Abstract
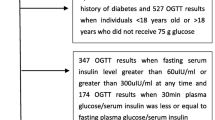
Type 2 diabetes mellitus (T2DM) is a heterogeneous disorder characterized by defects in insulin secretion and action and obesity plays an important role in the deterioration of glucose metabolism. In the present study we evaluated the degree of insulin resistance and first-phase insulin secretion of β-cell in obese subjects with normal glucose tolerance (NGT), impaired glucose tolerance (IGT), and T2DM in Chinese. A total of 220 subjects underwent standard 75 g oral glucose tolerance test (OGTT) and insulin-modified frequently sampled intravenous glucose tolerance test (FSIGT). Insulin sensitivity index (S I) was assessed by the reduced sample number (n = 12) of Bergman’s minimal model method with FSIGT. Insulin secretion capacities were determined by the insulinogenic index (I 30 min − I 0 min)/(G 30 min − G 0 min) in OGTT and the acute insulin response to glucose (AIR) in FSIGT. The disposition index (DI), the product of AIR and S I was used to determine whether AIR was adequate to compensate for insulin resistance. The S I in healthy lean control group was significantly higher than that in NGT, IGT, and T2DM group, but there was no significant difference among NGT, IGT, and T2DM group. The AIR in NGT group was significantly greater than that in control group, but then it was progressively decreased in IGT and T2DM group. The value of DI in control group was significantly higher than that in those three abnormal groups, and was decreased from NGT to IGT and T2DM group with significant difference. It indicates that obese subjects with different glucose tolerances have a similar degree of insulin resistance but differ in insulin secretion in Chinese Han population.
Similar content being viewed by others
References
C. Weyer, C. Bogardus, P.A. Tataranni, R.E. Pratley, Diabetes Care 24, 89–94 (2001)
C. Weyer, C. Bogardus, D.M. Mott, R.E. Pratley, J. Clin. Invest. 104, 787–794 (1999)
G. Pillonetto, G. Sparacino, P. Magni, R. Bellazzi, C. Cobelli, Am. J. Physiol. Endocrinol. Metab. 282, E564–E573 (2002)
S.M. Haffner, R. D’Aqostino, M.F. Saad et al., Diabetes 45(6), 742–748 (l996)
S.M. Haffner, G. Howard, E. Mayer et al., Diabetes 46(1), 63–69 (1997)
F.B. Hu, T.Y. Li, G.A. Colditz, W.C. Willett, J.E. Manson, JAMA 14, 1785–1791 (2003)
E. Ferrannini, S. Vichi, H. Beck-Nielsen, M. Laakso, G. Paolisso, U. Smith, Diabetes 45, 947–953 (1996)
E.J. Mayer-Davis, T. Costacou, Curr. Diab. Rep. 2, 170–176 (2001)
R.A. DeFronzo, Diabetes 28, 1095–1101 (1979)
M. Chen, R.N. Bergman, G. Pacini, D. Porte Jr., J. Clin. Endocrinol. Metab. 60, 13–20 (1985)
M. Annette, J.B. Chang Halter, Am. J. Physiol. Endocrinol. Metab. 284, E7–E12 (2003)
A. Fritsche, A. Madaus, N. Stefan et al., Diabetes 51, S234–S239 (2002)
W.Y. Fujimoto, S.L. Abbate, S.E. Kahn, J.E. Hokanson, J.D.␣Brunzell, Obes. Res. 2, 364–371 (1994)
K.M. Utzschneider, D.B. Carr, R.L. Hull et al., Diabetes 53, 2867–2872 (2004)
T. Kuzuya, Br J Nutr. 84(Suppl 2), S177–181 (2000)
Steering Committee of the Western Pacific Region of the World Health Organization, the International Association for the Study of Obesity, and the International Obesity Task Force. Melbourne, Australia: Health Communications Australia Pty Ltd, 2000
G.M. Steil, A. Volund, S.E. Kahn, R.N. Bergman, Diabetes 42, 250–256 (1993)
G. Pacini, G. Tonolo, M. Sambataro et al., Am J Physiol. 274(4 Pt 1), E592–599 (1998)
S.E. Kahn, D.L. Prigeon, D.K. McCulloch et al., Diabetes 42, 1663–1672 (1993)
Acknowledgments
This study was supported by grants from National Natural Science Foundation of China (No. 30570880). The authors would like to thank Professor Bergman RN for his generous support in providing the minimal model software for our clinical center.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hong, J., Gu, WQ., Zhang, YF. et al. The interplay of insulin resistance and β-cell dysfunction involves the development of type 2 diabetes in Chinese obeses. Endocr 31, 93–99 (2007). https://doi.org/10.1007/s12020-007-0002-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-007-0002-2