Abstract
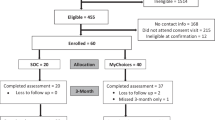
Communicating personalized genomic risk results for common diseases to the general population as a form of tailored prevention is novel and may require alternative genetic counseling service delivery models. We describe the development and evaluation of a communication protocol for disclosing melanoma genomic risk information to the asymptomatic general population and assess participants’ satisfaction and acceptability. Participants (n = 117) were aged 22–69 years, living in New South Wales, Australia and unselected for family history. They provided a saliva sample and had genomic testing for melanoma for low to moderate penetrant melanoma susceptibility variants in 21 genes. Participants could choose to receive their results from a genetic counselor via telephone, followed by a mailed booklet or to receive their risk result via mailed booklet only with a follow-up call for those at high risk. A follow-up questionnaire was completed by 85% of participants 3-months later. Most participants (80%) elected to receive their result via telephone. Participants were highly satisfied with the delivery of results (mean 3.4 out of 4, standard deviation 0.5), and this did not differ by delivery mode, risk category, age or sex. On follow-up, 75% accurately recalled their risk category, 6% indicated a preference for a different delivery mode, either electronic or face-to-face. The process of disclosing genomic risk results to the general population over the telephone with accompanying written material was feasible and acceptable, and may be useful for communicating polygenic risk for common diseases in the context of increasing demands for genomic testing.

Similar content being viewed by others
References
Armstrong, B. K., & Kricker, A. (1993). How much melanoma is caused by sun exposure? Melanoma Research, 3(6), 395–401.
Baumanis, L., Evans, J., Callanan, N., & Susswein, L. (2009). Telephoned BRCA1/2 genetic test results: Prevalence, practice and patient satisfaction. Journal of Genetic Counseling, 18, 447–463.
Buchanan, A. H., Rahm, A. K., & Williams, J. L. (2016). Alternate service delivery models in cancer genetic counseling: A mini-review. Frontiers in Oncology, 6, 120.
Burton, H., Chowdhury, S., Dent, T., Hall, A., Pashayan, N., & Pharoah, P. (2013). Public health implications from COGS and potential for risk stratification and screening. Nature Genetics, 45(4), 349–351.
Butterfield, L. D., Borgen, W. A., Amundson, N. E., & Maglio, A. T. (2005). Fifty years of the critical incident technique: 1954-2004 and beyond. Qualitative Research, 5(4), 475–497.
Cherkas, L. F., Harris, J. M., Levinson, E., Spector, T. D., & Prainsack, B. (2010). A survey of UK public interest in internet-based personal genome testing. PLoS One, 5(10), e13473.
Christensen, K. D., Roberts, J. S., Shalowitz, D. I., Everett, J. N., Kim, S. Y., Raskin, L., et al. (2011). Disclosing individual CDKN2A research results to melanoma survivors: Interest, impact, and demands on researchers. Cancer Epidemiology, Biomarkers & Prevention, 20(3), 522–529.
Cohen, S. A., Marvin, M. L., Riley, B. D., Vig, H. S., Rousseau, J. A., & Gustafson, S. L. (2013). Identification of genetic counseling service delivery models in practice: A report from the NSGC Service delivery model task force. Journal of Genetic Counseling, 22(4), 411–421.
Edwards, A., Gray, J., Clarke, A., Dundon, J., Elwyn, G., Gaff, C., et al. (2008). Interventions to improve risk communication in clinical genetics: Systematic review. Patient Education and Counseling, 71(1), 4–25.
Fagerlin, A., Ubel, P. A., Smith, D. M., & Zikmund-Fisher, B. J. (2007). Making numbers matter: Present and future research in risk communication. American Journal of Health Behavior, 31(Suppl 1), S47–S56.
Foulkes, W. D., Knoppers, B. M., & Turnbull, C. (2016). Population genetic testing for cancer susceptibility: Founder mutations to genomes. Nature Reviews. Clinical Oncology, 13(1), 41–54.
Godard, B., Kaariainen, H., Kristoffersson, U., Tranebjaerg, L., Coviello, D., & Ayme, S. (2003). Provision of genetic services in Europe: Current practices and issues. European Journal of Human Genetics, 11(Suppl 2), S13–S48.
Graves, K. D., Leventhal, K. G., Nusbaum, R., Salehizadeh, Y., Hooker, G. W., Peshkin, B. N., et al. (2013). Behavioral and psychosocial responses to genomic testing for colorectal cancer risk. Genomics, 102(2), 123–130.
Green, A. C., Williams, G. M., Logan, V., & Strutton, G. M. (2011). Reduced melanoma after regular sunscreen use: Randomized trial follow-up. Journal of Clinical Oncology, 29(3), 257–263.
Gurmankin, A. D., Domchek, S., Stopfer, J., Fels, C., & Armstrong, K. (2005). Patients’ resistance to risk information in genetic counseling for brca1/2. Archives of Internal Medicine, 165(5), 523–529.
Hallowell, N., Green, J. M., Statham, H., Murton, F., & Richards, M. P. M. (1997). Recall of numerical risk estimates and counsellees' perceptions of the importance of risk information following genetic counselling for breast and ovarian cancer. Psychology, Health & Medicine, 2(2), 149–159.
Hawley, S. T., Zikmund-Fisher, B., Ubel, P., Jancovic, A., Lucas, T., & Fagerlin, A. (2008). The impact of the format of graphical presentation on health-related knowledge and treatment choices. Patient Education and Counseling, 73(3), 448–455.
Hooker, G. W., Babu, D., Myers, M., Zierhut, H., & McAllister, M. (2017). Standards for the reporting of genetic counseling interventions in research and other studies (GCIRS): An NSGC task force report. Journal of Genetic Counseling, 26(3), 355–360.
Human Genetics Society of Australasia. (2012). Guideline; Process of Genetic Counselling. Retrieved from https://www.hgsa.org.au/documents/item/13
Jenkins, J., Calzone, K. A., Dimond, E., Liewehr, D. J., Steinberg, S. M., Jourkiv, O., et al. (2007). Randomized comparison of phone versus in-person BRCA1/2 predisposition genetic test result disclosure counseling. Genetics in Medicine, 9(8), 487–495.
Kasparian, N., Wakefield, C., & Meiser, B. (2007). Assessment of psychosocial outcomes in genetic counseling research: An overview of available measurement scales. Journal of Genetic Counseling, 16(6), 693–712.
Lautenbach, D. M., Christensen, K. D., Sparks, J. A., & Green, R. C. (2013). Communicating genetic risk information for common disorders in the era of genomic medicine. Annual Review of Genomics and Human Genetics, 14, 491–513.
Leachman, S. A., Lucero, O. M., Sampson, J. E., Cassidy, P., Bruno, W., Queirolo, P., et al. (2017). Identification, genetic testing, and management of hereditary melanoma. Cancer and Metastasis Reviews, 36(1), 77–90.
Lloyd, S., Watson, M., Waites, B., Meyer, L., Eeles, R., Ebbs, S., et al. (1996). Familial breast cancer: A controlled study of risk perception, psychological morbidity and health beliefs in women attending for genetic counselling. British Journal of Cancer, 74(3), 482–487.
McBride, C. M., Bryan, A. D., Bray, M. S., Swan, G. E., & Green, E. D. (2012). Health behavior change: Can genomics improve behavioral adherence? American Journal of Public Health, 102(3), 401–405.
McBride, C. M., Birmingham, W. C., & Kinney, A. Y. (2015). Health psychology and translational genomic research: Bringing innovation to cancer-related behavioral interventions. The American Psychologist, 70(2), 91–104.
Modell, S. M., Kardia, S. L. R., & Citrin, T. (2014). Stakeholder consultation insights on the future of genomics at the clinical-public health interface. Translational Research, 163(5), 466–477.
Patrick-Miller, L. J., Egleston, B. L., Fetzer, D., Forman, A., Bealin, L., Rybak, C., et al. (2014). Development of a communication protocol for telephone disclosure of genetic test results for cancer predisposition. JMIR Res Protoc, 3(4), e49.
Peshkin, B. N., Kelly, S., Nusbaum, R. H., Similuk, M., DeMarco, T. A., Hooker, G. W., et al. (2016). Patient perceptions of telephone vs. in-person BRCA1/BRCA2 genetic counseling. Journal of Genetic Counseling, 25(3), 472–482.
Salemink, S., Dekker, N., Kets, C. M., van der Looij, E., van Zelst-Stams, W. A. G., & Hoogerbrugge, N. (2013). Focusing on patient needs and preferences may improve genetic counseling for colorectal cancer. Journal of Genetic Counseling, 22(1), 118–124.
Schmidlen, T. J., Wawak, L., Kasper, R., García-España, J. F., Christman, M. F., & Gordon, E. S. (2014). Personalized genomic results: Analysis of informational needs. Journal of Genetic Counseling, 23(4), 578–587.
Shelton, C. A., & Whitcomb, D. C. (2015). Evolving roles for physicians and genetic counselors in managing complex genetic disorders. Clin Transl Gastroenterol, 6, e124.
Sie, A. S., van Zelst-Stams, W. A., Spruijt, L., Mensenkamp, A. R., Ligtenberg, M. J., Brunner, H. G., et al. (2014). More breast cancer patients prefer BRCA-mutation testing without prior face-to-face genetic counseling. Familial Cancer, 13(2), 143–151.
Sie, A. S., Spruijt, L., van Zelst-Stams, W. A., Mensenkamp, A. R., Ligtenberg, M. J., Brunner, H. G., et al. (2016). High satisfaction and low distress in breast cancer patients one year after BRCA-mutation testing without prior face-to-face genetic counseling. Journal of Genetic Counseling, 25(3), 504–514.
Smerecnik, C. M., Mesters, I., Verweij, E., de Vries, N. K., & de Vries, H. (2009). A systematic review of the impact of genetic counseling on risk perception accuracy. Journal of Genetic Counseling, 18(3), 217–228.
Smit, A. K., Keogh, L. A., Newson, A. J., Hersch, J., Butow, P., & Cust, A. E. (2015). Exploring the potential emotional and Behavioural impact of providing personalised genomic risk information to the public: A focus group study. Public Health Genomics, 18(5), 309–317.
Smit, A. K., Keogh, L. A., Hersch, J., Newson, A. J., Butow, P., Williams, G., et al. (2016). Public preferences for communicating personal genomic risk information: A focus group study. Health Expectations, 19(6), 1203–1214.
Smit, A. K., Espinoza, D., Newson, A. J., Morton, R. L., Fenton, G., Freeman, L., et al. (2017). A pilot randomized controlled trial of the feasibility, acceptability, and impact of giving information on personalized genomic risk of melanoma to the public. Cancer Epidemiology, Biomarkers & Prevention, 26(2), 212–221.
Vos, J., Gomez-Garcia, E., Oosterwijk, J. C., Menko, F. H., Stoel, R. D., van Asperen, C. J., et al. (2012a). Opening the psychological black box in genetic counseling. The psychological impact of DNA testing is predicted by the counselees' perception, the medical impact by the pathogenic or uninformative BRCA1/2-result. Psychooncology, 21(1), 29–42.
Vos, J., Oosterwijk, J. C., Gomez-Garcia, E., Menko, F. H., Collee, M. J., van Asperen, C. J., et al. (2012b). Exploring the short-term impact of DNA-testing in breast cancer patients: The counselees' perception matters, but the actual BRCA1/2 result does not. Patient Education and Counseling, 86(2), 239–251.
Weinstock, M. A. (2012). Reducing death from melanoma and standards of evidence. The Journal of Investigative Dermatology, 132(5), 1311–1312.
Acknowledgements
The study would like to thank Elvira Zilliacus for her contribution. This study received funding from Sydney Catalyst Translational Cancer Research Centre and The University of Sydney Cancer Strategic Priority Area for Research Collaboration (SPARC) Implementation Scheme. A.E. Cust received Career Development Fellowships from the National Health and Medical Research Council of Australia (NHMRC; 1063593) and Cancer Institute NSW (15/CDF/1-14). A.K. Smit received a Research Training Program (RTP) Stipend Scholarship and a Merit Top Up Scholarship from the University of Sydney, and a Top Up Scholar Award from the Sydney Catalyst Translational Cancer Research Centre.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human Studies and Informed Consent
All procedures followed were in accordance with the ethical standards of the responsible institutional review committees of the collaborating institutions, national guidelines, and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all individual participants included in the study.
Animal Studies
No animal studies were carried out by the authors for this article.
Rights and permissions
About this article
Cite this article
Fenton, G.L., Smit, A.K., Freeman, L. et al. Development and Evaluation of a Telephone Communication Protocol for the Delivery of Personalized Melanoma Genomic Risk to the General Population. J Genet Counsel 27, 370–380 (2018). https://doi.org/10.1007/s10897-017-0183-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10897-017-0183-7