Abstract
Introduction
We analyzed the impact of cause, severity, and duration of fever on functional outcome in patients with aneurysmal subarachnoid hemorrhage (aSAH).
Methods
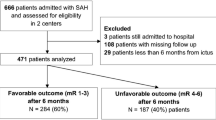
Fever characteristics were analyzed in 584 consecutive patients with aSAH. Fever was defined as core body temperature ≥38.3 °C on ≥2 consecutive days. Subfebrile measurements were those between 37 and 38.2 °C. Febrile and subfebrile loads were the number of hours with fever or subfebrile measurements, respectively. Univariate and multivariate logistic regression models were developed to define predictors of outcome using various categorizations of fever cause, severity, and duration.
Results
Febrile measurements were observed in 281/584 (48.1 %) patients, recurring over a mean duration of 2.1 ± 3.0 days. Early fever within 24 and 72 h was encountered in 69 (11.9 %) and 110 (18.9 %) of patients, respectively. An infectious source was discovered in 126 (44.8 %) febrile patients. On univariate analysis, days of fever, febrile load, and fever onset within 24 and 72 h were associated with poor outcome (all p < 0.001); but subfebrile load was not (p = 0.56). On multivariate model constructed with all variables associated with outcome on univariate analyses, days of fever remained independently associated with poor outcome (OR 1.14 of poor outcome per day of fever, 95 % CI 1.06–1.22; p = 0.0006) displacing all other fever measures from the final model.
Conclusions
Early onset of fever, number of hours with fever, and especially days of fever are associated with poor functional outcome. Conversely, subfebrile load does not influence clinical outcome. These data suggest prolonged fever should be avoided, but subfebrile temperatures may not justify intervention.
Similar content being viewed by others
References
Polderman KH. Induced hypothermia and fever control for prevention and treatment of neurological injuries. Lancet. 2008;371:1955–69.
Greer DM, Funk SE, Reaven NL, Ouzounelli M, Uman GC. Impact of fever on outcome in patients with stroke and neurologic injury: a comprehensive meta-analysis. Stroke. 2008;39:3029–35.
Rossi S, Zanier ER, Mauri I, Columbo A, Stocchetti N. Brain temperature, body core temperature, and intracranial pressure in acute cerebral damage. J Neurol Neurosurg Psychiatry. 2001;71:448–54.
Diringer MN, Reaven NL, Funk SE, Uman GC. Elevated body temperature independently contributes to increased length of stay in the neurologic intensive care unit patients. Crit Care Med. 2004;32:1489–95.
Naidech AM, Bendok BR, Tamul P, Bassin SL, Watts CM, Batjer HH, et al. Medical complications drive length of stay after brain hemorrhage: a cohort study. Neurocrit Care. 2009;10:11–9.
Oliveira-Filho J, Ezzeddine MA, Segal AZ, Buonanno FS, Chang Y, Ogilvy CS, et al. Fever in subarachnoid hemorrhage: relationship to vasospasm and outcome. Neurology. 2001;56:1299–304.
Mees SMD, Luitse MJ, van den Bergh WM, Rinkel GJ. Fever after aneurysmal subarachnoid hemorrhage: relation with extent of hydrocephalus and amount of extravasated blood. Stroke. 2008;39:2141–3.
Commichau C, Scarmeas N, Mayer SA. Risk factors for fever in the neurologic intensive care unit. Neurology. 2003;60:837–41.
Fernandez A, Schmidt JM, Claassen J, Pavlicova M, Huddleston D, Kreiter KT, et al. Fever after subarachnoid hemorrhage: risk factors and impact on outcome. Neurology. 2007;68:1013–9.
Todd MM, Hindman BJ, Clarke WR, Torner JC, Weeks JB, Bayman EO, et al. IHAST Investigators. Perioperative fever and outcome in surgical patients with aneurysmal subarachnoid hemorrhage. Neurosurgery. 2009;64:897–908.
Springer MV, Schmidt JM, Wartenberg KE, Frontera JA, Badjatia N, Mayer SA. Predictors of global cognitive impairment 1 year after subarachnoid hemorrhage. Neurosurgery. 2009;65:1043–50.
Wartenberg KE, Schmidt JM, Claassen J, Temes RE, Frontera JA, et al. Impact of medical complications on outcome after subarachnoid hemorrhage. Crit Care Med. 2006;34:617–23.
Naidech AM, Bendok BR, Bernstein RA, Alberts MJ, Batjer HH, Watts CM, et al. Fever burden and functional recovery after subarachnoid hemorrhage. Neurosurgery. 2008;63:212–7.
Rincon F, Hunter K, Schorr C, Dellinger RP, Zanotti-Cavazzoni S. The epidemiology of spontaneous fever and hypothermia on admission of brain injury patients to intensive care units: a multicenter cohort study. J Neurosurg. 2014;121:950–60.
Rincon F, et al. Brain injury as a risk factor for fever upon admission to the intensive care unit and association with in-hospital case fatality: a matched cohort study. J Intensive Care Med. 2015;30:107–14.
Diringer MN, et al. Critical care management of patients following aneurismal subarachnoid hemorrhage: recommendations from the neurocritical care society’s multidisciplinary consensus conference. Neurocrit Care. 2011;15:211–40.
Scaravilli V, Tenchero G, Citerio G. Fever management in SAH. Neurocrit Care. 2011;15:287–94.
Giraldo EA, Mandrekar JN, Rubin MN, Dupont SA, Zhang Giraldo EA, Mandrekar JN, et al. Timing of clinical grade assessment and poor outcome in patients with aneurysmal subarachnoid hemorrhage. J Neurosurg. 2012;117:15–9.
Rabinstein AA, Lanzino G, Wijdicks EF. Multidisciplinary management and emerging therapeutic strategies in aneurysmal subarachnoid haemorrhage. Lancet Neurol. 2010;9:504–19.
Van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988;19:604–7.
Rabinstein AA, Sandhu K. Non-infectious fever in the neurological intensive care unit: incidence, causes and predictors. J Neurol Neurosurg Psychiatry. 2007;78:1278–80.
Hocker SE, Tian L, Li G, Steckelberg JM, Mandrekar JN, Rabinstein AA. Indicators of central fever in the neurologic intensive care unit. JAMA Neurol. 2013;70:1499–504.
Yoshimoto Y, Tanaka Y, Hoya K. Acute systemic inflammatory response syndrome in subarachnoid hemorrhage. Stroke. 2001;32:1989–93.
Hanafy KA, Morgan Stuart R, Fernandez L, Schmidt JM, Claassen J, Lee K, et al. Cerebral inflammatory response and predictors of admission clinical grade after aneurysmal subarachnoid hemorrhage. J Clin Neurosci. 2010;17:22–5.
Badjatia N, Fernandez L, Schmidt JM, Lee K, Claassen J, Connolly ES, et al. Impact of induced normothermia on outcome after subarachnoid hemorrhage: a case-control study. Neurosurgery. 2010;66:696–700.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Drs. Kramer, Rabinstein, Pegoli, and Mandrekar report no disclosures. Dr. Lanzino reports a consultant relationship with eV3/Covidien and Codman.
Rights and permissions
About this article
Cite this article
Kramer, C.L., Pegoli, M., Mandrekar, J. et al. Refining the Association of Fever with Functional Outcome in Aneurysmal Subarachnoid Hemorrhage. Neurocrit Care 26, 41–47 (2017). https://doi.org/10.1007/s12028-016-0281-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-016-0281-7