Abstract
Purpose of Review
To examine the impact of the new 2017 ACC/AHA hypertension guideline on the prevalence of hypertension, its constituent ratio, and their associated factors in southwest China.
Recent Findings
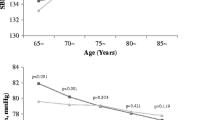
A total of 14,220 permanent residents ≥ 18 years were enrolled in this survey. According to the 2017 ACC/AHA hypertension guideline, the hypertension prevalence was substantially increased (46.9% vs. 24.5%); consistent across different age and gender groups, while the hypertension awareness (23.8% vs. 45.6%); treatment (18.6% vs. 35.5%); control (2.3% vs. 11.2%); and control among treatment (9.6% vs. 24.0%) patients were decreased in southwest of China. In our cohort, 31.1% participants were newly diagnosed as hypertension. Young adults accounted considerable proportion in this newly diagnosed hypertension population. The proportion of young hypertensive individuals substantially increased, whereas those of the older hypertensive subjects decreased. Among the hypertensive subjects aged ≥ 65 years undergoing treatment, 90% of the elderly subjects were not eligible for hypertension control and 32.5% have systolic blood pressure control at 130–149 mmHg, and thus need to intensify antihypertensive treatment according to 2017 ACC/AHA hypertension guideline. Smoking, drinking, body fat percentage, and body mass index were considered the factors associated with hypertension according to the Chinese hypertension guideline but not in the 2017 ACC/AHA hypertension guideline.
Summary
The adoption of the 2017 ACC/AHA hypertension guideline will substantially increase hypertension prevalence in southwest of China. The new definition of hypertension implies that more young adults will likely suffer from high cardiovascular risks, while additional one third of elder hypertensive subjects will likely need intensified antihypertension treatments.




Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Xu X, Byles J, Shi Z, McElduff P, Hall J. Dietary pattern transitions, and the associations with BMI, waist circumference, weight and hypertension in a 7-year follow-up among the older Chinese population: a longitudinal study. BMC Public Health. 2016;16(743):743. https://doi.org/10.1186/s12889-016-3425-y.
Dzau V, Braunwald E. Resolved and unresolved issues in the prevention and treatment of coronary artery disease: a workshop consensus statement. Am Heart J. 1991;121(1):1244–63. https://doi.org/10.1016/0002-8703(91)90694-D.
RS V, MG L, EP L, et al. Impact of high-normal blood pressure on the risk of cardiovascular disease. ACC Curr J Rev. 2001;11(2):31–1. https://doi.org/10.1016/S1062-1458(02)00536-6.
Zhou M, Wang H, Zhu J, Chen W, Wang L, Liu S, et al. Cause-specific mortality for 240 causes in China during 1990–2013: a systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet. 2016;387(10015):251–72. https://doi.org/10.1016/S0140-6736(15)00551-6.
World Health Organization. A global brief on hypertension : silent killer, global public health crisis: World Health Day 2013. World Health Organization. 2013. http://www.who.int/iris/handle/10665/79059.
Feng XL, Pang M, Beard J. Health system strengthening and hypertension awareness, treatment and control: data from the China Health and Retirement Longitudinal Study. Bull World Health Organ. 2014;92(1):29–41. https://doi.org/10.2471/BLT.13.124495.
Liu L, Wang D, Wong KS, et al. Stroke and stroke care in China: huge burden, significant workload, and a national priority. Stroke. 2011;42(12):3651–4. https://doi.org/10.1161/STROKEAHA.111.635755.
Yang G, Kong L, Zhao W, Wan X, Zhai Y, Chen LC, et al. Emergence of chronic non-communicable diseases in China. Lancet. 2008;372(9650):1697–705. https://doi.org/10.1016/S0140-6736(08)61366-5.
Lewington S, Lacey B, Clarke R, Guo Y, Kong XL, Yang L, et al. The burden of hypertension and associated risk for cardiovascular mortality in China. JAMA Intern Med. 2016;176(4):524–32. https://doi.org/10.1001/jamainternmed.2016.0190.
•• Li Y, Yang L, Wang L, et al. Burden of hypertension in China: a nationally representative survey of 174,621 adults. Int J Cardiol. 2017;227:516–23. https://doi.org/10.1016/j.ijcard.2016.10.110 This epidemiological study describes the severe burden of hypertension in China from the aspects of hypertension prevalence, awareness, treatment, and control rates.
•• Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2018;71(19):e127–248. https://doi.org/10.1016/j.jacc.2017.11.006 This comprehensive guideline redefines the hypertension criteria which will have a major impact on the assessment and management of hypertension around the world.
•• Muntner P, Carey RM, Gidding S, et al. Potential US population impact of the 2017 ACC/AHA high blood pressure guideline. Circulation. 2018;137(2):109–18. https://doi.org/10.1161/CIRCULATIONAHA.117.032582 This article carefully analyzes the potential impact of new hypertension guidelines on the assessment and management of hypertension in the USA.
Liu X, Gu W, Li Z, Lei H, Li G, Huang W. Hypertension prevalence, awareness, treatment, control, and associated factors in Southwest China: an update. J Hypertens. 2017;35(3):637–44. https://doi.org/10.1097/HJH.0000000000001203.
Wang JG. Chinese hypertension guidelines. Pulse (Basel). 2015;3(1):14–20. https://doi.org/10.1159/000382025.
• Yang C, Wang J, Gao B, et al. Prevalence and treatment of hypertension in China: impacts of 2017 American College of Cardiology/American Heart Association High Blood Pressure Guideline. Sci Bull. 2018;63(8):488–93. https://doi.org/10.1016/j.scib.2018.03.006 This article analyzes the impact of new guidelines on hypertension prevalence and treatment in China.
• Khera R, Lu Y, Lu J, et al. Impact of 2017 ACC/AHA guidelines on prevalence of hypertension and eligibility for antihypertensive treatment in United States and China: nationally representative cross sectional study. Bmj. 2018;362:k2357. https://doi.org/10.1136/bmj.k2357 The study analyzes the effects of the 2017 ACC/AHA guidelines on the prevalence of hypertension and antihypertensive treatment in the USA and China.
Beckett NS, Peters R, Fletcher AE, Staessen JA, Liu L, Dumitrascu D, et al. Treatment of hypertension in patients 80 years of age or older. Minerva Med. 2008;100(1):25. https://doi.org/10.1056/NEJMoa0801369.
Listed N. Cholesterol, diastolic blood pressure, and stroke: 13,000 strokes in 450,000 people in 45 prospective cohorts. Prospective studies collaboration. Lancet. 1995; 346(8991-8992):1647–1653. https://doi.org/10.1016/S0140-6736(95)92836-7.
Franklin SS, Wong ND, Kannel WB. Age-specific relevance of usual blood pressure to vascular mortality. Lancet. 2002;361(9366):1389–90. https://doi.org/10.1016/S0140-6736(03)13062-0.
Group SR, Wright JT Jr, Williamson JD, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373(22):2103–16. https://doi.org/10.1056/NEJMoa1511939.
Kearney PM, Whelton M, Reynolds K, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2016;42(8):2103–16. https://doi.org/10.1056/NEJMx170008.
Group SS, Benavente OR, Coffey CS, et al. Blood-pressure targets in patients with recent lacunar stroke: the SPS3 randomised trial. Lancet. 2013;382(9891):507–15. https://doi.org/10.1016/S0140-6736(13)60852-1.
Martell-Claros N, Cruz JJDL. Manidipine for hypertension not controlled by dual therapy in patients with diabetes mellitus. Clin Drug Investig. 2011;31(6):427–34. https://doi.org/10.2165/11587400-000000000-00000.
•• Lacey B, Lewington S, Clarke R, et al. Age-specific association between blood pressure and vascular and non-vascular chronic diseases in 0·5 million adults in China: a prospective cohort study. Lancet Global Health. 2018;6(6):e641–9. https://doi.org/10.1016/S2214-109X(18)30217-1 This study analyzes the age-specific association between blood pressure and vascular and nonvascular chronic diseases in China and suggest the highly association of blood pressure with intracerebral haemorrhage and ischaemic stroke in Chinese population.
•• Messerli FH, Bangalore S, Messerli AW. Age, blood pressure targets, and guidelines: rift between those who preach, those who teach, and those who treat? Circulation. 2018;138(2):128–30. https://doi.org/10.1161/CIRCULATIONAHA.118.034390 This very useful review describes the effect of age on blood pressure and the blood presuure for the elder people..
Rakugi H, Ogihara T, Goto Y, et al. Comparison of strict- and mild-blood pressure control in elderly hypertensive patients: a per-protocol analysis of JATOS. Hypertens Res. 2010;33(11):1124–8. https://doi.org/10.1038/hr.2010.144.
Somes GW, Pahor M, Shorr RI, Cushman WC, Applegate WB. The role of diastolic blood pressure when treating isolated systolic hypertension. Arch Int Med. 1999;159(17):2004. https://doi.org/10.1001/archinte.159.17.2004.
Peng J, Lu F, Wang Z, Zhong M, Sun L, Hu N, et al. Excessive lowering of blood pressure is not beneficial for progression of brain white matter hyperintensive and cognitive impairment in elderly hypertensive patients: 4-year follow-up study. J Am Med Dir Assoc. 2014;15(12):904–10. https://doi.org/10.1016/j.jamda.2014.07.005.
Liu P, Zheng JG. Blood pressure targets in the hypertensive elderly. Chin Med J. 2017;130(16):1968. https://doi.org/10.4103/0366?6999.211885.
Chaudhry KN, Chavez P, Gasowski J, et al. Hypertension in the elderly: some practical considerations. Cleve Clin J Med. 2012;79(10):694–704. https://doi.org/10.3949/ccjm.79a.12017.
Hollenberg NK. Hypertension in an aging population: problems and opportunities. Am J Med. 1991;90(4B):1S–2S. https://doi.org/10.1016/0002-9343(91)90471-9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
This study was approved by the Ethics Committee of the First Affiliated Hospital of Chongqing Medical University and all subjects signed informed consent for data collection and analyses prior to participation.
Dan Li, Xiaofang Zeng, Yi Huang, Han Lei, Ge Li, Nan Zhang, and Wei Huang declare that they no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Guidelines/Clinical Trials/Meta-Analysis
Rights and permissions
About this article
Cite this article
Li, D., Zeng, X., Huang, Y. et al. Increased Risk of Hypertension in Young Adults in Southwest China: Impact of the 2017 ACC/AHA High Blood Pressure Guideline. Curr Hypertens Rep 21, 21 (2019). https://doi.org/10.1007/s11906-019-0926-y
Published:
DOI: https://doi.org/10.1007/s11906-019-0926-y