Abstract
Background and purpose
Left ventricular diastolic dysfunction (LVDD) constitutes the prominent characteristic of cirrhotic cardiomyopathy, but its relevance on the clinical course of cirrhotic patients has not been clearly defined. The aim of the study was to evaluate the relationship of LVDD with the severity and etiology of liver disease and to investigate whether it affects the outcome of cirrhotic patients.
Methods
Cardiac function of 45 cirrhotics was studied by a tissue Doppler imaging echocardiography. Diagnosis of LVDD was made according to the latest guidelines of the American Society of Echocardiography. All patients were followed up for a period of 2 years. Death or liver transplantation was the endpoint of the study.
Results
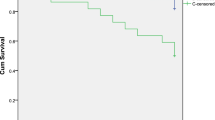
LVDD was found in 17 (38 %) of 45 patients. Its presence was not found to be associated with the etiology and stage of cirrhosis, but its severity was directly correlated with the Child-Pugh score. At the end of follow-up, 14 patients had died; 9 had LVDD (9/17, 53 %) and 5 had not (5/28, 18 %). Patients who died at the beginning of observation period had a higher Child-Pugh and MELD score, higher BNP, lower albumin and more prolonged QTc. On Kaplan-Meier analysis, patients with LVDD had statistically significantly worse prognosis compared to those without (p = 0.013, log rank: 5.495). Low albumin values (p = 0.003) and presence of LVDD (p = 0.017) were independent predictive factors of mortality.
Conclusions
LVDD is a common complication of cirrhosis. As its development seems to be related to a worse prognosis, patients with LVDD must be under a strict follow-up.


Similar content being viewed by others
Abbreviations
- LVDD:
-
Left ventricular diastolic dysfunction
- HRS:
-
Hepatorenal syndrome
- CC:
-
Cirrhotic cardiomyopathy
- SBP:
-
Spontaneous bacterial peritonitis
- BNP:
-
Brain natriuretic peptide
- ECG:
-
Electrocardiograph
- QTc:
-
Corrected QT interval
- PW:
-
Pulse wave
- TDI:
-
Tissue Doppler imaging
- HR:
-
Heart rate
- MAP:
-
Mean arterial pressure
- LVEDD:
-
Left ventricular end diastolic diameter
- LAvol in.:
-
Left atrium volume index
- LVEF %:
-
Left ventricular ejection fraction %
- CI:
-
Cardiac index
- SVRI:
-
Systemic vascular resistance index
- DT:
-
Deceleration time
- IVRT:
-
Isovolumetric relaxation time
- PASP:
-
Pulmonary artery systolic pressure
- MELD:
-
Model of end-stage liver disease
References
Schrier RW, Arroyo V, Bernardi M, Epstein M, Henriksen JH, Rode’s J. Peripheral artery vasodilatation hypothesis: a proposal for the initiation of renal sodium and water retention in cirrhosis. Hepatology 1988;5:1151–1157
Iwakiri Y, Groszmann RJ. The hyperdynamic circulation of chronic liver diseases: from the patient to the molecule. Hepatology 2006;43:S121–S131
Salermo F, Cazzaniga M, Gobbo G. Pharmacological treatment of hepatorenal syndrome: a note of optimism. J Hepatol 2007;47:729–731
Moller S, Henriksen JH. The systemic circulation in cirrhosis. In Gines P, Arroyo V, Rodes J, Schrier RW, editors. Ascites and Renal Dysfunction in Liver Disease. 2nd ed. Malden: Blackwell; 2005. 139–155
Krag A, Bendtsen F, Burroughs AK, Moller S. The cardiorenal link in advanced cirrhosis. Med Hypotheses 2012;79:53–55
Timoh T, Protano MA, Wagman G, Bloom M, Vittorio TJ. A perspective on cirrhotic cardiomyopathy. Transplant Proc 2011;43:1649–1653
Moller S, Hove JD, Dixen U, Bendtsen F. New insights into cirrhotic cardiomyopathy. Int J Cardiol 2013;167:1101–1108
Bernardi M, Maggioli C, Dibra V, Zaccherini G. QT interval prolongation in liver cirrhosis: innocent bystander or serious threat? Expert Rev Gastroenterol Hepatol 2012;6:57–66
Wiese S, Hove JD, Bendtsen F, Moller S. Cirrhotic cardiomyopathy: pathogenesis and clinical relevance. Nat Rev Gastroenterol Hepatol 2013;11:177–186
Pozzi M, Redaelli E, Ratti L, Poli G, Guidi C, Milanese M, et al. Time-course of diastolic dysfunction in different stages of chronic HCV related liver diseases. Minerva Gastroenterol Dietol 2005;51:179–186
Guilo P, Mansourati J, Maheu B, Etienne Y, Provost K, Simon O, et al. Long-term prognosis in patients with alcoholic cardiomyopathy and severe heart failure after total abstinence. Am J Cardiol 1997;79(9):1276–1278
Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr 2009;22:107–133
Klein AL, Burstow DJ, Talik AJ, Zachariak PK, Bailey KR, Seward JB. Effects of age on left ventricular dimensions and filling dynamics in 117 normal persons. Mayo Clin Proc 1994;69:212–224
Kazankov K, Holland-Fischer P, Andersen NH, Torp P, Sloth E, Aagaard NK, et al. Resting myocardial dysfunction in cirrhosis quantified by tissue Doppler imaging. Liver Int 2011;31:534–540
Sampaio F, Pimenta J, Bettencourt N, Fontes‐Carvalho R, Silva AP, Valente J, et al. Systolic and diastolic dysfunction in cirrhosis: a tissue-Doppler and speckle tracking echocardiography study. Liver int 2013;33:1158–1165
Lee RF, Glenn TK, Lee SS. Cardiac dysfunction in cirrhosis. Best Pract Res Clin Gastroenterol 2007;21:125–140
Mandell MS, Lindenfeld J, Tsou MY, Zimmerman M. Cardiac evaluation of liver transplant candidates. World J Gastroenterol 2008;14:3445–3451
Moller S, Bernardi M. Interactions of the heart and the liver. Eur Heart J 2013;34:2804–2811
Cazzaniga M, Salerno F, Pagnozzi G, Dionigi E, Visentin S, Cirello I, et al. Diastolic dysfunction is associated with poor survival in cirrhotic patients with transjugular intrahepatic portosystemic shunt. Gut 2007;56:869–875
Rabie RN, Cazzaniga M, Salerno F, Wong F. The use of E/A ratio as a predictor of outcome in cirrhotic patients treated with transjugular intrahepatic portosystemic shunt. Am J Gastroenterol 2009;104:2458–2466
Ripoll C, Catalina MV, Yotti R, Olmedilla L, Pérez-Peña J, Iacono O, et al. Cardiac dysfunction during liver transplantation: incidence and preoperative predictors. Transplantation 2008;85:1766–1772
Holt EW, Woo G, Trilesskaya M, Haeusslein EA, Shaw RE, Frederick RT. Diastolic dysfunction defined by E/A ratio < 1 on 2-D echo is an independent predictor of liver transplantation or death in patient with cirrhosis. J Hepatol 2011;54:S245–S246
Ruiz-del-Arbol L, Achecar L, Serradilla R, Rodríguez‐Gandía MÁ, Rivero M, Garrido E, et al. Diastolic dysfunction is a predictor of poor outcomes in patients with cirrhosis, portal hypertension and I normal creatinine. Hepatology 2013;58:1732–1741
Nazar A, Guevara M, Sitges M, Terra C, Solà E, Guigou C, et al. Left ventricular function assessed by echocardiography in cirrhosis: Relationship to systemic hemodynamics and renal dysfunction. J Hepatol 2013;58:51–57
Merli M, Calicchia A, Ruffa A, Pellicori P, Riggio O, Giusto M, et al. Cardiac dysfunction in cirrhosis is not associated with the severity of liver disease. Euro J Int Med 2013;24:172–176
Alexopoulou A, Papatheodoridis G, Pouriki S, Chrysohoou C, Raftopoulos L, Stefanadis C, et al. Diastolic myocardial dysfunction does not affect survival in patients with cirrhosis. Transpl Int 2012;25:1174–1181
Henriksen JH, Goetze JP, Fuglsang S, Christensen E, Bendtsen F, Moller S. Increased circulating pro-brain natriuretic peptide (proBNP) and brain natriuretic peptide (BNP) in patients with cirrhosis: relation to cardiovascular dysfunction and severity of disease. Gut 2003;52:1511–1157
Pimenta J, Paulo C, Gomes A, Silva S, Rocha-Goncalves F, Bettencourt P. B-type natriuretic peptide is related to cardiac function and prognosis in hospitalized patients with decompensated cirrhosis. Liver Int 2010;30:1059–1066
Bal JS, Thuluvath PJ. Prolongation of QTc inteval: relationship with etiology and severity of liver disease, mortality and liver transplantation. Liver int 2003;23:243–248
Trevisani F, Di Micoli A, Zambruni A, Biselli M, Santi V, Erroi V, et al. QT interval prolongation by acute gastrointestinal bleeding in patients with cirrhosis. Liver Int 2012;32:1510–1515
Acknowledgements
Guarantor of the study: Prof. S.D. Ladas. D.Karagiannakis planned and designed the study, recruited the pool of patients, analyzed the data and wrote the report. G. Anastasiadis was responsible for the cardiovascular assessment that was performed on patients. Assistant Prof. J. Vlachogiannakos participated in the study design and interpretation of the data, and he was responsible for the statistical analysis. Prof. I. Vafiadis-Zouboulis participated in the interpretation of the data.
Compliance with ethical requirements and Conflict of interest
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. Informed consent was obtained from all patients for being included in the study. Dimitrios Karagiannakis, Jiannis Vlachogiannakos, Georgios Anastasiadis, Irini Vafiadis-Zouboulis and Spiros D. Ladas declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Karagiannakis, D.S., Vlachogiannakos, J., Anastasiadis, G. et al. Diastolic cardiac dysfunction is a predictor of dismal prognosis in patients with liver cirrhosis. Hepatol Int 8, 588–594 (2014). https://doi.org/10.1007/s12072-014-9544-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-014-9544-6