ABSTRACT
BACKGROUND
Identifying factors associated with do-not-resuscitate (DNR) orders is an informative step in developing strategies to improve their use. As such, a descriptive analysis of the factors associated with the use of DNR orders in the early and late phases of hospitalizations for sepsis was performed.
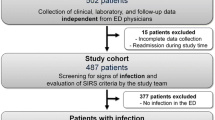
METHODS
A retrospective cohort of adult patients hospitalized for sepsis was identified using a statewide administrative database. DNR orders placed within 24 h of hospitalization (early DNR) and after 24 h of hospitalization (late DNR) were the primary outcome variables. Multivariable logistic regression analysis was used to identify patient, hospital, and healthcare system-related factors associated with the use of early and late DNR orders.
RESULTS
Among 77,329 patients hospitalized for sepsis, 27.5 % had a DNR order during their hospitalization. Among the cases with a DNR order, 75.5 % had the order within 24 h of hospitalization. Smaller hospital size and the absence of a teaching program increased the likelihood of an early DNR order being written. Additionally, greater patient age, female gender, White race, more medical comorbidities, Medicare payer status and admission from a skilled nursing facility were all significantly associated with the likelihood of having an early DNR. The strength of association between these factors and the use of late DNR orders was weaker. In contrast, the greater the burden of medical comorbidities, the more likely a patient was to receive a late DNR order.
CONCLUSION
Multiple patient, hospital, and healthcare system-related factors are associated with the use of DNR orders in sepsis, many of which appear to be independent of a patient’s clinical status. Over the course of the hospitalization, the burden of medical illness shows a stronger association relative to other variables. The influence of these multi-level factors needs to be recognized in strategies to improve the use of DNR orders. .

Similar content being viewed by others
REFERENCES
Angus DC, Linde-Zwirble WT, Lidicker J, et al. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29:1303–10.
Martin GS, Mannino DM, Eaton S, et al. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348:1546–54.
Hodgin KE, Moss M. The epidemiology of sepsis. Curr Pharm Des. 2008;14:1833–9.
Kleinpell R. New guidelines for sepsis care integrating palliative care and end of life care concepts. BMJ Support Palliat Care. 2012;2:194.
Burns JP, Edwards J, Johnson J, et al. Do-not-resuscitate order after 25 years. Crit Care Med. 2003;31:1543–50.
Hakim RB, Teno JM, Harrell FE Jr, et al. Factors associated with do-not-resuscitate orders: patients’ preferences, prognoses, and physicians’ judgments. SUPPORT Investigators. Study to understand prognoses and preferences for outcomes and risks of treatment. Ann Intern Med. 1996;125:284–93.
Shepardson LB, Gordon HS, Ibrahim SA, et al. Racial variation in the use of do-not-resuscitate orders. J Gen Intern Med. 1999;14:15–20.
Wenger NS, Pearson ML, Desmond KA, et al. Epidemiology of do-not-resuscitate orders. Disparity by age, diagnosis, gender, race, and functional impairment. Arch Intern Med. 1995;155:2056–62.
Zingmond DS, Wenger NS. Regional and institutional variation in the initiation of early do-not-resuscitate orders. Arch Intern Med. 2005;165:1705–12.
Office of Statewide Health Planning and Development. Patient Discharge Data, Public Set 2011 www.oshpd.ca.gov/HID/MIRCal/IPManual.html. 15 May 2014
Office of Statewide Health Planning and Development. Hospital Data / Financial. www.oshpd.ca.gov/HID/Dataflow/HospMain.html. 15 May 2014
Banta JE, Joshi KP, Beeson L, et al. Patient and hospital characteristics associated with inpatient severe sepsis mortality in California, 2005–2010. Crit Care Med. 2012;40:2960–6.
Iwashyna TJ, Odden A, Rohde J, et al. Identifying patients with severe sepsis using administrative claims: patient-level validation of the angus implementation of the international consensus conference definition of severe sepsis. Med Care. 2012;52:e39–43.
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–9.
Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
D’Hoore W, Bouckaert A, Tilquin C. Practical considerations on the use of the Charlson comorbidity index with administrative data bases. J Clin Epidemiol. 1996;49:1429–33.
Shepardson LB, Youngner SJ, Speroff T, et al. Variation in the use of do-not-resuscitate orders in patients with stroke. Arch Intern Med. 1997;157:1841–7.
Powell ES, Sauser K, Cheema N, et al. Severe sepsis in do-not-resuscitate patients: intervention and mortality rates. J Emerg Med. 2013;44:742–9.
Wenger NS, Pearson ML, Desmond KA, et al. Outcomes of patients with do-not-resuscitate orders: toward an understanding of what do-not-resuscitate orders mean and how they affect patients. Arch Intern Med. 1995;155:2063–8.
O’Brien J Jr, Aberegg S, Ali N, et al. Results from the national sepsis practice survey: predictions about mortality and morbidity and recommendations for limitation of care orders. Crit Care. 2009;13:1–11.
Barnato AE, Alexander SL, Linde-Zwirble WT, et al. Racial variation in the incidence, care, and outcomes of severe sepsis: analysis of population, patient, and hospital characteristics. Am J Respir Crit Care Med. 2008;177:279–84.
Barnato AE, Berhane Z, Weissfeld LA, et al. Racial variation in end-of-life intensive care use: a race or hospital effect? Health Serv Res. 2006;41:2219–37.
Soto GJ, Martin GS, Gong MN. Healthcare disparities in critical illness. Crit Care Med. 2013;41:2784–93.
Yergan J, Flood AB, LoGerfo JP, et al. Relationship between patient race and the intensity of hospital services. Med Care. 1987;25:592–603.
Contributions
Dr. Chang is the guarantor of the contents in the manuscript, including the data and analysis.
Dr. Chang: contributed to acquiring, analyzing, and interpreting the data and drafted the submitted article.
Dr. Brass: contributed to analyzing and interpreting the data; reviewed and revised the article critically for important intellectual content.
Other contributors: We thank Chi-hong Tseng, Ph.D. for his review of the statistical analysis and manuscript.
Funding / Support
The research described was supported by the National Institutes of Health (NIH)/National Center for Advancing Translational Science (NCATS) UCLA CTSI Grant Number UL1TR000124.
Prior Publication / Presentation
None.
Conflicts of Interest
Dr. Dong Chang has no conflicts of interest to report. Dr. Eric Brass is a consultant to numerous companies related to the development of drugs and medical devices. None of these companies or projects has a direct interest in the topic of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 124 kb)
Rights and permissions
About this article
Cite this article
Chang, D.W., Brass, E.P. Patient and Hospital-Level Characteristics Associated with the Use of Do-Not-Resuscitate Orders in Patients Hospitalized for Sepsis. J GEN INTERN MED 29, 1256–1262 (2014). https://doi.org/10.1007/s11606-014-2906-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-014-2906-x