Opinion statement
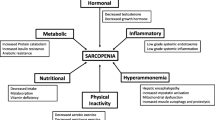
Most widely recognized complications in cirrhotic patients include ascites, hepatic encephalopathy, variceal bleeding, kidney dysfunction, and hepatocellular carcinoma; however, malnutrition and muscle wasting (sarcopenia) constitute common complications which negatively impact survival, quality of life, and response to stressors, such as infection and surgery in patients with cirrhosis. Despite the important role that malnutrition and sarcopenia play in the prognosis of patients with cirrhosis, they are frequently overlooked, in part because nutritional assessment can be a difficult task in patients with cirrhosis due to fluid retention and/or overweight. Moreover, patients with cirrhosis may develop simultaneous loss of skeletal muscle and gain of adipose tissue, culminating in the condition of “sarcopenic obesity.” In addition, muscle depletion is characterized by both a reduction in muscle size and increased proportion of intermuscular and intramuscular fat-denominated “myosteatosis.” Sarcopenia in cirrhotic patients has been associated with increased mortality, sepsis complications, hyperammonemia, overt hepatic encephalopathy, and increased length of stay after liver transplantation. Muscularity assessment with cross-sectional imaging studies has become an attractive index of nutritional status evaluation in cirrhosis, as sarcopenia reflects a chronic detriment in general physical condition, rather than acute severity of the liver disease. In this review, we discuss the current diagnostic methods to evaluate malnutrition and muscle abnormalities in cirrhosis and also analyze the current knowledge regarding incidence and clinical impact of malnutrition and muscle abnormalities in cirrhosis and their impact after liver transplantation. We also discuss existing and potential novel therapeutic strategies for malnutrition in cirrhosis, emphasizing the recognition of sarcopenia in cirrhosis in an effort to improve survival and reduce morbidity related to cirrhosis. Finally, we analyze new studies including sarcopenia with the MELD score that seems to allow better prediction of mortality among cirrhotic patients waiting for liver transplantation.

Similar content being viewed by others
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Periyalwar P, Dasarathy S. Malnutrition in cirrhosis: contribution and consequences of sarcopenia on metabolic and clinical responses. Clin Liver Dis. 2012;16:95–131.
Montano-Loza AJ, Meza-Junco J, Prado CM, Lieffers JR, Baracos VE, Bain VG, et al. Muscle wasting is associated with mortality in patients with cirrhosis. Clin Gastroenterol Hepatol. 2011;10:166–73. The initial paper describing the association of sarcopenia measured by CT and increase mortality in patients with cirrhosis.
D’Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol. 2006;44:217–31.
Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60:646–9.
Kamath PS, Kim WR. The model for end-stage liver disease (MELD). Hepatology. 2007;45:797–805.
Montano-Loza AJ, Angulo P, Meza-Junco J, Prado CMM, Sawyer MB, Beaumont C, et al. Sarcopenic obesity and myosteatosis are associated with higher mortality in patients with cirrhosis. J Cachexia Sarcopenia Muscle 2016; In press. This paper describes the frequency of sarcopenic obesity and myosteatosis and its association with increase mortality in patients with cirrhosis.
Johnson TM, Overgard EB, Cohen AE, DiBaise JK. Nutrition assessment and management in advanced liver disease. Nutr Clin Pract. 2013;28:15–29. This review describes nutritional assessment tools and general principles in the nutritional support of patients with advanced liver disease.
O’Brien A, Williams R. Nutrition in end-stage liver disease: principles and practice. Gastroenterology. 2008;134:1729–40.
Montano-Loza AJ. Skeletal muscle abnormalities and outcomes after liver transplantation. Liver Transpl. 2014;20:1293–5.
Gallagher D, Kuznia P, Heshka S, Albu J, Heymsfield SB, Goodpaster B, et al. Adipose tissue in muscle: a novel depot similar in size to visceral adipose tissue. Am J Clin Nutr. 2005;81:903–10.
Petersen KF, Befroy D, Dufour S, Dziura J, Ariyan C, Rothman DL, et al. Mitochondrial dysfunction in the elderly: possible role in insulin resistance. Science. 2003;300:1140–2.
Visser M, Goodpaster BH, Kritchevsky SB, Newman AB, Nevitt M, Rubin SM, et al. Muscle mass, muscle strength, and muscle fat infiltration as predictors of incident mobility limitations in well-functioning older persons. J Gerontol a-Biol. 2005;60:324–33.
Schrager MA, Metter EJ, Simonsick E, Ble A, Bandinelli S, Lauretani F, et al. Sarcopenic obesity and inflammation in the InCHIANTI study. J Appl Physiol. 2007;102:919–25.
Kim TN, Park MS, Lim KI, Choi HY, Yang SJ, Yoo HJ, et al. Relationships between sarcopenic obesity and insulin resistance, inflammation, and vitamin D status: the Korean Sarcopenic Obesity Study. Clin Endocrinol. 2013;78:525–32. This Korean sarcopenic obesity study showed that HOMA-IR and 25[OH]D levels were independently associated with sarcopenic obesity in men, while HOMA-IR and hsCRP were significant factors predicting sarcopenic obesity in women.
Plevak DJ, Dicecco SR, Wiesner RH, Porayko MK, Wahlstrom HE, Janzow DJ, et al. Nutritional support for liver-transplantation—identifying caloric and protein-requirements. Mayo Clin Proc. 1994;69:225–30.
Montano-Loza AJ. New concepts in liver cirrhosis: clinical significance of sarcopenia in cirrhotic patients. Minerva Gastroenterol Dietol. 2013;59:173–86.
Quigley EMM. Gastrointestinal dysfunction in liver disease and portal hypertension—gut-liver interactions revisited. Digest Dis Sci. 1996;41:557–61.
Kalaitzakis E, Bosaeus I, Ohman L, Bjornsson E. Altered postprandial glucose, insulin, leptin, and ghrelin in liver cirrhosis: correlations with energy intake and resting energy expenditures. Am J Clin Nutr. 2007;85:808–15.
Lemoine O, Marchant A, Degroote D, Azar C, Goldman M, Deviere J. Role of defective monocyte interleukin-10 release in tumor-necrosis-factor-alpha overproduction in alcoholic cirrhosis. Hepatology. 1995;22:1436–9.
Madden AM, Bradbury W, Morgan MY. Taste perception in cirrhosis: its relationship to circulating micronutrients and food preferences. Hepatology. 1997;26:40–8.
Bergheim I, Parlesak A, Dierks C, Bode JC, Bode C. Nutritional deficiencies in German middle-class male alcohol consumers: relation to dietary intake and severity of liver disease. Eur J Clin Nutr. 2003;57:431–8.
Montano-Loza AJ. Muscle wasting: a nutritional criterion to prioritize patients for liver transplantation. Curr Opin Clin Nutr. 2014;17:219–25.
Baumgartner RN, Koehler KM, Gallagher D, Romero L, Heymsfield SB, Ross RR, et al. Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol. 1998;147:755–63.
Marcell TJ. Sarcopenia: causes, consequences, and preventions. J Gerontol A Biol Sci Med Sci. 2003;58:911–6.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39:412–23.
Elliott JM, Kerry R, Flynn T, Parrish TB. Content not quantity is a better measure of muscle degeneration in whiplash. Manual Ther. 2013;18:578–82.
Lang T, Streeper T, Cawthon P, Baldwin K, Taaffe DR, Harris TB. Sarcopenia: etiology, clinical consequences, intervention, and assessment. Osteoporos Int. 2010;21:543–59.
Kim HY, Jang JW. Sarcopenia in the prognosis of cirrhosis: going beyond the MELD score. World J Gastroenterol. 2015;21:7637–47. This review describes the role of sarcopenia in determining the prognosis of patients with cirrhosis. It also discusses the role of sarcopenia alone or in combination with MELD in the assessment of prognosis of patients with cirrhosis.
Meza-Junco J, Montano-Loza AJ, Baracos VE, Prado CM, Bain VG, Beaumont C, et al. Sarcopenia as a prognostic index of nutritional status in concurrent cirrhosis and hepatocellular carcinoma. J Clin Gastroenterol. 2013;47:861–70.
Tandon P, Ney M, Irwin I, Ma MM, Gramlich L, Bain VG, et al. Severe muscle depletion in patients on the liver transplant wait list: its prevalence and independent prognostic value. Liver Transplant. 2012;18:1209–16.
Montano-Loza AJ, Meza-Junco J, Baracos VE, Prado CM, Ma M, Meeberg G, et al. Severe muscle depletion predicts postoperative length of stay but is not associated with survival after liver transplantation. Liver Transpl. 2014;20:640–8.
Cruz RJ, Dew MA, Myaskovsky L, Goodpaster B, Fox K, Fontes P, et al. Objective radiologic assessment of body composition in patients with end-stage liver disease: going beyond the BMI. Transplantation. 2013;95:617–22.
Masuda T, Shirabe K, Ikegami T, Harimoto N, Yoshizumi T, Soejima Y, et al. Sarcopenia is a prognostic factor in living donor liver transplantation. Liver Transplant. 2014;20:401–7. This study showed that sarcopenia is an independent predictor of mortality and sepsis after living donor transplantation. They also showed that the occurrence of post operative sepsis decreased in patients with sarcopenia after routine application of early enteral nutrition.
Englesbe MJ, Patel SP, He K, Lynch RJ, Schaubel DE, Harbaugh C, et al. Sarcopenia and mortality after liver transplantation. J Am Coll Surg. 2010;211:271–8.
Krell RW, Kaul DR, Martin AR, Englesbe MJ, Sonnenday CJ, Cai S, et al. Association between sarcopenia and the risk of serious infection among adults undergoing liver transplantation. Liver Transpl 2013;19:1396-402.
Shen W, Punyanitya M, Wang ZM, Gallagher D, St-Onge MP, Albu J, et al. Total body skeletal muscle and adipose tissue volumes: estimation from a single abdominal cross-sectional image. J Appl Physiol. 2004;97:2333–8.
Kim TY, Kim MY, Sohn JH, Kim SM, Ryu JA, Lim S, et al. Sarcopenia as a useful predictor for long-term mortality in cirrhotic patients with ascites. J Korean Med Sci. 2014;29:1253–9.
Durand F, Buyse S, Francoz C, Laouenan C, Bruno O, Belghiti J, et al. Prognostic value of muscle atrophy in cirrhosis using psoas muscle thickness on computed tomography. J Hepatol. 2014;60:1151–7. In this study transversal psoas muscle thickness/height on CT at the level of the umbilicus was an objective marker of sarcopenia was predictive of mortality in cirrhotic patients. This was independent of the MELD and MELD-Na scores.
Beneke R, Neuerburg J, Bohndorf K. Muscle cross-section measurement by magnetic resonance-imaging. Eur J Appl Physiol O. 1991;63:424–9.
Parry SM, El-Ansary D, Cartwright MS, Sarwal A, Berney S, Koopman R, et al. Ultrasonography in the intensive care setting can be used to detect changes in the quality and quantity of muscle and is related to muscle strength and function. J Crit Care. 2015;30:1151.e9–1151.e14.
Horber FF, Thomi F, Casez JP, Fonteille J, Jaeger P. Impact of hydration status on body composition as measured by dual energy X-ray absorptiometry in normal volunteers and patients on haemodialysis. Br J Radiol. 1992;65:895–900.
Pirlich M, Schutz T, Spachos T, Ertl S, Weiss ML, Lochs H, et al. Bioelectrical impedance analysis is a useful bedside technique to assess malnutrition in cirrhotic patients with and without ascites. Hepatology. 2000;32:1208–15.
Madden AM, Morgan MY. The potential role of dual-energy X-ray absorptiometry in the assessment of body composition in cirrhotic patients. Nutrition. 1997;13:40–5.
Fiore P, Merli M, Andreoli A, De Lorenzo A, Masini A, Ciuffa L, et al. A comparison of skinfold anthropometry and dual-energy X-ray absorptiometry for the evaluation of body fat in cirrhotic patients. Clin Nutr. 1999;18:349–51.
Selberg O, Selberg D. Norms and correlates of bioimpedance phase angle in healthy human subjects, hospitalized patients, and patients with liver cirrhosis. Eur J Appl Physiol. 2002;86:509–16.
Toshikuni N, Arisawa T, Tsutsumi M. Nutrition and exercise in the management of liver cirrhosis. World J Gastroenterol. 2014;20:7286–97.
Singal AK, Kamath PS, Francisco Ziller N, DiCecco S, Shoreibah M, Kremers W, et al. Nutritional status of patients with alcoholic cirrhosis undergoing liver transplantation: time trends and impact on survival. Transpl Int. 2013;26:788–94.
Baker JP, Detsky AS, Wesson DE, Wolman SL, Stewart S, Whitewell J, et al. Nutritional assessment: a comparison of clinical judgement and objective measurements. N Engl J Med. 1982;306:969–72.
Pikul J, Sharpe MD, Lowndes R, Ghent CN. Degree of preoperative malnutrition is predictive of postoperative morbidity and mortality in liver transplant recipients. Transplantation. 1994;57:469–72.
Hirsch S, Bunout D, Delamaza P, Iturriaga H, Petermann M, Icazar G, et al. Controlled trial on nutrition supplementation in outpatients with symptomatic alcoholic cirrhosis. Jpen-Parenter Enter. 1993;17:119–24.
Alvares-da-Silva MR, Reverbel da Silveira T. Comparison between handgrip strength, subjective global assessment, and prognostic nutritional index in assessing malnutrition and predicting clinical outcome in cirrhotic outpatients. Nutrition. 2005;21:113–7.
Roberts HC, Denison HJ, Martin HJ, Patel HP, Syddall H, Cooper C, et al. A review of the measurement of grip strength in clinical and epidemiological studies: towards a standardised approach. Age Ageing. 2011;40:423–9.
Goodpaster BH, Park SW, Harris TB, Kritchevsky SB, Nevitt M, Schwartz AV, et al. The loss of skeletal muscle strength, mass, and quality in older adults: the health, aging and body composition study. J Gerontol a-Biol. 2006;61:1059–64.
Alameri HF, Sanai FM, Al Dukhayil M, Azzam NA, Al-Swat KA, Hersi AS, et al. Six minute walk test to assess functional capacity in chronic liver disease patients. World J Gastroenterol. 2007;13:3996–4001.
Carey EJ, Steidley DE, Aqel BA, Byrne TJ, Mekeel KL, Rakela J, et al. Six-minute walk distance predicts mortality in liver transplant candidates. Liver Transpl. 2010;16:1373–8.
Glass C, Hipskind P, Tsien C, Malin SK, Kasumov T, Shah SN, et al. Sarcopenia and a physiologically low respiratory quotient in patients with cirrhosis: a prospective controlled study. J Appl Physiol. 2013;114:559–65. In this study, patients with cirrhosis low respiratory quotient were accompanied by low muscle mass. This indicated a decompensated metabolic state that should be managed by improved nutritional support to improve muscle mass.
Mowat NAG, Edwards CRW, Fisher R, Mcneilly AS, Green JRB, Dawson AM. Hypothalamic-pituitary-gonadal function in men with cirrhosis of liver. Gut. 1976;17:345–50.
Qiu J, Tsien C, Thapalaya S, Narayanan A, Weihl CC, Ching JK, et al. Hyperammonemia-mediated autophagy in skeletal muscle contributes to sarcopenia of cirrhosis. Am J Physiol Endocrinol Metab. 2012;303:E983–993.
Kovarik M, Muthny T, Sispera L, Holecek M. The dose-dependent effects of endotoxin on protein metabolism in two types of rat skeletal muscle. J Physiol Biochem. 2012;68:385–95.
Changani KK, Jalan R, Cox IJ, Ala-Korpela M, Bhakoo K, Taylor-Robinson SD, et al. Evidence for altered hepatic gluconeogenesis in patients with cirrhosis using in vivo 31-phosphorus magnetic resonance spectroscopy. Gut. 2001;49:557–64.
Montanari A, Simoni I, Vallisa D, Trifiro A, Colla R, Abbiati R, et al. Free amino acids in plasma and skeletal muscle of patients with liver cirrhosis. Hepatology. 1988;8:1034–9.
Montano-Loza AJ, Duarte-Rojo A, Bhanji R, Rose C. Cirrhotic patients with sarcopenia and sarcopenic-obesity have an increased risk of hyperammonemia and hepatic encephalopathy. Am J Gastroenterol. 2015;110:S875–5.
Glass D, Roubenoff R. Recent advances in the biology and therapy of muscle wasting. Ann Ny Acad Sci. 2010;1211:25–36.
Ruegg MA, Glass DJ. Molecular mechanisms and treatment options for muscle wasting diseases. Annu Rev Pharmacol. 2011;51:373–95.
Dickinson JM, Fry CS, Drummond MJ, Gundermann DM, Walker DK, Glynn EL, et al. Mammalian target of rapamycin complex 1 activation is required for the stimulation of human skeletal muscle protein synthesis by essential amino acids. J Nutr. 2011;141:856–62.
Drummond MJ, Bell JA, Fujita S, Dreyer HC, Glynn EL, Volpi E, et al. Amino acids are necessary for the insulin-induced activation of mTOR/S6K1 signaling and protein synthesis in healthy and insulin resistant human skeletal muscle. Clin Nutr. 2008;27:447–56.
Drummond MJ, Glynn EL, Fry CS, Timmerman KL, Volpi E, Rasmussen BB. An increase in essential amino acid availability upregulates amino acid transporter expression in human skeletal muscle. Am J Physiol-Endoc M. 2010;298:E1011–8.
Montano-Loza AJ. Clinical relevance of sarcopenia in patients with cirrhosis. World J Gastroentero. 2014;20:8061–71.
Merion RM, Wolfe RA, Dykstra DM, Leichtman AB, Gillespie B, Held PJ. Longitudinal assessment of mortality risk among candidates for liver transplantation. Liver Transpl. 2003;9:12–8.
Kim WR, Biggins SW, Kremers WK, Wiesner RH, Kamath PS, Benson JT, et al. Hyponatremia and mortality among patients on the liver-transplant waiting list. N Engl J Med. 2008;359:1018–26.
Myers RP, Shaheen AA, Faris P, Aspinall AI, Burak KW. Revision of MELD to include serum albumin improves prediction of mortality on the liver transplant waiting list. PLoS One. 2013;8, e51926.
DiMartini A, Cruz RJ, Dew MA, Myaskovsky L, Goodpaster B, Fox K, et al. Muscle mass predicts outcomes following liver transplantation. Liver Transplant. 2013;19:1172–80.
Montano-Loza AJ, Duarte-Rojo A, Meza-Junco J, Baracos VE, Sawyer MB, Pang JXQ, et al. Inclusion of sarcopenia within MELD (MELD-sarcopenia) and the prediction of mortality in patients with cirrhosis. Clin Transl Gastroenterol. 2015;6:e102. In this study, MELD sarcopenia (defined by L3 skeletal muscle index) was calculated combining MELD score and sarcopenia. MELD-sarcopenia was associated with improved prediction of mortality in patients with cirrhosis, primarily in patients with low MELD score.
Norman K, Kirchner H, Lochs H, Pirlich M. Malnutrition affects quality of life in gastroenterology patients. World J Gastroenterol. 2006;12:3380–5.
Alberino F, Gatta A, Amodio P, Merkel C, Di Pascoli L, Boffo G, et al. Nutrition and survival in patients with liver cirrhosis. Nutrition. 2001;17:445–50.
Hanai T, Shiraki M, Nishimura K, Ohnishi S, Imai K, Suetsugu A, et al. Sarcopenia impairs prognosis of patients with liver cirrhosis. Nutrition. 2015;31:193–9. In this study, sarcopenia was associated with increased mortality in patients with cirrhosis and branched chain amino acid supplementation improved survival in sarcopenic patients.
Cosqueric G, Sebag A, Ducolombier C, Thomas C, Piette F, Weill-Engerer S. Sarcopenia is predictive of nosocomial infection in care of the elderly. Brit J Nutr. 2006;96:895–901.
Merli M, Lucidi C, Giannelli V, Giusto M, Riggio O, Falcone M, et al. Cirrhotic patients are at risk for health care-associated bacterial infections. Clin Gastroenterol Hepatol. 2010;8:979–85.
Montano-Loza AJ, Duarte-Rojo A, Rose CF. Sarcopenia and myosteatosis increase the risk of hepatic encephalopathy in cirrhotic patients. Hepatology. 2014;60:384a–5a.
Donaghy A, Ross R, Wicks C, Hughes SC, Holly J, Gimson A, et al. Growth hormone therapy in patients with cirrhosis: a pilot study of efficacy and safety. Gastroenterology. 1997;113:1617–22.
Moller S, Becker U, Gronbaek M, Juul A, Winkler K, Skakkebaek NE. Short-term effect of recombinant human growth-hormone in patients with alcoholic cirrhosis. J Hepatol. 1994;21:710–7.
Tsien CD, McCullough AJ, Dasarathy S. Late evening snack: exploiting a period of anabolic opportunity in cirrhosis. J Gastroen Hepatol. 2012;27:430–41.
Dasarathy S, McCullough AJ, Muc S, Schneyer A, Bennett CD, Dodig M, et al. Sarcopenia associated with portosystemic shunting is reversed by follistatin. J Hepatol. 2011;54:915–21.
Fry CS, Drummond MJ, Glynn EL, Dickinson JM, Gundermann DM, Timmerman KL, et al. Aging impairs contraction-induced human skeletal muscle mTORC1 signaling and protein synthesis. Skelet Muscle. 2011;1:1–11.
Dreyer HC, Drummond MJ, Pennings B, Fujita S, Glynn EL, Chinkes DL, et al. Leucine-enriched essential amino acid and carbohydrate ingestion following resistance exercise enhances mTOR signaling and protein synthesis in human muscle. Am J Physiol Endocrinol Metab. 2008;294:E392–400.
Bonetto A, Penna F, Minero VG, Reffo P, Costamagna D, Bonelli G, et al. Glutamine prevents myostatin hyperexpression and protein hypercatabolism induced in C2C12 myotubes by tumor necrosis factor-alpha. Amino Acids. 2011;40:585–94.
Teran JC, Mullen KD, Mccullough AJ. Glutamine—a conditionally essential amino-acid in cirrhosis. Am J Clin Nutr. 1995;62:897–900.
Marchesini G, Dioguardi FS, Bianchi GP, Zoli M, Bellati G, Roffi L, et al. Long-term oral branched-chain amino-acid treatment in chronic hepatic-encephalopathy—a randomized double-blind casein-controlled trial. J Hepatol. 1990;11:92–101.
Mcghee A, Henderson JM, Millikan WJ, Bleier JC, Vogel R, Kassouny M, et al. Comparison of the effects of hepatic-aid and a casein modular diet on encephalopathy, plasma amino-acids, and nitrogen-balance in cirrhotic-patients. Ann Surg. 1983;197:288–93.
Horst D, Grace ND, Conn HO, Schiff E, Schenker S, Viteri A, et al. Comparison of dietary-protein with an oral, branched-chain enriched amino-acid supplement in chronic portal-systemic encephalopathy—a randomized controlled trial. Hepatology. 1984;4:279–87.
Christie ML, Sack DM, Pomposelli J, Horst D. Enriched branched-chain amino-acid formula versus a casein-based supplement in the treatment of cirrhosis. Jpen-Parenter Enter. 1985;9:671–8.
Swart GR, Vandenberg JWO, Vanvuure JK, Rietveld T, Wattimena DL, Frenkel M. Minimum protein-requirements in liver-cirrhosis determined by nitrogen-balance measurements at 3 levels of protein-intake. Clin Nutr. 1989;8:329–36.
Egberts EH, Schomerus H, Hamster W, Jurgens P. Branched-chain amino-acids in the treatment of latent portosystemic encephalopathy—a double-blind placebo-controlled crossover study. Gastroenterology. 1985;88:887–95.
Muto Y, Sato S, Watanabe A, Moriwaki H, Suzuki K, Kato A, et al. Effects of oral branched-chain amino acid granules on event-free survival in patients with liver cirrhosis. Clin Gastroenterol Hepatol. 2005;3:705–13.
Muto Y, Sato S, Watanabe A, Moriwaki H, Suzuki K, Kato A, et al. Overweight and obesity increase the risk for liver cancer in patients with liver cirrhosis and long-term oral supplementation with branched-chain amino acid granules inhibits liver carcinogenesis in heavier patients with liver cirrhosis. Hepatol Res. 2006;35:204–14.
Berzigotti A, Saran U, Dufour JF. Physical activity and liver diseases. Hepatology 2016. In press.
Hayashi F, Matsumoto Y, Momoki C, Yuikawa M, Okada G, Hamakawa E, et al. Physical inactivity and insufficient dietary intake are associated with the frequency of sarcopenia in patients with compensated viral liver cirrhosis. Hepatol Res. 2013;43:1264–75.
Wilborn CD, Taylor LW, Greenwood M, Kreider RB, Willoughby DS. Effects of different intensities of resistance exercise on regulators of myogenesis. J Strength Cond Res. 2009;23:2179–87.
Kaido T, Ogawa K, Fujimoto Y, Ogura Y, Hata K, Ito T, et al. Impact of sarcopenia on survival in patients undergoing living donor liver transplantation. Am J Transplant. 2013;13:1549–56. This study found that skeletal muscle depletion was closely involved with posttransplant mortality in patients undergoing living donor liver transplantation. Perioperative nutritional therapy significantly improved overall survival in cirrhotic patients with skeletal muscle depletion.
Yamauchi M, Takeda K, Sakamoto K, Ohata M, Toda G. Effect of oral branched chain amino acid supplementation in the late evening on the nutritional state of patients with liver cirrhosis. Hepatol Res. 2001;21:199–204.
Les I, Doval E, Garcia-Martinez R, Planas M, Cardenas G, Gomez P, et al. Effects of branched-chain amino acids supplementation in patients with cirrhosis and a previous episode of hepatic encephalopathy: a randomized study. Am J Gastroenterol. 2011;106:1081–8.
Tsien C, Shah SN, McCullough AJ, Dasarathy S. Reversal of sarcopenia predicts survival after a transjugular intrahepatic portosystemic stent. Eur J Gastroenterol Hepatol. 2013;25:85–93. This study demonstrated that some cirrhotic patients have reversal of sarcopenia after transjugular intrahepatic portosystemic stents, and this fining was associated with better survival.
Roman E, Torrades MT, Nadal MJ, Cardenas G, Nieto JC, Vidal S, et al. Randomized pilot study: effects of an exercise programme and leucine supplementation in patients with cirrhosis. Dig Dis Sci. 2014;59:1966–75.
Zenith L, Meena N, Ramadi A, Yavari M, Harvey A, Carbonneau M, et al. Eight weeks of exercise training increases aerobic capacity and muscle mass and reduces fatigue in patients with cirrhosis. Clin Gastroenterol Hepatol. 2014;12:1920–1926 e1922. This prospective controlled pilot trial showed that 8 weeks of supervised aerobic exercise training led to increase in peak exercise oxygen uptake and muscle mass and reduced fatigue in patients with cirrhosis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Ragesh B. Thandassery and Aldo J. Montano-Loza declare that they have no conflict of interest.
Human and animal rights and informed consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Liver
Rights and permissions
About this article
Cite this article
Thandassery, R.B., Montano-Loza, A.J. Role of Nutrition and Muscle in Cirrhosis. Curr Treat Options Gastro 14, 257–273 (2016). https://doi.org/10.1007/s11938-016-0093-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11938-016-0093-z