Abstract
There is increasing evidence that alterations in sleep continuity due to central nervous system arousal and/or reductions in deeper stages of sleep adversely affect blood pressure and contribute to hypertension. Disturbed sleep also blunts the normal nocturnal dip in blood pressure and may lead to sustained daytime hypertension as well. Nocturnal drops in blood pressure result from increased parasympathetic and reduced sympathetic activity during sleep. Slow-wave sleep, considered to be the most “restorative,” is the specific sleep state associated with the largest decline in sympathetic activity. The time in slow-wave sleep declines with age as well as in association with other health problems. A reduction in the time in slow-wave sleep has recently been reported to predict increased incident hypertension. The mechanisms by which this occurs have not been well described but may include alterations in dipping patterns, sympathetic nervous system activity, corticotrophin pathways, and the renin–angiotensin system. This article reviews the overall association between sleep and hypertension, with a specific focus on slow-wave sleep, a possible novel target for future blood pressure interventions.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA: The Journal of the American Medical Association. 2010;303:2043–50.
Wright JD, Hughes JP, Ostchega Y, Yoon SS, Nwankwo T. Mean systolic and diastolic blood pressure in adults aged 18 and over in the United States, 2001-2008. National Health Statistics Reports. 2011;1–22:24.
Kaplan, NM and Victor, R. Hypertension in the population at large. Clinical Hypertension (2010).
Logan AG, et al. High prevalence of unrecognized sleep apnoea in drug-resistant hypertension. J Hypertens. 2001;19:2271–7.
Pratt-Ubunama MN, et al. Plasma aldosterone is related to severity of obstructive sleep apnea in subjects with resistant hypertension. Chest. 2007;131:453–9.
Kato N, et al. Sleep-disordered breathing and hypertension in Japanese steel workers. Ind Heal. 2008;46:233–8.
Sulit L, Storfer-Isser A, Kirchner HL, Redline S. Differences in polysomnography predictors for hypertension and impaired glucose tolerance. Sleep. 2006;29:777–83.
Uchimura N. Hypertension and insomnia. Nihon Rinsho Japanese Journal of Clinical Medicine. 2011;69:2275–81.
Prejbisz A, et al. Characterization of insomnia in patients with essential hypertension. Blood pressure. 2006;15:213–9.
Kato M, et al. Effects of sleep deprivation on neural circulatory control. Hypertension. 2000;35:1173–5.
• Knutson KL, et al. Association between sleep and blood pressure in midlife: the CARDIA Sleep Study. Arch Intern Med. 2009;169:1055–61. This cross-sectional analysis of young adults revealed that reduced sleep duration and poorer sleep quality predicted elevated and adverse effects on BP.
Gottlieb DJ, et al. Association of usual sleep duration with hypertension: the Sleep Heart Health Study. Sleep. 2006;29:1009–14.
Javaheri S, Storfer-Isser A, Rosen CL, Redline S. Sleep quality and elevated blood pressure in adolescents. Circulation. 2008;118:1034–40.
Ogawa Y, et al. Total sleep deprivation elevates blood pressure through arterial baroreflex resetting: a study with microneurographic technique. Sleep. 2003;26:986–9.
Mullington, J.M., Haack, M., Toth, M., Serrador, J.M. & Meier-Ewert, H.K. Cardiovascular, inflammatory, and metabolic consequences of sleep deprivation. Progress in Cardiovascular Diseases 51, 294-302
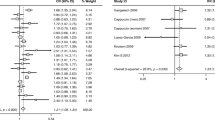
•• Fung MM, et al. Decreased slow wave sleep increases risk of developing hypertension in elderly men. Hypertension. 2011;58:596–603. This prospective analysis of over 700 subjects revealed that the amount of time spent in SWS was inversely related to the development of incident hypertension independently of sleep duration and sleep-disordered breathing.
Pressman M. Primer of Polysomnogram Interpretation. Boston: Butterworth-Heinemann; 2002.
Landolt HP, Borbély AA. Alcohol and sleep disorders. Therapeutische Umschau Revue Thérapeutique. 2000;57:241–5.
Redline S, et al. The effects of age, sex, ethnicity, and sleep-disordered breathing on sleep architecture. Arch Intern Med. 2004;164:406–18.
Landolt HP, Gillin JC. Sleep abnormalities during abstinence in alcohol-dependent patients. Aetiology and management. CNS Drugs. 2001;15:413–25.
Pillai V, Kalmbach DA, Ciesla JA. A meta-analysis of electroencephalographic sleep in depression: evidence for genetic biomarkers. Biol Psychiatry. 2011;70:912–9.
Dijk D-J. Slow-wave sleep deficiency and enhancement: implications for insomnia and its management. The World Journal of Biological Psychiatry: The Official Journal of the World Federation of Societies of Biological Psychiatry. 2010;11 Suppl 1:22–8.
Sarkar S, Katshu MZUH, Nizamie SH, Praharaj SK. Slow wave sleep deficits as a trait marker in patients with schizophrenia. Schizophr Res. 2010;124:127–33.
Kyung Lee E, Douglass AB. Sleep in psychiatric disorders: where are we now? Canadian Journal of Psychiatry. Revue Canadienne de Psychiatrie. 2010;55:403-–12.
Walsh JK. Enhancement of slow wave sleep: implications for insomnia. Journal of Clinical Sleep Medicine: JCSM: Official Publication of the American Academy of Sleep Medicine. 2009;5:S27–32.
Verdecchia P, Schillaci G, Porcellati C. Dippers versus non-dippers. Journal of Hypertension Supplement: Official Journal of the International Society of Hypertension. 1991;9:S42–4.
Staessen JA, et al. Nocturnal blood pressure fall on ambulatory monitoring in a large international database. The "Ad Hoc" Working Group. Hypertension. 1997;29:30–9.
Pickering TG. The clinical significance of diurnal blood pressure variations. Dippers and nondippers. Circulation. 1990;81:700–2.
• Minutolo R, et al. Prognostic role of ambulatory blood pressure measurement in patients with nondialysis chronic kidney disease. Arch Intern Med. 2011;171:1090–8. Ambulatory BP monitoring was compared with in-office BP monitoring in 436 patients with chronic kidney disease. In-office monitoring did not predict any outcomes, whereas ambulatory BP monitoring, particularly at night, predicted both renal and cardiovascular risk.
•• Ivanovic BA, Tadic MV, Celic VP. To dip or not to dip? The unique relationship between different blood pressure patterns and cardiac function and structure. J Hum Hypertens. 2011. doi:10.1038/jhh.2011.83. Hypertensive subjects underwent 24-h ambulatory BP monitoring and an echocardiogram in this cross-sectional analysis. Parameters of left ventricular and right ventricular diastolic function significantly and progressively worsened across the spectrum of dipping (extreme dippers, dippers, nondippers, and reverse dippers). Additionally, left ventricular and right ventricular structures were significantly more impaired in nondippers and reverse dippers than in the rest.
Cuspidi C, et al. Short-term reproducibility of a non-dipping pattern in type 2 diabetic hypertensive patients. J Hypertens. 2006;24:647–53.
Pierdomenico SD, et al. Arterial disease in dipper and nondipper hypertensive patients. Am J Hypertens. 1997;10:511–8.
Pierdomenico SD, et al. Blunted nocturnal fall in blood pressure and oxidative stress in men and women with essential hypertension. Am J Hypertens. 1999;12:356–63.
•• Verdecchia P, et al. Day-night dip and early-morning surge in blood pressure in hypertension: prognostic implications. Hypertension. 2012. doi:10.1161/HYPERTENSIONAHA.112.1918583763012. Subjects with initially untreated essential hypertension were followed for approximately 8 years with monitoring of BP dipping and early-morning BP surge. Analysis revealed that blunted overnight dipping was associated with a blunted morning BP surge, and that a blunted morning BP surge independently predicted cardiovascular events.
•• Li Y, et al. Prognostic value of the morning blood pressure surge in 5645 subjects from 8 populations. Hypertension. 2010;55:1040–8. This analysis of 5,645 subjects revealed that elevated morning BP surge is a significant and independent predictor of cardiovascular morbidity and mortality, suggesting that ambulatory BP monitoring may be a potentially useful modality for risk stratification.
Kario K, et al. Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: a prospective study. Circulation. 2003;107:1401–6.
Diekelmann S, Wilhelm I, Born J. The whats and whens of sleep-dependent memory consolidation. Sleep Medicine Reviews. 2009;13:309–21.
Rao MN, et al. Association between sleep architecture and measures of body composition. Sleep. 2009;32:483–90.
Tasali E, Leproult R, Ehrmann DA, Van Cauter E. Slow-wave sleep and the risk of type 2 diabetes in humans. Proc Natl Acad Sci U S A. 2008;105:1044–9.
Brooks D, Horner RL, Kozar LF, Render-Teixeira CL, Phillipson EA. Obstructive sleep apnea as a cause of systemic hypertension. Evidence from a canine model The Journal of Clinical Investigation. 1997;99:106–9.
•• Sayk F, et al. Effects of selective slow-wave sleep deprivation on nocturnal blood pressure dipping and daytime blood pressure regulation. Am J Physiol Regul Integr Comp Physiol. 2010;298:R191–7. Healthy subjects were selectively deprived of SWS for one night via acoustic stimulation and the effects were compared with those of one night of undisturbed sleep 1 week later. There was a significant reduction in BP dipping during the SWS suppression, but there was no significant difference in morning BP measurements, urine catecholamine measurements, or HR variability following each night.
Munakata M, et al. Involvement of the hypothalamo-pituitary-adrenal axis in the control of circadian blood pressure rhythm. Journal of Hypertension Supplement: Official Journal of the International Society of Hypertension. 1988;6:S44–6.
Opp MR. Rat strain differences suggest a role for corticotropin-releasing hormone in modulating sleep. Physiol Behav. 1997;63:67–74.
Chang FC, Opp MR. Blockade of corticotropin-releasing hormone receptors reduces spontaneous waking in the rat. Am J Physiol. 1998;275:R793–802.
Chang FC, Opp MR. IL-1 is a mediator of increases in slow-wave sleep induced by CRH receptor blockade. American Journal of Physiology. Regulatory. Integrative and Comparative Physiology. 2000;279:R793–802.
Krueger JM, et al. Involvement of cytokines in slow wave sleep. Progress in Brain Research. 2011;193:39–47.
Kapsimalis F, Richardson G, Opp MR, Kryger M. Cytokines and normal sleep. Current Opinion in Pulmonary Medicine. 2005;11:481–4.
Meijer JL, Ardesch HG, van Rooijen JC, de Bruijn JH. Low dose captopril twice daily lowers blood pressure without disturbance of the normal circadian rhythm. Postgraduate Medical Journal. 1986;62 Suppl 1:101–5.
Di Murro A, et al. Renin-angiotensin-aldosterone system in patients with sleep apnoea: prevalence of primary aldosteronism. Journal of the Renin-Angiotensin-Aldosterone System: JRAAS. 2010;11:165–72.
Van Someren EJW. Mechanisms and functions of coupling between sleep and temperature rhythms. Progress in Brain Research. 2006;153:309–24.
Karacan I, Thornby JI, Anch AM, Williams RL, Perkins HM. Effects of high ambient temperature on sleep in young men. Aviation, Space, and Environmental Medicine. 1978;49:855–60.
Raymann RJEM, Swaab DF, Van Someren EJW. Skin deep: enhanced sleep depth by cutaneous temperature manipulation. Brain: A Journal of Neurology. 2008;131:500–13.
Shapiro CM, Bortz R, Mitchell D, Bartel P, Jooste P. Slow-wave sleep: a recovery period after exercise. Science (New York, NY). 1981;214:1253–4.
Baekeland F, Lasky R. Exercise and sleep patterns in college athletes. Percept Mot Ski. 1966;23:1203–7.
Hanlon EC, Faraguna U, Vyazovskiy VV, Tononi G, Cirelli C. Effects of skilled training on sleep slow wave activity and cortical gene expression in the rat. Sleep. 2009;32:719–29.
Nihino S, M.E. Wake-promoting medications: basic mechanisms and pharmacology. Principles and Practices of Sleep Medicine 510 (2011).
O’Malley MB, Gleeson SK, W.I. Wake-promoting medications: efficacy and adverse effects. Principles and Practices of Sleep Medicine 527 (2011).
PK, S. Drugs that disturb sleep and wakefulness. Principles and Practices of Sleep Medicine 542 (2011).
W, M. Hypnotic medications: mechanisms of action and pharmacologic effects. Principles and Practices of Sleep Medicine 483 (2011).
DJ, B. Clinical pharmacology of other drugs used as hypnotics. Principles and Practices of Sleep Medicine 492 (2011).
Disclosure
S. Redline received research support from ResMed and Philips Respironics.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Javaheri, S., Redline, S. Sleep, Slow-Wave Sleep, and Blood Pressure. Curr Hypertens Rep 14, 442–448 (2012). https://doi.org/10.1007/s11906-012-0289-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11906-012-0289-0