Abstract
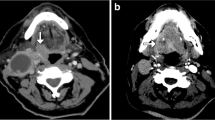
The World Health Organization (WHO) 2017 Classification of Head and Neck Tumors (“Blue Book”) will now include a new chapter on tumors and tumor-like lesions of the neck and lymph nodes, which was not included in the previous edition. Tumors and tumor-like lesions, including a variety of cysts and metastases, can arise in any component in the neck, including soft tissue, lymph nodes, and developmental remnants. The pathology and clinical features of metastatic carcinoma of unknown primary in the head and neck has changed dramatically in the last several years. Many of these tumors which were previously diagnosed as unknown primary are now identified as oropharyngeal and nasopharyngeal carcinomas related to human papillomavirus (HPV), less commonly to Epstein-Barr virus (EBV) and occasionally even to Merkel cell polyomavirus. Many unusual features can arise in these metastases, such as undifferentiated morphology, extensive cystic change with central degeneration, gland formation, and even ciliated cells. Rarely, carcinoma in the neck can arise in association with a heterotopic tissue, primarily thyroid or salivary gland tissue. Tumor-like lesions include branchial cleft cysts, thyroglossal duct cyst, dermoid and teratoid cyst, and ranula. Pathologists should be familiar with the diagnostic features and clinicopathologic corrections of these neck lesions in order to correctly diagnosis them and to provide for proper clinical management. This article will briefly describe the pathologic and clinical features of these entities as they are covered in the new 2017 Blue Book.



Similar content being viewed by others
References
Boscolo-Rizzo P, Schroeder L, Romeo S, Pawlita M. The prevalence of human papillomavirus in squamous cell carcinoma of unknown primary site metastatic to neck lymph nodes: a systematic review. Clin Exp Metastasis. 2015;32(8):835–45.
Ndiaye C, Mena M, Alemany L, Arbyn M, Castellsague X, Laporte L, et al. HPV DNA, E6/E7 mRNA, and p16INK4a detection in head and neck cancers: a systematic review and meta-analysis. Lancet Oncol. 2014;15(12):1319–31.
Bussu F, Sali M, Gallus R, Petrone G, Autorino R, Santangelo R, et al. HPV and EBV infections in neck metastases from occult primary squamous cell carcinoma: another virus-related neoplastic disease in the head and neck region. Ann Surg Oncol. 2015;22(Suppl 3):S979–84.
Tong CC, Luk MY, Chow SM, Ngan KC, Lau WH. Cervical nodal metastases from occult primary: undifferentiated carcinoma versus squamous cell carcinoma. Head Neck. 2002;24(4):361–9.
Chaturvedi AK, Engels EA, Pfeiffer RM, Hernandez BY, Xiao W, Kim E, et al. Human papillomavirus and rising oropharyngeal cancer incidence in the United States. J Clin Oncol. 2011;29(32):4294–301.
Bishop JA, Ma XJ, Wang H, Luo Y, Illei PB, Begum S, et al. Detection of transcriptionally active high-risk HPV in patients with head and neck squamous cell carcinoma as visualized by a novel E6/E7 mRNA in situ hybridization method. Am J Surg Pathol. 2012;36(12):1874–82.
Ang KK, Harris J, Wheeler R, Weber R, Rosenthal DI, Nguyen-Tan PF, et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med. 2010;363(1):24–35.
Ukpo OC, Flanagan JJ, Ma XJ, Luo Y, Thorstad WL, Lewis JS Jr. High-risk human papillomavirus E6/E7 mRNA detection by a novel in situ hybridization assay strongly correlates with p16 expression and patient outcomes in oropharyngeal squamous cell carcinoma. Am J Surg Pathol. 2011;35(9):1343–50.
McIlwain WR, Sood AJ, Nguyen SA, Day TA. Initial symptoms in patients with HPV-positive and HPV-negative oropharyngeal cancer. JAMA Otolaryngol Head Neck Surg. 2014;140(5):441–7.
Lewis JS Jr, Carpenter DH, Thorstad WL, Zhang Q, Haughey BH. Extracapsular extension is a poor predictor of disease recurrence in surgically treated oropharyngeal squamous cell carcinoma. Mod Pathol. 2011;24(11):1413–20.
Goldenberg D, Begum S, Westra WH, Khan Z, Sciubba J, Pai SI, et al. Cystic lymph node metastasis in patients with head and neck cancer: an HPV-associated phenomenon. Head Neck. 2008;30(7):898–903.
Gondim DD, Haynes W, Wang X, Chernock RD, El-Mofty SK, Lewis JS Jr. Histologic typing in oropharyngeal squamous cell carcinoma: a 4-year prospective practice study with p16 and high-risk HPV mRNA testing correlation. Am J Surg Pathol. 2016.
Chernock RD. Morphologic features of conventional squamous cell carcinoma of the oropharynx: ‘keratinizing’ and ‘nonkeratinizing’ histologic types as the basis for a consistent classification system. Head Neck Pathol. 2012;6(Suppl 1):S41–7.
Jalaly JB, Lewis JS Jr, Collins BT, Wu X, Ma XJ, Luo Y, et al. Correlation of p16 immunohistochemistry in FNA biopsies with corresponding tissue specimens in HPV-related squamous cell carcinomas of the oropharynx. Cancer cytopathology. 2015;123(12):723–31.
Holmes BJ, Maleki Z, Westra WH. The fidelity of p16 staining as a surrogate marker of human papillomavirus status in fine-needle aspirates and core biopsies of neck node metastases: implications for HPV testing protocols. Acta Cytol. 2015;59(1):97–103.
Xu B, Ghossein R, Lane J, Lin O, Katabi N. The utility of p16 immunostaining in fine needle aspiration in p16-positive head and neck squamous cell carcinoma. Hum Pathol. 2016;54:193–200.
Bishop JA, Westra WH. Ciliated HPV-related carcinoma: a well-differentiated form of head and neck carcinoma that can be mistaken for a benign cyst. Am J Surg Pathol. 2015;39(11):1591–5.
Radkay-Gonzalez L, Faquin W, McHugh JB, Lewis JS Jr, Tuluc M, Seethala RR. Ciliated adenosquamous carcinoma: expanding the phenotypic diversity of human papillomavirus-associated tumors. Head Neck Pathol. 2016;10(2):167–75.
Cianchetti M, Mancuso AA, Amdur RJ, Werning JW, Kirwan J, Morris CG, et al. Diagnostic evaluation of squamous cell carcinoma metastatic to cervical lymph nodes from an unknown head and neck primary site. Laryngoscope. 2009;119(12):2348–54.
McDowell LJ, Young RJ, Johnston ML, Tan TJ, Kleid S, Liu CS, et al. p16-positive lymph node metastases from cutaneous head and neck squamous cell carcinoma: no association with high-risk human papillomavirus or prognosis and implications for the workup of the unknown primary. Cancer. 2016;122(8):1201–8.
Yanagawa N, Wang A, Kohler D, Santos Gda C, Sykes J, Xu J, et al. Human papilloma virus genome is rare in North American non-small cell lung carcinoma patients. Lung cancer. 2013;79(3):215–20.
Kuwamoto S, Higaki H, Kanai K, Iwasaki T, Sano H, Nagata K, et al. Association of Merkel cell polyomavirus infection with morphologic differences in Merkel cell carcinoma. Hum Pathol. 2011;42(5):632–40.
Leech SN, Kolar AJ, Barrett PD, Sinclair SA, Leonard N. Merkel cell carcinoma can be distinguished from metastatic small cell carcinoma using antibodies to cytokeratin 20 and thyroid transcription factor 1. J Clin Pathol. 2001;54(9):727–9.
Pan Z, Chen YY, Wu X, Trisal V, Wilczynski SP, Weiss LM, et al. Merkel cell carcinoma of lymph node with unknown primary has a significantly lower association with Merkel cell polyomavirus than its cutaneous counterpart. Mod Pathol. 2014;27(9):1182–92.
Foote M, Veness M, Zarate D, Poulsen M. Merkel cell carcinoma: the prognostic implications of an occult primary in stage IIIB (nodal) disease. J Am Acad Dermatol. 2012;67(3):395–9.
Newberry TR, Kaufmann CR, Miller FR. Review of accessory parotid gland tumors: pathologic incidence and surgical management. Am J Otolaryngol. 2014;35(1):48–52.
Daniel E, McGuirt WF Sr. Neck masses secondary to heterotopic salivary gland tissue: a 25-year experience. Am J Otolaryngol. 2005;26(2):96–100.
Klubo-Gwiezdzinska J, Manes RP, Chia SH, Burman KD, Stathatos NA, Deeb ZE, et al. Clinical review: ectopic cervical thyroid carcinoma–review of the literature with illustrative case series. J Clin Endocrinol Metab. 2011;96(9):2684–91.
Barnes L. Surgical pathology of the head and neck. New York: CRC Press; 2008.
Doi O, Hutson JM, Myers NA, McKelvie PA. Branchial remnants: a review of 58 cases. J Pediatr Surg. 1988;23(9):789–92.
Golledge J, Ellis H. The aetiology of lateral cervical (branchial) cysts: past and present theories. J Laryngol Otol. 1994;108(8):653–9.
Sidhu S, Lioe TF, Clements B. Thyroid papillary carcinoma in lateral neck cyst: missed primary tumour or ectopic thyroid carcinoma within a branchial cyst? J Laryngol Otol. 2000;114(9):716–8.
Doshi J, Anari S. Branchial cyst side predilection: fact or fiction? Ann Otol Rhinol Laryngol. 2007;116(2):112–4.
Guldfred LA, Philipsen BB, Siim C. Branchial cleft anomalies: accuracy of pre-operative diagnosis, clinical presentation and management. J Laryngol Otol. 2012;126(6):598–604.
Bradley PT, Bradley PJ. Branchial cleft cyst carcinoma: fact or fiction? Curr Opinion Otolaryngol Head Neck Surg. 2013;21(2):118–23.
Cao D, Begum S, Ali SZ, Westra WH. Expression of p16 in benign and malignant cystic squamous lesions of the neck. Hum Pathol. 2010;41(4):535–9.
LaPlante JK, Pierson NS, Hedlund GL. Common pediatric head and neck congenital/developmental anomalies. Radiol Clin North Am. 2015;53(1):181–96.
Soni S, Poorey VK, Chouksey S. Thyroglossal duct cyst, variation in presentation, our experience. Indian J Otolaryngol Head Neck Surg. 2014;66(4):398–400.
Choi YM, Kim TY, Song DE, Hong SJ, Jang EK, Jeon MJ, et al. Papillary thyroid carcinoma arising from a thyroglossal duct cyst: a single institution experience. Endocr J. 2013;60(5):665–70.
Allard RH. The thyroglossal cyst. Head Neck Surg. 1982;5(2):134–46.
Gaddikeri S, Vattoth S, Gaddikeri RS, Stuart R, Harrison K, Young D, et al. Congenital cystic neck masses: embryology and imaging appearances, with clinicopathological correlation. Curr Probl Diagn Radiol. 2014;43(2):55–67.
Deane SA, Telander RL. Surgery for thyroglossal duct and branchial cleft anomalies. Am J Surg. 1978;136(3):348–53.
Hartl DM, Al Ghuzlan A, Chami L, Leboulleux S, Schlumberger M, Travagli JP. High rate of multifocality and occult lymph node metastases in papillary thyroid carcinoma arising in thyroglossal duct cysts. Ann Surg Oncol. 2009;16(9):2595–601.
Patel SG, Escrig M, Shaha AR, Singh B, Shah JP. Management of well-differentiated thyroid carcinoma presenting within a thyroglossal duct cyst. J Surg Oncol. 2002;79(3):134–9. discussion 40–1.
Ellis GL AP. Tumors of the salivary glands. Silver Spring, MD: ARP Press; 2008.
Wenig BM. Atlas of head and neck pathology. New York, NY 2008 2008.
Zhao YF, Jia Y, Chen XM, Zhang WF. Clinical review of 580 ranulas. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol. 2004;98(3):281–7.
Pryor SG, Lewis JE, Weaver AL, Orvidas LJ. Pediatric dermoid cysts of the head and neck. Otolaryngol–Head Neck Surg. 2005;132(6):938–42.
Paradis J, Koltai PJ. Pediatric teratoma and dermoid cysts. Otolaryngol Clin North Am. 2015;48(1):121–36.
Orozco-Covarrubias L, Lara-Carpio R, Saez-De-Ocariz M, Duran-McKinster C, Palacios-Lopez C, Ruiz-Maldonado R. Dermoid cysts: a report of 75 pediatric patients. Pediatr Dermatol. 2013;30(6):706–11.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Neither author has any conflicts of interest to disclose.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Special Issue: World Health Organization Classification Update
Rights and permissions
About this article
Cite this article
Katabi, N., Lewis, J.S. Update from the 4th Edition of the World Health Organization Classification of Head and Neck Tumours: What Is New in the 2017 WHO Blue Book for Tumors and Tumor-Like Lesions of the Neck and Lymph Nodes. Head and Neck Pathol 11, 48–54 (2017). https://doi.org/10.1007/s12105-017-0796-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12105-017-0796-z