Abstract
Background
Lymph node metastases are prognostically significant in pancreatic ductal adenocarcinoma. Little is known about the significance of direct lymph node invasion.
Aim
The aim of this study is to find out whether direct lymph node invasion has the same prognostic significance as regional nodal metastases.
Methods
Retrospective review of patients resected between 1/1/1993 and 7/31/2008. “Direct” was defined as tumor extension into adjacent nodes, and “regional” was defined as metastases to peripancreatic nodes.
Results
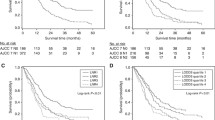
Overall, 517 patients underwent pancreatic resection for adenocarcinoma, of whom 89 had one positive node (direct 26, regional 63), and 79 had two positive nodes (direct 6, regional 68, both 5). Overall, survival of node-negative patients was improved compared to patients with positive nodes (N0 30.8 months vs. N1 16.4 months; p < 0.001). There was no survival difference for patients with direct vs. regional lymph node invasion (p = 0.67). Patients with one positive node had a better overall survival compared to patients with ≥2 positive nodes (22.3 and 15 months, respectively; p < 0.001). The lymph node ratio (+LN/total LN) was prognostically significant after Cox regression (p < 0.001).
Conclusions
Isolated direct invasion occurs in 20% of patients with one to two positive nodes. Node involvement by metastasis or by direct invasion are equally significant predictors of reduced survival. Both the number of positive nodes and the lymph node ratio are significant prognostic factors.





Similar content being viewed by others
References
American Cancer Society www.cancer.org.
Ferrone CR, Brennan MF, Gonen M et al. Pancreatic adenocarcinoma: the actual 5-year survivors. J Gastrointest Surg 2008;12(4):701–706.
Winter JM, Cameron JL, Campbell KA et al. 1423 pancreaticoduodenectomies for pancreatic cancer: a single-institution experience. J Gastrointest Surg 2006;10(9):1199–210. discussion 1210–1.
Schnelldorfer T, Ware AL, Sarr MG et al. Long-term survival after pancreatoduodenectomy for pancreatic adenocarcinoma: is cure possible? Ann Surg 2008;247(3):456–462.
Cleary SP, Gryfe R, Guindi M et al. Prognostic factors in resected pancreatic adenocarcinoma: analysis of actual 5-year survivors. J Am Coll Surg 2004;198(5):722–731.
House MG, Gonen M, Jarnagin WR et al. Prognostic significance of pathologic nodal status in patients with resected pancreatic cancer. J Gastrointest Surg 2007;11(11):1549–1555.
Lim JE, Chien MW, Earle CC. Prognostic factors following curative resection for pancreatic adenocarcinoma: a population-based, linked database analysis of 396 patients. Ann Surg 2003;237(1):74–85.
Ishikawa O, Ohigashi H, Sasaki Y et al. Practical grouping of positive lymph nodes in pancreatic head cancer treated by an extended pancreatectomy. Surgery 1997;121(3):244–249.
Pedrazzoli S, DiCarlo V, Dionigi R et al. Standard versus extended lymphadenectomy associated with pancreatoduodenectomy in the surgical treatment of adenocarcinoma of the head of the pancreas: a multicenter, prospective, randomized study. Lymphadenectomy Study Group. Ann Surg 1998;228(4):508–517.
Yeo CJ, Cameron JL, Lillemoe KD et al. Pancreaticoduodenectomy with or without distal gastrectomy and extended retroperitoneal lymphadenectomy for periampullary adenocarcinoma, part 2: randomized controlled trial evaluating survival, morbidity, and mortality. Ann Surg 2002;236(3):355–366. discussion 366–8.
Farnell MB, Pearson RK, Sarr MG et al. A prospective randomized trial comparing standard pancreatoduodenectomy with pancreatoduodenectomy with extended lymphadenectomy in resectable pancreatic head adenocarcinoma. Surgery 2005;138(4):618–628. discussion 628–30.
Schwarz RE, Smith DD. Extent of lymph node retrieval and pancreatic cancer survival: information from a large US population database. Ann Surg Oncol 2006;13(9):1189–1200.
Pawlik TM, Gleisner AL, Cameron JL et al. Prognostic relevance of lymph node ratio following pancreaticoduodenectomy for pancreatic cancer. Surgery 2007;141(5):610–618.
Tomlinson JS, Jain S, Bentrem DJ et al. Accuracy of staging node-negative pancreas cancer: a potential quality measure. Arch Surg 2007;142(8):767–723. discussion 773–4.
Hellan M, Sun CL, Artinyan A et al. The impact of lymph node number on survival in patients with lymph node-negative pancreatic cancer. Pancreas 2008;37(1):19–24.
Wilson M, Rosato EL, Chojnacki KA et al. Prognostic significance of lymph node metastases and ratio in esophageal cancer. J Surg Res 2008;146(1):11–15.
Inoue K, Nakane Y, Iiyama H et al. The superiority of ratio-based lymph node staging in gastric carcinoma. Ann Surg Oncol 2002;9(1):27–34.
Nitti D, Marchet A, Olivieri M et al. Ratio between metastatic and examined lymph nodes is an independent prognostic factor after D2 resection for gastric cancer: analysis of a large European monoinstitutional experience. Ann Surg Oncol 2003;10(9):1077–1085.
Le Voyer TE, Sigurdson ER, Hanlon AL et al. Colon cancer survival is associated with increasing number of lymph nodes analyzed: a secondary survey of intergroup trial INT-0089. J Clin Oncol 2003;21(15):2912–2919.
Berger AC, Watson JC, Ross EA, Hoffman JP. The metastatic/examined lymph node ratio is an important prognostic factor after pancreaticoduodenectomy for pancreatic adenocarcinoma. Am Surg 2004;70(3):235–240. discussion 240.
Smith RA, Bosonnet L, Ghaneh P et al. Preoperative CA19–9 levels and lymph node ratio are independent predictors of survival in patients with resected pancreatic ductal adenocarcinoma. Dig Surg 2008;25(3):226–232.
Acknowledgments
We would like to thank Hyacinth Haggarty and Ana Miranda from the Health Information Services and Carol Venuti from the Tumor Registry of the Massachusetts General Hospital for their precious help.
Author information
Authors and Affiliations
Corresponding author
Additional information
This research is being supported by the Andrew L. Warshaw, MD Institute for Pancreatic Cancer Research, Boston and by the Lantzounis research grant of the Hellenic Medical Society of New York.
Rights and permissions
About this article
Cite this article
Konstantinidis, I.T., Deshpande, V., Zheng, H. et al. Does the Mechanism of Lymph Node Invasion Affect Survival in Patients with Pancreatic Ductal Adenocarcinoma?. J Gastrointest Surg 14, 261–267 (2010). https://doi.org/10.1007/s11605-009-1096-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-009-1096-z