Abstract
Introduction
This study aimed to compare the challenge of puncture and catheterization and the effect of postoperative analgesia of ultrasound-guided continuous thoracic paravertebral block and the continuous epidural analgesia in patients receiving thoracoscopic surgery for lung cancer.
Methods
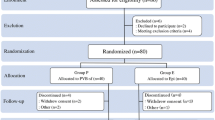
One-hundred and fifty patients received elective unilateral thoracoscopic surgery for lung cancer and were randomized into three groups; test group 1 (T group), test group 2 (P group), and the control group (E group). Both of the test groups received ultrasound-guided continuous thoracic paravertebral block (TPVB) while the control group received continuous epidural analgesia. After the operation, all the patients in the test groups received the same postoperative analgesia; loading dose 0.5 mg kg−1, background dose 0.25 mg kg−1 h−1, patient controlled analgesia (PCA) 0.25 mg kg−1, and a locking time of 60 min, while the patients in the control group received a loading dose of 5 ml, a background dose of 5 ml h−1, and a locking time of 20 min. The outcomes of this study were the success rate of the puncture and catheter placement, the blocked segments, numerical rating scale (NRS) scores at rest and during coughing, and the segments with reduced or lost cold and pinpricking sensation.
Results
The success rates of the puncture and catheterization in group T were the highest. Compared with group P, the failure rate of the puncture in group E was lower (p < 0.05), but the success rate of catheterization was higher (p < 0.05). The puncture time in group T was the shortest; there was no difference between group E and group T. The time of catheterization in group P was the longest, this was followed by group T, and was the fastest in group E. The stable time of the block level in group E was shorter than that in groups P and T, but was similar between groups P and T. The block level of all three groups in the 4 h postoperative period was similar (p > 0.05), while the 4 h postoperative levels of groups P and T were reduced significantly (p < 0.05).
Conclusion
The continuous analgesia technique of paravertebral space catheterization cannot replace the continuous epidural analgesia in thoracoscopic lung cancer surgery as the latter technique is still considered to be the gold standard.
Trial Registration
China Clinical Trial Registration Center identifier ChiCTR1900020973.






Similar content being viewed by others
References
Andreae MH, Andreae DA. Regional anaesthesia to prevent chronic pain after surgery: a Cochrane systematic review and meta-analysis. Br J Anaesth. 2013;111:711–20. https://doi.org/10.1093/bja/aet213.
Guay J, Nishimori M, Kopp SL. Epidural local anesthetics versus opioid-based analgesic regimens for postoperative gastrointestinal paralysis, vomiting, and pain after abdominal surgery: a Cochrane review. Anesth Analg. 2016;123:1591–602. https://doi.org/10.1213/ANE.0000000000001628.
Bendixen M, Jørgensen OD, Kronborg C, Andersen C, Licht PB. Postoperative pain and quality of life after lobectomy via video-assisted thoracoscopic surgery or anterolateral thoracotomy for early stage lung cancer: a randomised controlled trial. Lancet Oncol. 2016;17:836–44. https://doi.org/10.1016/S1470-2045(16)00173-X.
Scott WJ, Allen MS, Darling G, et al. Video-assisted thoracic surgery versus open lobectomy for lung cancer: a secondary analysis of data from the American College of Surgeons Oncology Group Z0030 randomized clinical trial. J Thorac Cardiovasc Surg. 2010;139:976–81. https://doi.org/10.1016/j.jtcvs.2009.11.059.
Wildgaard K, Ringsted TK, Hansen HJ, Petersen RH, Kehlet H. Persistent postsurgical pain after video-assisted thoracic surgery–an observational study. Acta Anaesthesiol Scand. 2016;60:650–8. https://doi.org/10.1111/aas.12681.
Steegers MA, Snik DM, Verhagen AF, van der Drift MA, Wilder-Smith OH. Only half of the chronic pain after thoracic surgery shows a neuropathic component. J Pain. 2008;9:955–61. https://doi.org/10.1016/j.jpain.2008.05.009.
Lenz N, Hirschburger M, Roehrig R, et al. Application of continuous wound-infusion catheters in lung transplantation: a retrospective data analysis. Thorac Cardiovasc Surg. 2017;65:403–9. https://doi.org/10.1055/s-0036-1580621.
Helms O, Mariano J, Hentz JG, et al. Intra-operative paravertebral block for postoperative analgesia in thoracotomy patients: a randomized, double-blind, placebo-controlled study. Eur J Cardiothorac Surg. 2011;40:902–6. https://doi.org/10.1016/j.ejcts.2011.01.067.
Rawal N. Epidural technique for postoperative pain: gold standard no more? Reg Anesth Pain Med. 2012;37:310–7. https://doi.org/10.1097/AAP.0b013e31825735c6.
Desai PM. Thoracic paravertebral block. Br J Anaesth. 1999;82:149–50. https://doi.org/10.1093/bja/82.1.149.
Richardson J, Lönnqvist PA. Thoracic paravertebral block. Br J Anaesth. 1998;81:230–8. https://doi.org/10.1093/bja/81.2.230.
Gilbert J, Hultman J. Thoracic paravertebral block: a method of pain control. Acta Anaesthesiol Scand. 1989;33:142–5. https://doi.org/10.1111/j.1399-6576.1989.tb02877.x.
Yeung JH, Gates S, Naidu BV, Wilson MJ, Gao Smith F. Paravertebral block versus thoracic epidural for patients undergoing thoracotomy. Cochrane Database Syst Rev. 2016;2:CD009121. https://doi.org/10.1002/14651858.CD009121.pub2.
Grider JS, Mullet TW, Saha SP, Harned ME, Sloan PA. A randomized, double-blind trial comparing continuous thoracic epidural bupivacaine with and without opioid in contrast to a continuous paravertebral infusion of bupivacaine for post-thoracotomy pain. J Cardiothorac Vasc Anesth. 2012;26:83–9. https://doi.org/10.1053/j.jvca.2011.09.003.
Gulbahar G, Kocer B, Muratli SN, et al. A comparison of epidural and paravertebral catheterisation techniques in post-thoracotomy pain management. Eur J Cardiothorac Surg. 2010;37:467–72. https://doi.org/10.1016/j.ejcts.2009.05.057.
Bimston DN, McGee JP, Liptay MJ, Fry WA. Continuous paravertebral extrapleural infusion for post-thoracotomy pain management. Surgery. 1999;126(4):650–7.
Casati A, Alessandrini P, Nuzzi M, et al. A prospective, randomized, blinded comparison between continuous thoracic paravertebral and epidural infusion of 0.2% ropivacaine after lung resection surgery. Eur J Anaesthesiol. 2006;23:999–1004. https://doi.org/10.1017/S0265021506001104.
Hutchins JL, Grandelis AJ, Kaizer AM, Jensen EH. Thoracic paravertebral block versus thoracic epidural analgesia for post-operative pain control in open pancreatic surgery: a randomized controlled trial. J Clin Anesth. 2018;48:41–5. https://doi.org/10.1016/j.jclinane.2018.04.013.
Bauer C, Pavlakovic I, Mercier C, et al. Adding sufentanil to ropivacaine in continuous thoracic paravertebral block fails to improve analgesia after video-assisted thoracic surgery: a randomised controlled trial. Eur J Anaesthesiol. 2018;35:766–73. https://doi.org/10.1097/EJA.0000000000000777.
Cowie B, McGlade D, Ivanusic J, Barrington MJ. Ultrasound-guided thoracic paravertebral blockade: a cadaveric study. Anesth Analg. 2010;110:1735–9. https://doi.org/10.1213/ANE.0b013e3181dd58b0.
Parra MC, Washburn K, Brown JR, et al. Fluoroscopic guidance increases the incidence of thoracic epidural catheter placement within the epidural space: a randomized trial. Reg Anesth Pain Med. 2017;42:17–24. https://doi.org/10.1097/AAP.0000000000000519.
Hurford WE, Bailin MT, Davison JK, Haspel K, Rosow C. Intravenous and inhalation anesthetics. Clinical anesthesia procedures of the Massachusetts General Hospital, 5th edn. Philadelphia: Lippincott-Raven; 1997. pp. 162–80.
Rosenberg PH, Veering BT, Urmey WF. Maximum recommended doses of local anesthetics: a multifactorial concept. Reg Anesth Pain Med. 2004;29:564–24. https://doi.org/10.1016/j.rapm.2004.08.003.
Bouman EAC, Sieben JM, Balthasar AJR, et al. Boundaries of the thoracic paravertebral space: potential risks and benefits of the thoracic paravertebral block from an anatomical perspective. Surg Radiol Anat. 2017;39:1117–1125. https://doi.org/10.1007/s00276-017-1857-4.
Fujii T, Shibata Y, Nishiwaki K. Observation of ultrasound-guided thoracic paravertebral block using thoracoscopy. Acta Anaesthesiol Taiwan. 2016;54:101–2. https://doi.org/10.1016/j.aat.2016.05.004.
Eason MJ, Wyatt R. Paravertebral thoracic block-a reappraisal. Anaesthesia. 1979;34:638–42. https://doi.org/10.1111/j.1365-2044.1979.tb06363.x.
Taketa Y, Irisawa Y, Fujitani T. Comparison of analgesic efficacy between two approaches of paravertebral block for thoracotomy: a randomised trial. Acta Anaesthesiol Scand. 2018;62:1274–9. https://doi.org/10.1111/aas.13216.
Krediet AC, Moayeri N, van Geffen GJ, et al. Different approaches to ultrasound-guided thoracic paravertebral block: an illustrated review. Anesthesiology. 2015;123:459–74. https://doi.org/10.1097/ALN.0000000000000747.
Yoshida T, Watanabe Y, Hashimoto T, Ohta A, Nakamoto T. Effects of catheter tip location on the spread of sensory block caused by a continuous thoracic paravertebral block: a prospective, randomized, controlled, double-blind study. Biomed Res Int. 2019;2019:1051629. .
Zani G, Bizzarri FT, Maitan S, et al. Thoracic paravertebral analgesia through a new multiple-hole catheter. J Cardiothorac Vasc Anesth. 2016;30:e13–e1414. https://doi.org/10.1053/j.jvca.2015.09.016.
Santonastaso DP, de Chiara A, Rispoli M, Musetti G, Agnoletti V. Real-time view of anesthetic solution spread during an ultrasound-guided thoracic paravertebral block. Tumori. 2018;104:NP50–NP52. https://doi.org/10.1177/0300891618763212.
Phoon P, Thong SY, Koh PT, Loh K. Thoracoscopic visualization of a misdirected paravertebral catheter. Can J Anaesth. 2015;62:830–1. https://doi.org/10.1007/s12630-015-0363-6.
Norum HM, Breivik H. A systematic review of comparative studies indicates that paravertebral block is neither superior nor safer than epidural analgesia for pain after thoracotomy. Scand J Pain. 2010;1:12–23. https://doi.org/10.1016/j.sjpain.2009.10.003.
Acknowledgements
Funding
This research was supported by Fujian Natural Science Foundation, China (No. 2018J01206). The journal’s Rapid Service Fee was funded by the authors.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Qiao-Wen Huang, Jia-Bin Li, Ye Huang, Wen-Qing Zhang and Zhi-Wei Lu have nothing to disclose.
Compliance with Ethics Guidelines
This study was approved by the Ethics Committee of the Zhangzhou Municipal Hospital of Fujian Province (2018-lx-002) and was registered in the China Clinical Trial Registration Center (ChiCTR1900020973, https://www.chictr.org.cn). We also received written informed consent from the patients and/or their families. The study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments.
Data Availability
All data generated or analyzed during this study are included in this published article/as supplementary information files.
Author information
Authors and Affiliations
Corresponding author
Additional information
Digital Features
To view digital features for this article go to https://doi.org/10.6084/m9.figshare.12631379.
Rights and permissions
About this article
Cite this article
Huang, QW., Li, JB., Huang, Y. et al. A Comparison of Analgesia After a Thoracoscopic Lung Cancer Operation with a Sustained Epidural Block and a Sustained Paravertebral Block: A Randomized Controlled Study. Adv Ther 37, 4000–4014 (2020). https://doi.org/10.1007/s12325-020-01446-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-020-01446-3