Abstract
Background/Objectives
Depression and hopelessness are frequently experienced in chronic kidney disease (CKD) and are generally associated with lessened physical activity. The aim of this study was to quantify the associations between sarcopenia as determined by SARC-F with both depression and hopelessness.
Design and Setting
This multicenter cohort study involving cross-sectional and longitudinal analyses was conducted in a university hospital and four general hospitals, each with a nephrology center, in Japan.
Participants
Participants consisted of 314 CKD patients (mean age 67.6), some of whom were receiving dialysis (228, 73%).
Measurements
The main exposures were depression, measured using the Center for Epidemiologic Studies Depression (CES-D) questionnaire, and hopelessness, measured using a recently developed 18-item health-related hope scale (HR-Hope). The outcomes were sarcopenia at baseline and one year after, measured using the SARC-F questionnaire. Logistic regression models were applied.
Results
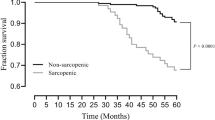
The cross-sectional and longitudinal analyses included 314 and 180 patients, respectively. Eighty-nine (28.3%) patients experienced sarcopenia at baseline, and 44 (24.4%) had sarcopenia at the one-year follow-up. More hopelessness (per 10-point lower, adjusted odds ratio [AOR]: 1.33, 95% confidence interval [95% CI] 1.12–1.58), depression (AOR: 1.87, 95% CI 1.003–3.49), age (per 10-year higher, AOR: 1.70, 95% CI 1.29–2.25), being female (AOR: 2.67, 95% CI 1.43–4.98), and undergoing hemodialysis (AOR, 2.92; 95% CI, 1.41–6.05) were associated with a higher likelihood of having baseline sarcopenia. More hopelessness (per 10-point lower, AOR: 1.69, 95% CI 1.14–2.51) and depression (AOR: 4.64, 95% CI: 1.33–16.2) were associated with a higher likelihood of having sarcopenia after one year.
Conclusions
Among patients with different stages of CKD, both hopelessness and depression predicted sarcopenia. Provision of antidepressant therapies or goal-oriented educational programs to alleviate depression or hopelessness can be useful options to prevent sarcopenia.


Similar content being viewed by others
References
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyere O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 2019;48(1):16–31.
Lamarca F, Carrero JJ, Rodrigues JC, Bigogno FG, Fetter RL, Avesani CM. Prevalence of sarcopenia in elderly maintenance hemodialysis patients: the impact of different diagnostic criteria. J Nutr Health Aging 2014;18(7):710–7.
Pereira RA, Cordeiro AC, Avesani CM, Carrero JJ, Lindholm B, Amparo FC, et al. Sarcopenia in chronic kidney disease on conservative therapy: prevalence and association with mortality. Nephrol Dial Transplant 2015;30(10):1718–25.
Giglio J, Kamimura MA, Lamarca F, Rodrigues J, Santin F, Avesani CM. Association of sarcopenia with nutritional parameters, quality of life, hospitalization, and mortality rates of elderly patients on hemodialysis. J Ren Nutr 2018;28(3):197–207.
Chang KV, Hsu TH, Wu WT, Huang KC, Han DS. Is sarcopenia associated with depression? A systematic review and meta-analysis of observational studies. Age Ageing 2017;46(5):738–46.
Kim JK, Choi SR, Choi MJ, Kim SG, Lee YK, Noh JW, et al. Prevalence of and factors associated with sarcopenia in elderly patients with end-stage renal disease. Clin Nutr 2014;33(1):64–8.
Kurita N, Wakita T, Ishibashi Y, Fujimoto S, Yazawa M, Suzuki T, et al. Association between health-related hope and adherence to prescribed treatment in CKD patients: multicenter cross-sectional study. BMC Nephrol 2020;21(1):453. doi: https://doi.org/10.1186/s12882-020-02120-0
Billington E, Simpson J, Unwin J, Bray D, Giles D. Does hope predict adjustment to end-stage renal failure and consequent dialysis? Br J Health Psychol 2008;13(4):683–99.
Ziegelstein RC, Fauerbach JA, Stevens SS, Romanelli J, Richter DP, Bush DE. Patients with depression are less likely to follow recommendations to reduce cardiac risk during recovery from a myocardial infarction. Arch Intern Med 2000;160(12):1818–23.
Blumenthal JA, Williams RS, Wallace AG, Williams RB, Jr., Needles TL. Physiological and psychological variables predict compliance to prescribed exercise therapy in patients recovering from myocardial infarction. Psychosom Med 1982;44(6):519–27.
Valtonen M, Laaksonen DE, Laukkanen J, Tolmunen T, Rauramaa R, Viinamäki H, et al. Leisure-time physical activity, cardiorespiratory fitness and feelings of hopelessness in men. BMC Public Health 2009;9(1):204.
Mitchell AM, Pössel P, Sjögren E, Kristenson M. Hopelessness the “active ingredient”? Associations of hopelessness and depressive symptoms with interleukin-6. Int J Psychiatr Med 2013;46(1):109–17.
Shima S, Shikano T, Kitamura T, Asai M. New self-rating scale for depression. Clin Psychiatry 1985;27(6):717–23 (in Japanese).
Fukuhara S, Kurita N, Wakita T, Green J, Shibagaki Y. A scale for measuring health-related hope: its development and psychometric testing. Ann Clin Epidemiol 2019;1(3):102–19. doi: https://doi.org/10.37737/ace.1.3_102
Radloff LS. The CES-D scale. Appl Psychol Meas 1977;1(3):385–401.
Snyder CR, Harris C, Anderson JR, Holleran SA, Irving LM, Sigmon ST, et al. The will and the ways: development and validation of an individual-differences measure of hope. J Pers Soc Psychol 1991;60(4):570–85.
Merchant RA, Chen MZ, Wong BLL, Ng SE, Shirooka H, Lim JY, et al. Relationship between fear of falling, fear-related activity restriction, frailty, and sarcopenia. J Am Geriatr Soc 2020:68(11):2602–8.
Malmstrom TK, Morley JE. SARC-F: a simple questionnaire to rapidly diagnose sarcopenia. J Am Med Dir Assoc 2013;14(8):531–2.
Chen LK, Woo J, Assantachai P, Auyeung TW, Chou MY, Iijima K, et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J Am Med Dir Assoc 2020; 21(3): 300–7.e302.
Ida S, Kaneko R, Murata K. SARC-F for screening of sarcopenia among older adults: A meta-analysis of screening test accuracy. J Am Med Dir Assoc 2018;19(8):685–9.
Kurita N, Wakita T, Kamitani T, Wada O, Mizuno K. SARC-F validation and SARC-F+EBM derivation in musculoskeletal disease: the SPSS-OK study. J Nutr Health Aging 2019;23(8):732–8.
van der Heijden GJMG, Donders AR, Stijnen T, Moons KG. Imputation of missing values is superior to complete case analysis and the missing-indicator method in multivariable diagnostic research: A clinical example. J Clin Epidemiol 2006;59(10):1102–9.
van Buuren S, Boshuizen HC, Knook DL. Multiple imputation of missing blood pressure covariates in survival analysis. Stat Med 1999;18(6):681–94.
Rubin DB. Multiple imputation for non response in surveys. New York: Wiley; 1987.
Everson SA, Kaplan GA, Goldberg DE, Salonen JT. Hypertension incidence is predicted by high levels of hopelessness in Finnish men. Hypertension 2000;35(2):561–7.
Everson SA, Goldberg DE, Kaplan GA, Cohen RD, Pukkala E, Tuomilehto J, et al. Hopelessness and risk of mortality and incidence of myocardial infarction and cancer. Psychosom Med 1996;58(2):113–21.
Honda H, Qureshi AR, Axelsson J, Heimburger O, Suliman ME, Barany P, et al. Obese sarcopenia in patients with end-stage renal disease is associated with inflammation and increased mortality. Am J Clin Nutr 2007;86(3):633–8.
Mehrotra R, Cukor D, Unruh M, Rue T, Heagerty P, Cohen SD, et al. Comparative efficacy of therapies for treatment of depression for patients undergoing maintenance hemodialysis: A randomized clinical trial. Ann Intern Med 2019;170(6):369–79.
Hedayati SS, Gregg LP, Carmody T, Jain N, Toups M, Rush AJ, et al. Effect of sertraline on depressive symptoms in patients with chronic kidney disease without dialysis dependence: the CAST randomized clinical trial. JAMA 2017;318(19):1876–90.
Veres A, Bain L, Tin D, Thorne C, Ginsburg LR. The neglected importance of hope in self-management programs—a call for action. Chronic Illn 2014;10(2):77–80.
Gardner T, Refshauge K, McAuley J, Hübscher M, Goodall S, Smith L. Combined education and patient-led goal setting intervention reduced chronic low back pain disability and intensity at 12 months: a randomised controlled trial. Br J Sports Med 2019;53(22):1424–31
Marini ACB, Perez DRS, Fleuri JA, Pimentel GD. SARC-F is better correlated with muscle function indicators than muscle mass in older hemodialysis patients. J Nutr Health Aging 2020;24(9):999–1002.
Hedayati SS, Bosworth HB, Kuchibhatla M, Kimmel PL, Szczech LA. The predictive value of self-report scales compared with physician diagnosis of depression in hemodialysis patients. Kidney Int 2006;69(9):1662–8.
Roemer M. Religious affiliation in contemporary Japan: untangling the enigma. Rev Relig Res 2009;50(3):298–320.
Acknowledgements
The authors greatly thank the following researchers, research assistants, and medical staff members for their assistance in collecting the questionnaire-based and clinical information used in this study: Ms. Asako Tamura, Ms. Yuka Masuda, and Ms. Takae Shimizu (St. Marriana University, Kawasaki-City, Kanagawa); Takayuki Nakamura, MD and Eiko Hashimoto, RN (JCHO Nihonmatsu Hospital, Nihonmatsu-City, Fukushima); Atsushi Kyan, MD and Masashi Saito, CE (Shirakawa Kosei General Hospital, Shirakawa-City, Fukushima); Ms. Lisa Shimokawa and Ms. Miyuki Sato (Fukushima Medical University Hospital, Fukushima-City, Fukushima).
Author information
Authors and Affiliations
Contributions
Authors’ contributions: Research idea and study design: NK, TW, YS, YI; data acquisition: NK, YI, SF, M Yazawa, TS, KK, M Yanagi, HK; data analysis and interpretation: NK, TW, YS, YI; statistical analysis: NK; supervision or mentorship: YS, YI. Each author contributed important intellectual content during article drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interests: The authors have no conflicts to disclose.
Ethical Standards: The study was conducted in accordance with the Declaration of Helsinki and the ethical guidelines for Ethical Guidelines for Medical and Health Research Involving Human Subjects in Japan.
Additional information
Financial Disclosure: This study was supported by JSPS KAKENHI (Grant Number: JP16H05216 and JP18K17970).
Sponsor’s role: The funder had no role in the study design, analysis, or interpretation of data; writing of the manuscript; or the decision to submit the manuscript for publication.
Impact Statement: We certify that this work is a novel clinical research contribution. We believe that its novelty and impact lie in the fact that existing literature has not investigated the predictive aspect of hopelessness for sarcopenia, differentiating it from depression amongst CKD and dialysis patients. The findings will allow clinicians and caregivers to create interventions that alleviate depression and hopelessness among CKD and dialysis patients, thus preventing sarcopenia.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Kurita, N., Wakita, T., Fujimoto, S. et al. Hopelessness and Depression Predict Sarcopenia in Advanced CKD and Dialysis: A Multicenter Cohort Study. J Nutr Health Aging 25, 593–599 (2021). https://doi.org/10.1007/s12603-020-1556-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-020-1556-4