Abstract
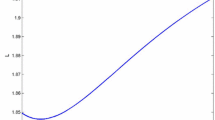
We study metastatic cancer progression through an extremely general individual-patient mathematical model that is rooted in the contemporary understanding of the underlying biomedical processes yet is essentially free of specific biological assumptions of mechanistic nature. The model accounts for primary tumor growth and resection, shedding of metastases off the primary tumor and their selection, dormancy and growth in a given secondary site. However, functional parameters descriptive of these processes are assumed to be essentially arbitrary. In spite of such generality, the model allows for computing the distribution of site-specific sizes of detectable metastases in closed form. Under the assumption of exponential growth of metastases before and after primary tumor resection, we showed that, regardless of other model parameters and for every set of site-specific volumes of detected metastases, the model-based likelihood-maximizing scenario is always the same: complete suppression of metastatic growth before primary tumor resection followed by an abrupt growth acceleration after surgery. This scenario is commonly observed in clinical practice and is supported by a wealth of experimental and clinical studies conducted over the last 110 years. Furthermore, several biological mechanisms have been identified that could bring about suppression of metastasis by the primary tumor and accelerated vascularization and growth of metastases after primary tumor resection. To the best of our knowledge, the methodology for uncovering general biomedical principles developed in this work is new.

Similar content being viewed by others
References
Alexander P (1983) Dormant metastases: studies in experimental animals. J Pathol 141:379–383
Balkwill F, Mantovani A (2001) Inflammation and cancer: back to Virchow? Lancet 357:539–545
Bashford E, Murray J, Cramer W (1907) The natural and induced resistance of mice to the growth of cancer. Proc R Soc Lond 79:164–187
Demicheli R, Retsky MW, Swartzendruber DE, Bonadonna G (1997) Proposal for a new model of breast cancer metastatic development. Ann Oncol 8:1075–1080
Demicheli R, Retsky M, Hrushesky WJM, Baum M, Gukas ID (2008) The effects of surgery on tumor growth: a century of investigations. Ann Oncol 19:1821–1828
DeWys WD (1972) Studies correlating the growth rate of a tumor and its metastases and providing evidence for tumor-related systemic growth-retarding factors. Cancer Res 32:374–379
Ehrlich P (1906) Experimentelle Karzinomstudien an Mäusen. Arch Koiglichen Inst Exp Ther Frankfurt am Main 1:65–103 (in German)
Fakir H, Hlatky L, Li H, Sachs R (2013) Repopulation of interacting tumor cells during fractionated radiotherapy: stochastic modeling of the tumor control probability. Med Phys 40(12):121716
Fidler IA (1990) Critical factors in the biology of human cancer metastasis: twenty-eighth G. H. A. Clowes memorial award lecture. Cancer Res 50:6130–6138
Fisher B (1999) From Halsted to prevention and beyond: advances in the management of breast cancer during the twentieth century. Eur J Cancer 35:1963–1973
Folkman J (1974) Tumor angiogenesis factor. Cancer Res 34:2109–2113
Folkman J (2002) Role of angiogenesis in tumor growth and metastasis. Semin Oncol 29(6), Suppl 16:15–18
Forget P, Vandenhende J, Berliere M, Machiels JP, Nussbaum B, Legrand C, DeKock M (2010) Do intraoperative analgesics influence breast cancer recurrence after mastectomy? A retrospective analysis. Anesth Analg 110(6):1630–1635
Gorelik E (1983) Concomitant tumor immunity and resistance to a second tumor challenge. Adv Cancer Res 39:71–120
Hadfield G (1954) The dormant cancer cell. Br Med J 2:607–610
Hanin LG (2008) Distribution of the sizes of metastases: mathematical and biomedical considerations. In: Tan WY, Hanin LG (eds) Handbook of cancer models with applications. World Scientific, Singapore, pp 141–169
Hanin LG (2013) Seeing the invisible: how mathematical models uncover tumor dormancy, reconstruct the natural history of cancer and assess the effects of treatment. In: Almog N, Enderling H, Hlatky L (eds) Systems biology of tumor dormancy. Advances in experimental medicine and biology, vol 734. Springer, New York, pp 261–282
Hanin L (2017) Do breast cancer patients benefit from surgery? Hypotheses, mathematical models and false beliefs. In: Retsky M, Demicheli R (eds) Perioperative inflammation as a triggering origin of metastasis development. Springer, New York, pp 161–182
Hanin LG, Yakovlev AY (1996) A nonidentifiability aspect of the two-stage model of carcinogenesis. Risk Anal 16:711–715
Hanin LG, Korosteleva O (2010) Does extirpation of the primary breast tumor give boost to growth of metastases? Evidence revealed by mathematical modeling. Math Biosci 223:133–141
Hanin L, Zaider M (2011) Effects of surgery and chemotherapy on metastatic progression of prostate cancer: evidence from the natural history of the disease reconstructed through mathematical modeling. Cancers 3:3632–3660
Hanin LG, Bunimovich-Mendrazitsky S (2014) Reconstruction of the natural history of metastatic cancer and assessment of the effects of surgery: gompertzian growth of the primary tumor. Math Biosci 247:47–58
Hanin L, Pavlova L (2016) A quantitative insight into metastatic relapse of breast cancer. J Theor Biol 394:172–181
Hanin L, Rose J (2016) Uncovering the natural history of cancer from post mortem cross-sectional diameters of hepatic metastases. Math Med Biol 33(4):397–416
Hanin LG, Rose J, Zaider M (2006) A stochastic model for the sizes of detectable metastases. J Theor Biol 243:407–417
Hanin L, Seidel K, Stoevesandt D (2016) A “universal” model of metastatic cancer, its parametric forms and their identification: what can be learned from site-specific volumes of metastases. J Math Biol 72(6):1633–1662
Hiller J, Schier R, Riedel B (2017) Perioperative biologic perturbation and cancer surgery: targeting the adrenergic-inflammatory response and microcirculatory dysregulation. In: Retsky M, Demicheli R (eds) Perioperative inflammation as a triggering origin of metastasis development. Springer, New York, pp 83–107
Holmgren K, O’Reilly MS, Folkman J (1995) Dormancy of micrometastases: balanced proliferation and apoptosis in the presence of angiogenesis suppression. Nat Med 1:149–153
Hölzel D, Eckel R, Emeny RT, Engel J (2010) Distant metastases do not metastasize. Cancer Metastasis Rev 29:737–750
Karr AF (1993) Probability. Springer, New York
Kendal WS (2006) Chance mechanisms affecting the burden of metastases. BMC Cancer 5:138
Kleffel S, Schatton T (2013) Tumor dormancy and cancer stem cells: two sides of the same coin? In: Almog N, Enderling H, Hlatky L (eds) Systems biology of tumor dormancy. Advances in experimental medicine and biology, vol 734. Springer, New York, pp 145–179
Maida V, Ennis M, Kuziemsky C, Corban J (2009) Wounds and survival in cancer patients. Eur J Cancer 45:3237–3244
Marches R, Scheuermann R, Uhr J (2006) Cancer dormancy-from mice to man. Cell Cycle 5(16):1772–1778
Prehn RT (1993) Two competing influences that may explain concomitant tumor resistance. Cancer Res 53:3266–3269
Retsky M, Demicheli R (2017) Perioperative inflammation as a triggering origin of metastasis development. In: Retsky M, Demicheli R (eds) Perioperative inflammation as a triggering origin of metastasis development. Springer, New York, pp 19–54
Retsky M, Demicheli R, Hrushesky W, Baum M, Gukas I (2010) Surgery triggers outgrowth of latent distant disease in breast cancer: an inconvenient truth? Cancers 2:305–337
Retsky M, Demicheli R, Hrushesky WJM, Forget P, DeKock M, Gukas I, Rogers RA, Baum M, Sukhatme V, Vaidya JS (2013) Reduction of breast cancer relapses with perioperative non-steroidal anti-inflammatory drugs: new findings and a review. Curr Med Chem 20(33):4163–4176
Ross SM (1997) Introduction to probability models, 6th edn. Academic Press, San Diego
Spano D, Heck C, De Antonelli P, Christofori G, Zollo M (2012) Molecular networks that regulate cancer metastasis. Semin Cancer Biol 22(3):234–49
Stigler SM (2007) The epic story of maximum likelihood. Stat Sci 22(4):598–620
Sugarbaker EV, Ketcham AS, Cohen AM (1971) Studies of dormant tumor cells. Cancer 28:545–552
Sugarbaker E, Thornswaite J, Ketcham A (1977) Inhibitory effect of a primary tumor on metastasis. In: Day S, Myers W, Stansly P, Garattini S, Lewis M (eds) Progress in cancer research and therapy, vol 5. Raven Press, New York, pp 227–240
Tyzzer EE (1913) Factors in the production and growth of tumor metastases. J Med Res 28:309–332
Vatner RE, Cooper BT, Vanpouille-Box C, Demaria S, Formenti SC (2014) Combinations of immunotherapy and radiation in cancer therapy. Front Oncol 4:325
Acknowledgements
Incisive and constructive comments by the two anonymous reviewers have helped the authors to considerably improve the manuscript. The reviewers’ suggestions are greatly appreciated.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hanin, L., Rose, J. Suppression of Metastasis by Primary Tumor and Acceleration of Metastasis Following Primary Tumor Resection: A Natural Law?. Bull Math Biol 80, 519–539 (2018). https://doi.org/10.1007/s11538-017-0388-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11538-017-0388-9