Abstract
Purpose
This study aimed to ascertain the general characteristics of injured patients and use the Andersen Model to identify factors affecting health-related quality of life (QOL) in injured patients with or without activity limitations.
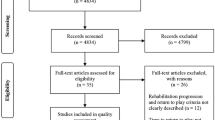
Methods
We used data of 1602 injured patients from 2014 to 2017 from the population-based Korea National Health and Nutrition Examination Survey, South Korea. QOL was measured using the EQ-5D-3L, and activity limitations were analyzed alongside predisposing factors (gender, age, education level, and marital status), enabling factors (basic living security, health insurance type, private insurance status, household income, and living with family), need factors (number of chronic diseases, subjective health status, and unmet medical needs), and health behaviors (smoking status, alcohol consumption, physical activity, and health screening). Data were analyzed using homogeneity testing, t tests, and logistic and multiple regression.
Results
The mean EQ-5D index was 0.8 with activity limitations and 0.9 without activity limitations. In mobility domain, patients without activity limitations showed significant effects of age, education level, number of chronic diseases, subjective health status, and unmet medical needs on mobility, whereas patients with activity limitations only showed a significant effect of age. In self-care domain, age, household income, and number of chronic diseases showed significant factors on patients without activity limitations, but there was no significant factor associated with activity limitations. Among the factors affecting usual activities, gender was found to have a significant effect only on patients with activity limitations, and subjective health status was found to have a significant effect regardless of activity limitations. Among the factors affecting pain/discomfort, living with family only affected pain/discomfort in patients with activity limitations. Among the factors affecting anxiety/depression, gender and alcohol consumption had significant effects only on patients with activity limitations.
Conclusion
Factors affecting the QOL of injured patients differed depending on whether patients had activity limitations. Therefore, when assessing injured patients, it may be necessary to ascertain the extent of activity limitations, and medical institutions and local communities need when implementing education and interventions to improve their QOL.
Similar content being viewed by others
References
World Health Organization. (2008). The global burden of disease: 2004 update. Geneva: World Health Organization.
Roth, T., Coulouvrat, C., Hajak, G., Lakoma, M. D., Sampson, N. A., Shahly, V., et al. (2011). Prevalence and perceived health associated with insomnia based on DSM-IV-TR; international statistical classification of diseases and related health problems, tenth revision; and research diagnostic criteria/international classification of sleep disorders, criteria: results from the America insomnia survey. Biological Psychiatry. https://doi.org/10.1016/j.biopsych.2010.10.023.
Statistics Korea (2019). 2018 cause of death statistics. Statistics Korea. http://kostat.go.kr/portal/eng/pressReleases/1/index.board?bmode=read&aSeq=380555.
Livingston, D. H., Tripp, T., Biggs, C., & Lavery, R. F. (2009). A fate worse than death? Long-term outcome of trauma patients admitted to the surgical intensive care unit. Journal of Trauma and Acute Care Surgery. https://doi.org/10.1097/TA.0b013e3181a5cc34.
van Delft-Schreurs, C. C. H. M., van Bergen, J. J. M., de Jongh, M. A. C., van de Sande, P., Verhofstad, M. H. J., & de Vries, J. (2014). Quality of life in severely injured patients depends on psychosocial factors rather than on severity or type of injury. Injury. https://doi.org/10.1016/j.injury.2013.02.025.
The World Health Organization Quality of Life Group. (1995). The World Health Organization quality of life assessment (WHOQOL): position paper from the World Health Organization. Social Science and Medicine. https://doi.org/10.1016/0277-9536(95)00112-K.
Kim, K., Kim, Y. M., & Kim, E. K. (2014). Correlation between the activities of daily living of stroke patients in a community setting and their quality of life. Journal of Physical Therapy Science. https://doi.org/10.1589/jpts.26.417.
Christensen, M. C., Banner, C., Lefering, R., Vallejo-Torres, L., & Morris, S. (2011). Quality of life after severe trauma: results from the global trauma trial with recombinant factor VII. Journal of Trauma and Acute Care Surgery. https://doi.org/10.1097/TA.0b013e3181f053c2.
Polinder, S., Haagsma, J. A., Belt, E., Lyons, R. A., Erasmus, V., Lund, J., et al. (2010). A systematic review of studies measuring health-related quality of life of general injury populations. BMC Public Health. https://doi.org/10.1186/1471-2458-10-783.
Boekamp, J. R., Overholser, J. C., & Schubert, D. S. (1996). Depression following a spinal cord injury. The International Journal of Psychiatry in Medicine. https://doi.org/10.2190/CMU6-24AH-E4JG-8KBN.
Chang, F. H., Wang, Y. H., Jang, Y., & Wang, C. W. (2012). Factors associated with quality of life among people with spinal cord injury: application of the International Classification of Functioning, Disability and Health model. Archives of Physical Medicine and Rehabilitation. https://doi.org/10.1016/j.apmr.2012.06.008.
Elsherbiny, O. E. E., Salem, M. A., El-Sabbagh, A. H., Elhadidy, M. R., & Eldeen, S. M. A. (2011). Quality of life of adult patients with severe burns. Burns. https://doi.org/10.1016/j.burns.2010.12.017.
Jain, N. B., Sullivan, M., Kazis, L. E., Tun, C. G., & Garshick, E. (2007). Factors associated with health-related quality of life in chronic spinal cord injury. American Journal of Physical Medicine and Rehabilitation/Association of Academic Physiatrists. https://doi.org/10.1097/PHM.0b013e31804a7d00.
Soberg, H. L., Røe, C., Anke, A., Arango-Lasprilla, J. C., Skandsen, T., Sveen, U., et al. (2013). Health-related quality of life 12 months after severe traumatic brain injury: a prospective nationwide cohort study. Journal of Rehabilitation Medicine. https://doi.org/10.2340/16501977-1158.
Baker, E., Xyrichis, A., Norton, C., Hopkins, P., & Lee, G. (2018). The long-term outcomes and health-related quality of life of patients following blunt thoracic injury: a narrative literature review. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine. https://doi.org/10.1186/s13049-018-0535-9.
Ciaramitaro, P., Mondelli, M., Logullo, F., Grimaldi, S., Battiston, B., Sard, A., et al. (2010). Traumatic peripheral nerve injuries: epidemiological findings, neuropathic pain and quality of life in 158 patients. Journal of the Peripheral Nervous System. https://doi.org/10.1111/j.1529-8027.2010.00260.x.
Yom, Y. H., & Han, J. H. (2014). Factors associated with oral health related-quality of life in elderly persons: applying Andersen’s model. Journal of Korean Academy of Fundamentals of Nursing. https://doi.org/10.7739/jkafn.2014.21.1.18.
Andersen, R. (1968). A behavioral model of families’ use of health services. Chicago, IL: University of Chicago.
Andersen, R. M. (1995). Revisiting the behavioral model and access to medical care: does it matter? Journal of Health and Social Behavior. https://doi.org/10.2307/2137284.
Willet, M., Dorstyn, D., Due, C., & Li, W. (2018). Applying Andersen’s model to explain service use and quality of life among Australian caregivers of children with autism spectrum disorder. Journal of Developmental and Physical Disabilities. https://doi.org/10.1007/s10882-018-9589-x.
Gaber, A., Galarneau, C., Feine, J. S., & Emami, E. (2018). Rural-urban disparity in oral health-related quality of life. Community Dentistry and Oral Epidemiology. https://doi.org/10.1111/cdoe.12344.
Buhse, M., Della Ratta, C., Galiczewski, J., & Eckardt, P. (2015). Caregivers of older persons with multiple sclerosis: determinants of health-related quality of life. Journal of Neuroscience Nursing. https://doi.org/10.1097/JNN.0000000000000117.
Alenzi, E. O., & Sambamoorthi, U. (2016). Depression treatment and health-related quality of life among adults with diabetes and depression. Quality of Life Research. https://doi.org/10.1007/s11136-015-1189-y.
Lee, D. Y., & Park, J. D. (2011). A study on the factors for the elderly living alone at home to determine their participation in a health promotion activity program: with the application of Anderson model. Social Welfare Policy, 38(4), 1–23.
Wannapakhe, J., Amatachaya, S., Siritaratiwat, W., Arrayawichanon, P., & Wattanapan, P. (2010). Physical abilities, quality of life, incidences of complications and falls in patients with chronic spinal cord injury after discharge. Journal of Medical Technology and Physical Therapy, 22(2), 188–195.
Korea Centers for Disease Control and Prevention. (2018). The Seventh Korea National Health and Nutrition Examination Survey. Cheongju: Korea Centers for Disease Control and Prevention.
Öster, C., Willebrand, M., Dyster-Aas, J., Kildal, M., & Ekselius, L. (2009). Validation of the EQ-5D questionnaire in burn injured adults. Burns. https://doi.org/10.1016/j.burns.2008.11.007.
Hung, M. C., Lu, W. S., Chen, S. S., Hou, W. H., Hsieh, C. L., & Wang, J. D. (2015). Validation of the EQ-5D in patients with traumatic limb injury. Journal of Occupational Rehabilitation. https://doi.org/10.1007/s10926-014-9547-0.
Malmivaara, K., Kivisaari, R., Hernesniemi, J., & Siironen, J. (2011). Cost-effectiveness of decompressive craniectomy in traumatic brain injuries. European Journal of Neurology. https://doi.org/10.1111/j.1468-1331.2010.03294.x.
Janssen, M. F., Szende, A., Cabases, J., Ramos-Goñi, J. M., Vilagut, G., & König, H. H. (2019). Population norms for the EQ-5D-3L: a cross-country analysis of population surveys for 20 countries. The European Journal of Health Economics. https://doi.org/10.1007/s10198-018-0955-5.
Lee, K. J., Jang, H. I., Lee, B. S., Lee, J. E., Han, S. H., & Kim, E. J. (2015). The determinant factors of quality of life in age-specific differences of spinal cord injury : Comparison of Korean youth and middle-aged adults. Journal of Rehabilitation Psychology, 22(1), 25–39.
Choi, J. S., Lee, E. H., So, A. Y., & Lee, K. S. (2012). Quality of life in the urban adults by age. Journal of Muscle Joint Health. https://doi.org/10.5953/JMJH.2012.19.3.362.
VanDerwerker, C. J., Gregory, C. M., & Simpson, K. N. (2019). Using inferred mobility status to estimate the time to major depressive disorder diagnosis post-spinal cord injury. Archives of Physical Medicine and Rehabilitation. https://doi.org/10.1016/j.apmr.2019.11.014.
Büyüktür, A. G., Ackerman, M. S., Newman, M. W., & Hung, P. Y. (2017). Design considerations for semi-automated tracking: self-care plans in spinal cord injury. In Proceedings of the 11th EAI International Conference on Pervasive Computing Technologies for Healthcare.
Seo, K. S., & Yeom, E. Y. (2018). Effects of family cohesion and self-care agency on the quality of life in community-dwelling elderly. Journal of the Korea Contents Association. https://doi.org/10.5392/JKCA.2018.18.12.516.
Sidani, S. (2003). Self-care. Nursing sensitive outcomes: the state of the science. Toronto: Jones and Bartlett Learning.
Allison, S. E. (2007). Self-care requirements for activity and rest: an Orem nursing focus. Nursing Science Quarterly. https://doi.org/10.1177/0894318406296297.
Langley, J., Davie, G., Wilson, S., Lilley, R., Ameratunga, S., Wyeth, E., & Derrett, S. (2013). Difficulties in functioning 1 year after injury: the role of preinjury sociodemographic and health characteristics, health care and injury-related factors. Archives of Physical Medicine and Rehabilitation. https://doi.org/10.1016/j.apmr.2013.02.012.
Garcia-Gordillo, M. A., Adsuar, J. C., & Olivares, P. R. (2016). Normative values of EQ-5D-5L: in a Spanish representative population sample from Spanish Health Survey, 2011. Quality of Life Research. https://doi.org/10.1007/s11136-015-1164-7.
Pillastrini, P., Mugnai, R., Bonfiglioli, R., Curti, S., Mattioli, S., Maioli, M. G., et al. (2008). Evaluation of an occupational therapy program for patients with spinal cord injury. Spinal Cord. https://doi.org/10.1038/sj.sc.3102072.
Cho, Y. W., & Cho, K. H. (2014). The study of quality of life between disabled and non-disabled people’s economic capability: the mediating effect of mental health factor via structural equation model multi-group analysis. Health and Social Welfare Review, 34(2), 276–309.
Kreuter, M., Siösteen, A., Erkholm, B., Byström, U., & Brown, D. J. (2005). Health and quality of life of persons with spinal cord lesion in Australia and Sweden. Spinal Cord. https://doi.org/10.1038/sj.sc.3101692.
Lee, H. J. (2009). An exploratory study on factors affecting quality of life for the elderly: focusing on socioeconomic and social capital traits. Stress Research, 17(2), 131–141.
Tramonti, F., Bonfiglio, L., Bongioanni, P., Belviso, C., Fanciullacci, C., Rossi, B., et al. (2019). Caregiver burden and family functioning in different neurological diseases. Psychology, Health and Medicine. https://doi.org/10.1080/13548506.2018.1510131.
Kim, M. O., Park, S. J., & Sohn, G. H. (2016). The mediating effect of depression on the relation between self-esteem of central nervous system injury patients’ caregivers and quality of life. Journal of Rehabilitation Psychology, 23(2), 299–313.
Qadeer, A., Khalid, U., Amin, M., Murtaza, S., Khaliq, M. F., & Shoaib, M. (2017). Caregiver’s burden of the patients with traumatic brain injury. Cureus. https://doi.org/10.7759/cureus.1590.
Kennedy, P., & Rogers, B. A. (2000). Anxiety and depression after spinal cord injury: a longitudinal analysis. Archives of Physical Medicine and Rehabilitation. https://doi.org/10.1053/apmr.2000.5580.
Craig, A., Tran, Y., & Middleton, J. (2009). Psychological morbidity and spinal cord injury: a systematic review. Spinal Cord. https://doi.org/10.1038/sc.2008.115.
Yoo, Y. S. (2000). A study on variables relating to marital satisfaction of the spinal cord injury couples. Korean Journal of Family Social Work, 5, 185–222.
Dryden, D. M., Saunders, L. D., Rowe, B. H., May, L. A., Yiannakoulias, N., Svenson, L. W., et al. (2005). Depression following traumatic spinal cord injury. Neuroepidemiology. https://doi.org/10.1159/000086284.
Daniel, A., & Manigandan, C. (2005). Efficacy of leisure intervention groups and their impact on quality of life among people with spinal cord injury. International Journal of Rehabilitation Research. https://doi.org/10.1097/00004356-200503000-00006.
McVeigh, S. A., Hitzig, S. L., & Craven, B. C. (2009). Influence of sport participation on community integration and quality of life: a comparison between sport participants and non-sport participants with spinal cord injury. The journal of spinal cord medicine. https://doi.org/10.1080/10790268.2009.11760762.
Tyagi, N., Goel, S. A., & Alexander, M. (2019). Improving quality of life after spinal cord injury in India with telehealth. Spinal Cord Series and Cases. https://doi.org/10.1038/s41394-019-0212-x.
Lee, I. S., Kim, D. K., & Um, T. Y. (2007). The study of relationship between self-respect and quality of life, and mediation effect of depression among the recipients of the medical security with a chronic disease. Korean Journal of Social Welfare Research, 17, 79–104.
Edelman, L. S. (2007). Social and economic factors associated with the risk of burn injury. Burns. https://doi.org/10.1016/j.burns.2007.05.002.
Bisgaier, J., Cutts, D. B., Edelstein, B. L., & Rhodes, K. V. (2011). Disparities in child access to emergency care for acute oral injury. Pediatrics. https://doi.org/10.1542/peds.2011-0011.
Nirula, R., Nirula, G., & Gentilello, L. M. (2009). Inequity of rehabilitation services after traumatic injury. Journal of Trauma and Acute Care Surgery. https://doi.org/10.1097/TA.0b013e31815ede46.
Aitken, L. M., Davey, T. M., Ambrose, J., Connelly, L. B., Swanson, C., & Bellamy, N. (2007). Health outcomes of adults 3 months after injury. Injury. https://doi.org/10.1016/j.injury.2006.05.020.
Acknowledgements
Korea Centers for Disease Control and Prevention provided the data for this study. This work is not funded.
Author information
Authors and Affiliations
Contributions
A designed the study and performed the statistical analyses and description of study methods and results. B involved the design of the study, reviewed literatures and wrote the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no actual or potential conflicts of interest.
Ethical approval
The study was approved by the Kyungpook National University’s Institutional Review Board (no. KNU 2020-0035). Ethical issues regarding plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, and redundancy have been completely observed by the author.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, E., Kim, Y. How do the influencing factors of health-related quality of life of the injured patient differ according to activity limitations?. Qual Life Res 30, 1103–1118 (2021). https://doi.org/10.1007/s11136-020-02708-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-020-02708-x