Abstract
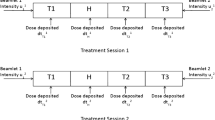
The main steps in planning radiotherapy consist in selecting for any patient diagnosed with a solid tumor (i) a prescribed radiation dose on the tumor, (ii) bounds on the radiation side effects on nearby organs at risk and (iii) a fractionation scheme specifying the number and frequency of therapeutic sessions during treatment. The goal of any radiotherapy treatment is to deliver on the tumor a radiation dose as close as possible to that selected in (i), while at the same time conforming to the constraints prescribed in (ii). To this day, considerable uncertainties remain concerning the best manner in which such issues should be addressed. In particular, the choice of a prescription radiation dose is mostly based on clinical experience accumulated on the particular type of tumor considered, without any direct reference to quantitative radiobiological assessment. Interestingly, mathematical models for the effect of radiation on biological matter have existed for quite some time, and are widely acknowledged by clinicians. However, the difficulty to obtain accurate in vivo measurements of the radiobiological parameters involved has severely restricted their direct application in current clinical practice.
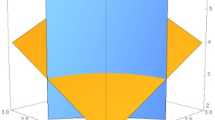
In this work, we first propose a mathematical model to select radiation dose distributions as solutions (minimizers) of suitable variational problems, under the assumption that key radiobiological parameters for tumors and organs at risk involved are known. Second, by analyzing the dependence of such solutions on the parameters involved, we then discuss the manner in which the use of those minimizers can improve current decision-making processes to select clinical dosimetries when (as is generally the case) only partial information on model radiosensitivity parameters is available. A comparison of the proposed radiation dose distributions with those actually delivered in a number of clinical cases strongly suggests that solutions of our mathematical model can be instrumental in deriving good quality tests to select radiotherapy treatment plans in rather general situations.








Similar content being viewed by others
Abbreviations
- PTV :
-
Planning Target Volume
- OAR :
-
Organ at Risk
- HT :
-
Healthy Tissue
- Dp :
-
Prescribed Radiation Dose on the PTV
- LQ :
-
Linear Quadratic Model
- Gy :
-
grays (1 Gy is 1 joule per kilogram)
- BED :
-
Biological Effective Dose
- ER :
-
Early-Responding Tissue
- LR :
-
Late-Responding Tissue
- TPS :
-
Treatment Planning System
- HI :
-
Homogeneity Index
- CI :
-
Conformity Index
- LINAC :
-
Linear Particle Accelerator
- DVH :
-
Dose–Volume Histogram
References
Akpati, H., Kim, C., Kim, B., Park, T., & Meek, A. (2008). Unified dosimetry index (UDI): a figure of merit for ranking treatment plans. J. Appl. Clin. Med. Phys., 9(3), 2803. doi:10.1120/jacmp.v9i3.2803.
Alfonso, J. C. L., Buttazzo, G., García-Archilla, B., Herrero, M. A., & Núñez, L. (2012). A class of optimization problems in radiotherapy dosimetry planning. Discrete Contin. Dyn. Syst., Ser. B, 17(6), 1651–1672. doi:10.3934/dcdsb.2012.17.1651.
Andasari, V., Gerisch, A., Lolas, G., South, A. P., & Chaplain, M. A. (2011). Mathematical modeling of cancer cell invasion of tissue: biological insight from mathematical analysis and computational simulation. J. Math. Biol., 63(1), 141–171. doi:10.1007/s00285-010-0369-1.
Araujo, R. P., & McElwain, D. L. (2004). A history of the study of solid tumour growth: the contribution of mathematical modelling. Bull. Math. Biol., 66(5), 1039–1091. doi:10.1016/j.bulm.2003.11.002.
Bao, S., Wu, Q., McLendon, R. E., Hao, Y., Shi, Q., Hjelmeland, A. B., Dewhirst, M. W., Bigner, D. D., & Rich, J. N. (2006). Glioma stem cells promote radioresistance by preferential activation of the DNA damage response. Nature, 444(7120), 756–760. doi:10.1038/nature05236.
Barendsen, G. W. (1982). Dose fractionation, dose rate and iso-effect relationships for normal tissue responses. Int. J. Radiat. Oncol. Biol. Phys., 8(11), 1981–1997. doi:10.1016/0360-3016(82)90459-X.
Bellomo, N., Bellouquid, A., & Delitala, M. (2004). Mathematical topics on the modelling complex multicellular systems and tumor immune cells competition. Math. Models Methods Appl. Sci., 14(11), 1683–1733.
Bertuzzi, A., Fasano, A., Gandolfi, A., & Sinisgalli, C. (2008). Reoxygenation and split-dose response to radiation in a tumour model with Krogh-type vascular geometry. Bull. Math. Biol., 70(4), 992–1012. doi:10.1007/s11538-007-9287-9.
Bertuzzi, A., Bruni, C., Fasano, A., Gandolfi, A., Papa, F., & Sinisgalli, C. (2010). Response of tumor spheroids to radiation: modeling and parameter estimation. Bull. Math. Biol., 72(5), 1069–1091. doi:10.1007/s11538-009-9482-y.
Boissonnat, J. D., Devillers, O., Pion, S., Teillaud, M., & Yvinec, M. (2002). Triangulations in CGAL. Comput. Geom. Theory Appl., 22, 5–19. doi:10.1016/S0925-7721(01)00054-2.
Brenner, D. J., Hlatky, L. R., Hahnfeldt, P. J., Huang, Y., & Sachs, R. K. (1998). The linear-quadratic model and most other common radiobiological models result in similar predictions of time-dose relationships. Radiat. Res., 150, 83–91. doi:10.2307/3579648.
Brezis, H. (2010). Functional analysis, Sobolev spaces and partial differential equations. Berlin: Springer.
Buttazzo, G. (1989). Semicontinuity, relaxation and integral representation in the calculus of variations. Harlow: Longman Scientific & Technical.
Buttazzo, G., Giaquinta, M., & Hildebrandt, S. (1998). One-dimensional calculus of variations: an introduction. Oxford: Oxford University Press.
Byrne, H., & Preziosi, L. (2003). Modelling solid tumour growth using the theory of mixtures. Math. Med. Biol., 20(4), 341–366. doi:10.1093/imammb/20.4.341.
Byrne, H. M., Alarcón, T., Owen, M. R., Webb, S. D., & Maini, P. K. (2006). Modelling aspects of cancer dynamics: a review. Philos. Trans. A Math. Phys. Eng. Sci., 364(1843), 1563–1578.
Cappuccio, A., Herrero, M. A., & Núñez, L. (2009). Tumour radiotherapy and its mathematical modelling. Contemp. Math., 492, 77–102.
Cappuccio, A., Herrero, M. A., & Núñez, L. (2009). Biological optimization of tumor radiosurgery. Med. Phys., 36(1), 98–104.
Carlson, D. J., Stewart, R. D., Li, X. A., Jennings, K., Wang, J. Z., & Guerrero, M. (2004). Comparison of in vitro and in vivo α/β ratios for prostate cancer. Phys. Med. Biol., 49, 4477–4491. doi:10.1088/0031-9155/49/19/003.
CGAL Computational Geometry Algorithms Library. http://www.cgal.org.
Chao, M., Xie, Y., Moros, E. G., Le, Q. T., & Xing, L. (2010). Image-based modeling of tumor shrinkage in head and neck radiation therapy. Med. Phys., 37(5), 2351–2358. doi:10.1118/1.3399872.
Ciarlet, P. G. (1978). The finite element method for elliptic problems. Philadelphia: SIAM. Reprint of the original, 2002.
Dale, R., & Jones, B. (2007). Radiobiological modelling in radiation oncology. The British Institute of Radiology, London, UK.
de Berg, M., Cheong, O., van Kreveld, M., & Overmars, M. (2008). Computational geometry: algorithms and applications (3rd ed.). Santa Clara: Springer.
Deasy, J. O., Blanco, A. I., & Clark, V. H. (2003). CERR: a computational environment for radiotherapy research. Med. Phys., 30(5), 979–985. doi:10.1118/1.1568978.
Debus, J., Wuendrich, M., Pirzkall, A., Hoess, A., Schlegel, W., Zuna, I., Engenhart-Cabillic, R., & Wannenmacher, M. (2001). High efficacy of fractionated stereotactic radiotherapy of large base-of-skull meningiomas: long-term results. J. Clin. Oncol., 19(15), 3547–3553.
Dionysiou, D. D., Stamatakos, G. S., Gintides, D., Uzunoglu, N., & Kyriaki, K. (2008). Critical parameters determining standard radiotherapy treatment outcome for glioblastoma multiforme: a computer simulation. Open Biomed. Eng. J., 2, 43–51. doi:10.2174/1874120700802010043.
Enderling, H., Park, D., Hlatky, L., & Hahnfeldt, P. (2009). The importance of spatial distribution of stemness and proliferation state in determining tumor radioresponse. Math. Model. Nat. Phenom., 4(3), 117–133. doi:10.1051/mmnp/20094305.
Enderling, H., Chaplain, M. A., & Hahnfeldt, P. (2010). Quantitative modeling of tumor dynamics and radiotherapy. Acta Biotheor., 58(4), 341–353. doi:10.1007/s10441-010-9111-z.
Feuvret, L., Noël, G., Mazeron, J. J., & Bey, P. (2006). Conformity index: a review. Int. J. Radiat. Oncol. Biol. Phys., 64(2), 333–342. doi:10.1016/j.ijrobp.2005.09.028.
Fowler, J. F. (1989). The linear-quadratic formula and progress in fractionated radiotherapy. Br. J. Radiol., 62(740), 679–694.
Gao, X., McDonald, J. T., Hlatky, L., & Enderling, H. (2013). Acute and fractionated irradiation differentially modulate glioma stem cell division kinetics. Cancer Res., 73(5), 1481–1490. doi:10.1158/0008-5472.CAN-12-3429.
Grimm, J., LaCouture, T., Croce, R., Yeo, I., Zhu, Y., & Xue, J. (2011). Dose tolerance limits and dose volume histogram evaluation for stereotactic body radiotherapy. J. Appl. Clin. Med. Phys., 12(2), 3368.
Hall, E. J., & Giaccia, A. J. (2006). Radiobiology for the radiologist. Baltimore: Lippincott Williams & Wilkins.
International Commission on Radiation Units and Measurements (1980). Radiation quantities and units. ICRU report 33. Washington DC, USA.
International Commission on Radiation Units and Measurements (2010). Prescribing, recording, and reporting IMRT. ICRU Report 83. Washington DC, USA.
Johnson, C. (2009). Numerical solution of partial differential equations by the finite element method. Mineola: Dover Reprint of the 1987 edition.
Jones, B., Dale, R. G., Deehan, C., Hopkins, K. I., & Morgan, D. A. (2001). The role of biologically effective dose (BED) in clinical oncology. Clin. Oncol. (R. Coll. Radiol.), 13(2), 71–81.
Kehwar, T. S. (2005). Analytical approach to estimate normal tissue complication probability using best fit of normal tissue tolerance doses into the NTCP equation of the linear quadratic model. J. Cancer Res. Ther., 1(3), 168–179. doi:10.4103/0973-1482.19597.
Kempf, H., Bleicher, M., & Meyer-Hermann, M. (2010). Spatio-temporal cell dynamics in tumour spheroid irradiation. Eur. Phys. J. D, 60(1), 177–193. doi:10.1140/epjd/e2010-00178-4.
Knöös, T., Kristensen, I., & Nilsson, P. (1998). Volumetric and dosimetric evaluation of radiation treatment plans: radiation conformity index. Int. J. Radiat. Oncol. Biol. Phys., 42(5), 1169–1176. doi:10.1016/S0360-3016(98)00239-9.
Law, M. Y., & Liu, B. (2009). Informatics in radiology: DICOM-RT and its utilization in radiation therapy. Radiographics, 29(3), 655–667. doi:10.1148/rg.293075172.
Lomax, N. J., & Scheib, S. G. (2003). Quantifying the degree of conformity in radiosurgery treatment planning. Int. J. Radiat. Oncol. Biol. Phys., 55(5), 1409–1419. doi:10.1016/S0360-3016(02)04599-6.
Macklin, P., McDougall, S., Anderson, A. R., Chaplain, M. A., Cristini, V., & Lowengrub, J. (2009). Multiscale modelling and nonlinear simulation of vascular tumour growth. J. Math. Biol., 58(4–5), 765–798. doi:10.1007/s00285-008-0216-9.
Martin, N. K., Gaffney, E. A., Gatenby, R. A., & Maini, P. K. (2010). Tumour-stromal interactions in acid-mediated invasion: a mathematical model. J. Theor. Biol., 267(3), 461–470. doi:10.1016/j.jtbi.2010.08.028.
Marusyk, A., Almendro, V., & Polyak, K. (2012). Intra-tumour heterogeneity: a looking glass for cancer? Nat. Rev. Cancer, 12(5), 323–334. doi:10.1038/nrc3261.
Mayles, P., Nahum, A., & Rosenwald, J. C. (2007). Handbook of radiotherapy physics: theory and practice. London: Taylor & Francis.
McAneney, H., & O’Rourke, S. F. (2007). Investigation of various growth mechanisms of solid tumour growth within the linear-quadratic model for radiotherapy. Phys. Med. Biol., 52(4), 1039–1054. doi:10.1088/0031-9155/52/4/012.
Menhel, J., Levin, D., Alezra, D., Symon, Z., & Pfeffer, R. (2006). Assessing the quality of conformal treatment planning: a new tool for quantitative comparison. Phys. Med. Biol., 51(20), 5363–5375. doi:10.1088/0031-9155/51/20/019.
Meyer, R. R., Zhang, H. H., Goadrich, L., Nazareth, D. P., Shi, L., & D’Souza, W. D. (2007). A multiplan treatment-planning framework: a paradigm shift for intensity-modulated radiotherapy. Int. J. Radiat. Oncol. Biol. Phys., 68(4), 1178–1189. doi:10.1016/j.ijrobp.2007.02.051.
Minniti, G., Amichetti, M., & Enrici, R. M. (2009). Radiotherapy and radiosurgery for benign skull base meningiomas. Radiat. Oncol., 4, 42. doi:10.1186/1748-717X-4-42.
Nocedal, J., & Wright, S. J. (2006). Numerical optimization (2nd ed.). New York: Springer.
Olive, P. L. (1998). The role of DNA single- and double-strand breaks in cell killing by ionizing radiation. Radiat. Res., 150(Suppl. 5), S42–S51.
O’Rourke, S. F., McAneney, H., & Hillen, T. (2009). Linear quadratic and tumour control probability modelling in external beam radiotherapy. J. Math. Biol., 58(4–5), 799–817. doi:10.1007/s00285-008-0222-y.
Paddick, I. (2000). A simple scoring ratio to index the conformity of radiosurgical treatment plans. J. Neurosurg., 93(Suppl. 3), 219–222.
Palta, J. R., & Mackie, T. R. (2003). Intensity-modulated radiation therapy—the state of the art,. Madison: Medical Physics Publishing.
Perfahl, H., Byrne, H. M., Chen, T., Estrella, V., Alarcón, T., Lapin, A., Gatenby, R. A., Gillies, R. J., Lloyd, M. C., Maini, P. K., Reuss, M., & Owen, M. R. (2011). Multiscale modelling of vascular tumour growth in 3D: the roles of domain size and boundary conditions. PLoS ONE, 6(4), e14790. doi:10.1371/journal.pone.0014790.
Ramis-Conde, I., Chaplain, M. A., Anderson, A. R., & Drasdo, D. (2009). Multi-scale modelling of cancer cell intravasation: the role of cadherins in metastasis. Phys. Biol., 6(1), 016008. doi:10.1088/1478-3975/6/1/016008.
Rockne, R., Alvord, E. C. Jr., Rockhill, J. K., & Swanson, K. R. (2009). A mathematical model for brain tumor response to radiation therapy. J. Math. Biol., 58(4–5), 561–578. doi:10.1007/s00285-008-0219-6.
Rockne, R., Rockhill, J. K., Mrugala, M., Spence, A. M., Kalet, I., Hendrickson, K., Lai, A., Cloughesy, T., Alvord, E. C. Jr., & Swanson, K. R. (2010). Predicting the efficacy of radiotherapy in individual glioblastoma patients in vivo: a mathematical modeling approach. Phys. Med. Biol., 55(12), 3271–3285. doi:10.1088/0031-9155/55/12/001.
Schaller, G., & Meyer-Hermann, M. (2006). Continuum versus discrete model: a comparison for multicellular tumour spheroids. Philos. Trans. A Math. Phys. Eng. Sci., 364, 1443–1464. 1843. doi:10.1098/rsta.2006.1780.
Schenk, O., Wächter, A., & Hagemann, M. (2007). Matching-based preprocessing algorithms to the solution of saddle-point problems in large-scale nonconvex interior-point optimization. Comput. Optim. Appl., 36(2–3), 321–341. doi:10.1007/s10589-006-9003-y.
Schenk, O., Bollhöfer, M., & Römer, R. A. (2008). On large-scale diagonalization techniques for the Anderson model of localization. SIAM J. Sci. Comput., 28(3), 963–983. doi:10.1137/050637649.
Schwarz, H. R. (1988). Finite element methods. London: Academic Press.
Shaw, E., Kline, R., Gillin, M., Souhami, L., Hirschfeld, A., Dinapoli, R., & Martin, L. (1993). Radiation therapy oncology group: radiosurgery quality assurance guidelines. Int. J. Radiat. Oncol. Biol. Phys., 27(5), 1231–1239. doi:10.1016/0360-3016(93)90548-A.
Shepard, D. M., Ferris, M. C., Olivera, G. H., & Mackie, T. R. (1999). Optimizing the delivery of radiation therapy to cancer patients. SIAM Rev., 41(4), 721–744. doi:10.1137/S0036144598342032.
Shrieve, D. C., Hazard, L., Boucher, K., & Jensen, R. L. (2004). Dose fractionation in stereotactic radiotherapy for parasellar meningiomas: radiobiological considerations of efficacy and optic nerve tolerance. J. Neurosurg., 101(Suppl. 3), 390–395.
Thames, H. D., Bentzen, S. M., Turesson, I., Overgaard, M., & Van den Bogaert, W. (1990). Time-dose factors in radiotherapy: a review of the human data. Radiother. Oncol., 19(3), 219–235. doi:10.1016/0167-8140(90)90149-Q.
Thariat, J., Hannoun-Levi, J. M., Sun Myint, A., Vuong, T., & Gérard, J. P. (2013). Past, present, and future of radiotherapy for the benefit of patients. Nat. Rev. Clin. Oncol., 10(1), 52–60. doi:10.1038/nrclinonc.2012.203.
Vernimmen, F. J., & Slabbert, J. P. (2010). Assessment of the alpha/beta ratios for arteriovenous malformations, meningiomas, acoustic neuromas, and the optic chiasma. Int. J. Radiat. Biol., 86(6), 486–498. doi:10.3109/09553001003667982.
Wachter, A., & Biegler, L. T. (2006). On the implementation of a primal–dual interior point filter line search algorithm for large-scale nonlinear programming. Math. Program., 106(1), 25–57. doi:10.1007/s10107-004-0559-y.
Wagner, T. H., Bova, F. J., Friedman, W. A., Buatti, J. M., Bouchet, L. G., & Meeks, S. L. (2003). A simple and reliable index for scoring rival stereotactic radiosurgery plans. Int. J. Radiat. Oncol. Biol. Phys., 57(4), 1141–1149. doi:10.1016/S0360-3016(03)01563-3.
Williams, M. V., Denekamp, J., & Fowler, J. F. (1985). A review of alpha/beta ratios for experimental tumors: implications for clinical studies of altered fractionation. Int. J. Radiat. Oncol. Biol. Phys., 11(1), 87–96. doi:10.1016/0360-3016(85)90366-9.
Wu, Q. R., Wessels, B. W., Einstein, D. B., Maciunas, R. J., Kim, E. Y., & Kinsella, T. J. (2003). Quality of coverage: conformity measures for stereotactic radiosurgery. J. Appl. Clin. Med. Phys., 4(4), 374–381.
Wu, V. W., Kwong, D. L., & Sham, J. S. (2004). Target dose conformity in 3-dimensional conformal radiotherapy and intensity modulated radiotherapy. Radiother. Oncol., 71(2), 201–206. doi:10.1016/j.radonc.2004.03.004.
Yoon, M., Park, S. Y., Shin, D., Lee, S. B., Pyo, H. R., Kim, D. Y., & Cho, K. H. (2007). A new homogeneity index based on statistical analysis of the dose-volume histogram. J. Appl. Clin. Med. Phys., 8(2), 9–17. doi:10.1120/jacmp.v8i2.2390.
Zienkiewicz, O. C., & Taylor, R. L. (1989). The finite element method. London: McGraw-Hill.
Acknowledgements
J.C.L. Alfonso gratefully acknowledges a Ph.D. fellowship funded by MINECO (Spain). J.C.L. Alfonso, M.A. Herrero and L. Núñez have been partially supported by Spanish MINECO Grant MTM 2011-22656. B. García-Archilla was partially supported by MINECO Grant 2009-07849.
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Appendix
Appendix
We provide here the main ingredients in the proofs of Theorems 2.1 and 2.2 in Sect. 2.
Proof of Theorem 2.1
It is readily seen that the functional given in (7) is lower semicontinuous (l.s.c.) on the space W 1,∞(Ω) endowed with the uniform convergence. Existence of at least one minimizer follows from the fact that the associated functional
where K is as in the statement of part (a) in the Theorem 2.1 and I K (D)=0 when D∈K,I K (D)=+∞ otherwise, is also l.s.c. on W 1,∞(Ω) with respect to the uniform convergence, since K is compact for that convergence. Then a minimizer of (17) (hence for the problem under consideration consisting of minimizing (7) under constraints (8)–(10)) exists by classical results (cf. Buttazzo 1989, Buttazzo et al. 1998).
On the other hand, a direct computation (similar to that performed in Alfonso et al. (2012) for a related problem) shows that the integrand in (7) is convex when inequalities (11) and (12) are satisfied. This in turn implies the convexity of J(D) in (7), whereupon uniqueness follows. □
Proof of Theorem 2.2
It is quite similar to that of Theorem 2.1. In particular, the functional
is l.s.c. on the space W 1,∞(Ω) endowed with the uniform convergence, since \(\overline{K}\) is compact for that convergence. This yields the existence of minimizers of (18), and hence for the problem under consideration consisting of minimizing (7) under constraints (8)–(10) and (13), (14). In its turn, uniqueness follows exactly as in Theorem 2.1. □
Rights and permissions
About this article
Cite this article
Alfonso, J.C.L., Buttazzo, G., García-Archilla, B. et al. Selecting Radiotherapy Dose Distributions by Means of Constrained Optimization Problems. Bull Math Biol 76, 1017–1044 (2014). https://doi.org/10.1007/s11538-014-9945-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11538-014-9945-7