Am J Gastroenterol. 2009;104:2089–96.
De Cruz P, Kamm MA, Hamilton AL, et al. Efficacy of thiopurines and adalimumab in preventing Crohn’s disease recurrence in high-risk patients—a POCER study analysis. Aliment Pharmacol Ther. 2015;42:867–79.
López-Sanromán A, Vera-Mendoza I, Domènech E, et al. Adalimumab vs azathioprine in the prevention of postoperative Crohn’s disease recurrence. A GETECCU Randomised Trial. J Crohns Colitis. 2017;11:1293–301.
Regueiro M, Schraut W, Baidoo L, et al. Infliximab prevents Crohn’s disease recurrence after ileal resection. Gastroenterology. 2009;136:441–50.
Regueiro M, El-Hachem S, Kip KE, et al. Postoperative infliximab is not associated with an increase in adverse events in Crohn’s disease. Dig Dis Sci. 2011;56:3610–5.
Regueiro M, Baidoo L, Kip KE, et al. Infliximab maintenance beyond one year prevents postoperative Crohn’s disease recurrence: long-term follow-up from the randomized controlled pilot study. Gastroenterology. 2013;144:173.
Yoshida K, Fukunaga K, Ikeuchi H, et al. Scheduled infliximab monotherapy to prevent recurrence of Crohn’s disease following ileocolic or ileal resection: a 3-year prospective randomized open trial. Inflamm Bowel Dis. 2012;18:1617–23.
Sorrentino D, Terrosu G, Avellini C, et al. Infliximab with low-dose methotrexate for prevention of postsurgical recurrence of ileocolonic Crohn disease. Arch Intern Med. 2007;167:1804–7.
Sorrentino D, Paviotti A, Terrosu G, et al. Low-dose maintenance therapy with infliximab prevents postsurgical recurrence of Crohn’s disease. Clin Gastroenterol Hepatol. 2010;8:591–9.
Aguas M, Bastida G, Cerrillo E, et al. Adalimumab in prevention of postoperative recurrence of Crohn’s disease in high-risk patients. WJG. 2012;18:4391–8.
Papamichael K, Archavlis E, Lariou C, et al. Adalimumab for the prevention and/or treatment of post-operative recurrence of Crohn’s disease: a prospective, two-year, single center, pilot study. J Crohns Colitis. 2012;6:924–31.
Yamada A, Komaki Y, Patel N, et al. The use of vedolizumab in preventing postoperative recurrence of Crohn’s disease. Inflamm Bowel Dis. 2018;24:502–9.
Sokol H, Brot L, Stefanescu C, et al. Prominence of ileal mucosa-associated microbiota to predict postoperative endoscopic recurrence in Crohn’s disease. Gut. 2019. https://doi.org/10.1136/gutjnl-2019-318719.
Van Gossum A, Dewit O, Louis E, et al. Multicenter randomized-controlled clinical trial of probiotics (Lactobacillus johnsonii, LA1) on early endoscopic recurrence of Crohn’s disease after lleo-caecal resection. Inflamm Bowel Dis. 2007;13:135–42.
Marteau P, Lémann M, Seksik P, et al. Ineffectiveness of Lactobacillus johnsonii LA1 for prophylaxis of postoperative recurrence in Crohn’s disease: a randomised, double blind, placebo controlled GETAID trial. Gut. 2006;55:842–7.
Prantera C, Scribano ML, Falasco G, et al. Ineffectiveness of probiotics in preventing recurrence after curative resection for Crohn’s disease: a randomised controlled trial with Lactobacillus GG. Gut. 2002;51:405–9.
Chermesh I, Tamir A, Reshef R, et al. Failure of Synbiotic 2000 to prevent postoperative recurrence of Crohn’s disease. Dig Dis Sci. 2007;52:385–9.
Madsen K, Backer JL, Leddin D, Dieleman LA, Bitton A, Feagan B, et al. A randomized controlled trial of VSL#3 for the prevention of endoscopic recurrence following surgery for Crohn’s disease. Gastroenterology. 2008;134(4 Suppl 1):A361.
Doherty GA, Bennett GC, Cheifetz AS, et al. Meta-analysis: targeting the intestinal microbiota in prophylaxis for post-operative Crohn’s disease. Aliment Pharmacol Ther. 2010;31:802–9.
Bommelaer G, Laharie D, Nancey S, et al. Oral curcumin no more effective than placebo in preventing recurrence of Crohn’s disease after surgery in a randomized controlled trial. Clin Gastroenterol Hepatol. 2019. https://doi.org/10.1016/j.cgh.2019.08.041.
de Bruyn Jessica, Bossuyt Peter, Ferrante Marc, et al. Postoperative endoscopic and clinical recurrence after ileocolonic resection in patients with Crohn’s disease cannot be prevented with high dose vitamin D. Gastroenterol. 2019;156(6 Suppl):1–33.
Nguyen GC, Loftus EV, Hirano I, et al. American gastroenterological association institute guideline on the management of Crohn’s disease after surgical resection. Gastroenterology. 2017;152:271–5.
Lichtenstein GR, Loftus EV, Isaacs KL, et al. ACG clinical guideline: management of Crohn’s disease in adults. Am J Gastroenterol. 2018;113:481–517.
Overview|Crohn’s disease: management|Guidance|NICE [Internet]. [cited 2019 Oct 9]. https://www.nice.org.uk/guidance/ng129. Accessed 9 Oct 2019.
Candia R, Naimark D, Sander B, et al. Cost-utility analysis: thiopurines plus endoscopy-guided biological step-up therapy is the optimal management of postoperative Crohn’s disease. Inflamm Bowel Dis. 2017;23:1930–40.
Gulacsi L, Pentek M, Rencz F, et al. Biosimilars for the management of inflammatory bowel diseases: economic considerations. Curr Med Chem. 2019;26:259–69.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
LV has received lecture fees from Abbvie, Ferring, Mayoli, MSD, Pfizer, Janssen, and Takeda; consulting fees from Abbvie, Ferring, Gilead, Janssen, and Takeda; research grants from MSD, Pfizer, and Takeda. LPB has received consulting fees from AbbVie, Amgen, Biogaran, Biogen, Boerhinger-Ingelheim, Bristol-Myers Squibb, Celgene, Celltrion, Ferring, Forward Pharma, Genentech, H.A.C. Pharma, Hospira, Index Pharmaceuticals, Janssen, Lycera, Merck, Lilly, Mitsubishi, Norgine, Pfizer, Pharmacosmos, Pilège, Samsung Bioepis, Sandoz, Takeda, Therakos, Tillots, UCB Pharma, and Vifor, and lecture fees from AbbVie, Ferring, H.A.C. Pharma, Janssen, Merck, Mitsubishi, Norgine, Takeda, Therakos, Tillots, and Vifor.
Funding statement
No funding was received for the preparation of this manuscript.
Rights and permissions
About this article
Cite this article
Vuitton, L., Peyrin-Biroulet, L. Pharmacological Prevention of Postoperative Recurrence in Crohn’s Disease. Drugs 80, 385–399 (2020). https://doi.org/10.1007/s40265-020-01266-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-020-01266-3