Abstract
Background
Aortic regurgitation (AR) without primary leaflet disease (functional AR) is known to occur as a result of loss of coaptation due to sinotubular junction (STJ) dilatation. However, the characteristics of change in the aortic valve coaptation length (AVCL) in 3 cusps in patients with functional AR are, as yet, unclear. The aim of this study was to measure the AVCL in 3 cusps in patients with functional AR by three-dimensional transesophageal echocardiograph (3D TEE).
Methods and results
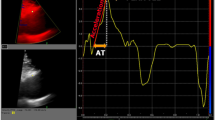
Thirteen patients with functional AR with or without aortic dilatation (trivial to mild AR [group A] and moderate to severe AR [group B]) and 7 controls without AR (group N) were examined. We measured the AVCL between the left coronary cusp (LCC) and right coronary cusp (RCC), the LCC and non coronary cusp (NCC), the RCC and NCC, and we also measured the cusp projection area, STJ arc length, leaflet tip–Valsalva wall distance and inter-commissural distance in each cusp by 3D TEE. The average AVCL was significantly shorter in group B than in groups N and A (P < 0.001). Particularly, in group B, there was a significant difference in AVCL in the 3 cusps (P = 0.043). Moreover, although there were no significant differences in the size of cusps in groups N and A, there was disproportion in the size of those cusps in group B with the largest in RCC.
Conclusion
Cusp enlargement was not uniform and was greatest in the RCC, and the loss of coaptation between the 3 cusps was also not uniform, with predominant reduction in the coaptation between the RCC and the other 2 cusps.



Similar content being viewed by others
References
Furukawa K, Ohteki H, Cao ZL, Doi K, Narita Y, Minato N, et al. Does dilatation of the sinotubular junction cause aortic regurgitation? Ann Thorac Surg. 1999;68:949–54.
Frazin L, Talano JV, Stephanides L, Loeb HS, Kopel L, Gunnar RM. Esophageal echocardiography. Circulation. 1976;54:102–8.
Pearlman AS, Gardin JM, Martin RP, Parisi AF, Popp RL, Quinones MA, et al. Guidelines for physician training in transesophageal echocardiography: recommendations of the American Society of Echocardiography Committee for Physician Training in Echocardiography. J Am Soc Echocardiogr. 1992;5:187–94.
Seward JB, Khandheria BK, Oh JK, Abel MD, Hughes RW Jr, Edwards WD, et al. Transesophageal echocardiography: technique, anatomic correlations, implementation, and clinical applications. Mayo Clin Proc. 1988;63:649–80.
Daniel WG, Erbel R, Kasper W, Visser CA, Engberding R, Sutherland GR, et al. Safety of transesophageal echocardiography. A multicenter survey of 10,419 examinations. Circulation. 1991;83:817–21.
Watanabe N, Ogasawara Y, Yamaura Y, Kawamoto T, Toyota E, Akasaka T, et al. Quantitation of mitral valve tenting in ischemic mitral regurgitation by transthoracic real-time three-dimensional echocardiography. J Am Coll Cardiol. 2005;45:763–9.
Watanabe N, Ogasawara Y, Yamaura Y, Wada N, Kawamoto T, Toyota E, et al. Mitral annulus flattens in ischemic mitral regurgitation: geometric differences between inferior and anterior myocardial infarction: a real-time 3-dimensional echocardiographic study. Circulation. 2005;112:I458–62.
Yamaura Y, Watanabe N, Ogasawara Y, Wada N, Kawamoto T, Toyota E, et al. Geometric change of mitral valve leaflets and annulus after reconstructive surgery for ischemic mitral regurgitation: real-time 3-dimensional echocardiographic study. J Thorac Cardiovasc Surg. 2005;130:1459–61.
Watanabe N, Ogasawara Y, Saito K, Yamaura Y, Tsukiji M, Okahashi N, et al. Quantitation of the degree of mitral valve prolapse by novel software system: new insights from transthoracic real-time three-dimensional echocardiography. J Echocardiogr. 2007;4:112–7.
Handke M, Jahnke C, Heinrichs G, Schlegel J, Vos C, Schmitt D, et al. New three-dimensional echocardiographic system using digital radiofrequency data—visualization and quantitative analysis of aortic valve dynamics with high resolution: methods, feasibility, and initial clinical experience. Circulation. 2003;107:2876–9.
Sato Y, Kamata J, Izumoto H, Nasu M, Kawazoe K. Morphological analysis of aortic root in eccentric aortic regurgitation using anyplane two-dimensional images produced by transesophageal three-dimensional echocardiography. J Heart Valve Dis. 2003;12:186–96.
Shim CY, Watanabe N, Tsukiji M, Yamaura Y, Ogasawara Y, Ha JW, et al. Three-dimensional geometry of aortic valve: a new trial of visualization with real-time three-dimensional echocardiography. J Echocardiogr. 2007;5:55–7.
Lang RM, Mor-Avi V, Sugeng L, Nieman PS, Sahn DJ. Three-dimensional echocardiography: the benefits of the additional dimension. J Am Coll Cardiol. 2006;48:2053–69.
Mercer JL, Benedicty M, Bahnson HT. The geometry and construction of the aortic leaflet. J Thorac Cardiovasc Surg. 1973;65:511–8.
Swanson M, Clark RE. Dimensions and geometric relationships of the human aortic valve as a function of pressure. Circ Res. 1974;35:871–82.
Perry GJ, Helmcke F, Nanda NC, Byard C, Soto B. Evaluation of aortic insufficiency by Doppler color flow mapping. J Am Coll Cardiol. 1987;9:952–9.
Dolan MS, Castello R, St Vrain JA, Aguirre F, Labovitz AJ. Quantitation of aortic regurgitation by Doppler echocardiography: a practical approach. Am Heart J. 1995;129:1014–20.
Vandervoort PM, Rivera JM, Mele D, Palacios IF, Dinsmore RE, Weyman AE, et al. Application of color Doppler flow mapping to calculate effective regurgitant orifice area. An in vitro study and initial clinical observations. Circulation. 1993;88:1150–6.
Bellhouse BJ, Bellhouse F, Abbott JA, Talbot L. Mechanism of valvular incompetence in aortic sinus dilatation. Cardiovasc Res. 1973;7:490–4.
Padial LR, Oliver A, Sagie A, Weyman AE, King ME, Levine RA. Two-dimensional echocardiographic assessment of the progression of aortic root size in 127 patients with chronic aortic regurgitation: role of the supraaortic ridge and relation to the progression of the lesion. Am Heart J. 1997;134:814–21.
Vasan RS, Larson MG, Levy D. Determinants of echocardiographic aortic root size. The Framingham Heart Study. Circulation. 1995;91:734–40.
Seder JD, Burke JF, Pauletto FJ. Prevalence of aortic regurgitation by color flow Doppler in relation to aortic root size. J Am Soc Echocardiogr. 1990;3:316–9.
Farasat SM, Morrell CH, Scuteri A, Ting CT, Yin FCP, Spurgeon HA, et al. Do hypertensive individuals have enlarged aortic root diameters? Insights from studying the various subtypes of hypertension. Am J Hypertens. 2008;21:558–63.
Edwards WD. Cardiac anatomy and examination of cardiac specimens. In: Emmanouilides G, Riemenschneider T, Allen H, Gutgesell H, editors. Moss & Adams’ heart disease in infants, children, and adolescents. 5th ed. Baltimore: Williams & Wilkins; 1995. pp. 70–105.
Minakata K, Schaff HV, Zehr KJ, Dearani JA, Daly RC, Orszulak TA, et al. Is repair of aortic valve regurgitation a safe alternative to valve replacement? J Thorac Cardiovasc Surg. 2004;127:645–53.
Acknowledgment
We would like to thank Mariko Mimura for the English language support.
Conflict of interest statement
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Imai, K., Watanabe, N., Saito, K. et al. Quantitative measurements of aortic valve coaptation by three-dimensional transesophageal echocardiography in patients with aortic regurgitation without primary leaflet disease. J Echocardiogr 8, 7–13 (2010). https://doi.org/10.1007/s12574-009-0028-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12574-009-0028-y