Abstract
Purpose
To develop a prognostic model to predict 30-day mortality following colorectal cancer (CRC) surgery using the Surveillance, Epidemiology, and End Results (SEER)-Medicare-linked data and to assess whether race/ethnicity, neighborhood, and hospital characteristics influence model performance.
Methods
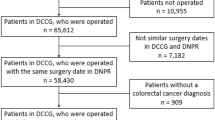
We included patients aged 66 years and older from the linked 2000–2005 SEER-Medicare database. Outcome included 30-day mortality, both in-hospital and following discharge. Potential prognostic factors included tumor, treatment, sociodemographic, hospital, and neighborhood characteristics (census-tract-poverty rate). We performed a multilevel logistic regression analysis to account for nesting of CRC patients within hospitals. Model performance was assessed using the area under the receiver operating characteristic curve (AUC) for discrimination and the Hosmer–Lemeshow goodness-of-fit test for calibration.
Results
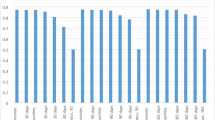
In a model that included all prognostic factors, important predictors of 30-day mortality included age at diagnosis, cancer stage, and mode of presentation. Race/ethnicity, census-tract-poverty rate, and hospital characteristics were independently associated with 30-day mortality, but they did not influence model performance. Our SEER-Medicare model achieved moderate discrimination (AUC = 0.76), despite suboptimal calibration.
Conclusions
We developed a prognostic model that included tumor, treatment, sociodemographic, hospital, and neighborhood predictors. Race/ethnicity, neighborhood, and hospital characteristics did not improve model performance compared with previously developed models.

Similar content being viewed by others
References
Siegel R, Naishadham D, Jemal A (2013) Cancer statistics, 2013. CA Cancer J Clin 63:11–30
Billingsley KG, Morris AM, Dominitz JA et al (2007) Surgeon and hospital characteristics as predictors of major adverse outcomes following colon cancer surgery: understanding the volume-outcome relationship. Arch Surg 142:23–31
Iversen LH, Harling H, Laurberg S, Wille-Jorgensen P (2007) Influence of caseload and surgical speciality on outcome following surgery for colorectal cancer: a review of evidence. Part 1: short-term outcome. Colorectal Dis 9:28–37
Rosen L, Stasik JJ Jr, Reed JF 3rd, Olenwine JA, Aronoff JS, Sherman D (1996) Variations in colon and rectal surgical mortality. Comparison of specialties with a state-legislated database. Dis Colon Rectum 39:129–135
Sagar PM, Hartley MN, MacFie J, Taylor BA, Copeland GP (1996) Comparison of individual surgeon’s performance. Risk-adjusted analysis with POSSUM scoring system. Dis Colon Rectum 39:654–658
Sagar PM, Hartley MN, Mancey-Jones B, Sedman PC, May J, Macfie J (1994) Comparative audit of colorectal resection with the POSSUM scoring system. Br J Surg 81:1492–1494
Copeland GP, Jones D, Walters M (1991) POSSUM: a scoring system for surgical audit. Br J Surg 78:355–360
Prytherch DR, Whiteley MS, Higgins B, Weaver PC, Prout WG, Powell SJ (1998) POSSUM and Portsmouth POSSUM for predicting mortality. Physiological and Operative Severity Score for the enUmeration of Mortality and morbidity. Br J Surg 85:1217–1220
Tekkis PP, Prytherch DR, Kocher HM et al (2004) Development of a dedicated risk-adjustment scoring system for colorectal surgery (colorectal POSSUM). Br J Surg 91:1174–1182
Tekkis PP, Poloniecki JD, Thompson MR, Stamatakis JD (2003) Operative mortality in colorectal cancer: prospective national study. BMJ 327:1196–1201
Fazio VW, Tekkis PP, Remzi F, Lavery IC (2004) Assessment of operative risk in colorectal cancer surgery: the Cleveland Clinic Foundation colorectal cancer model. Dis Colon Rectum 47:2015–2024
Richards CH, Leitch FE, Horgan PG, McMillan DC (2010) A systematic review of POSSUM and its related models as predictors of post-operative mortality and morbidity in patients undergoing surgery for colorectal cancer. J Gastrointest Surg 14:1511–1520
Senagore AJ, Warmuth AJ, Delaney CP, Tekkis PP, Fazio VW (2004) POSSUM, p-POSSUM, and Cr-POSSUM: implementation issues in a United States health care system for prediction of outcome for colon cancer resection. Dis Colon Rectum 47:1435–1441
Al-Homoud S, Purkayastha S, Aziz O et al (2004) Evaluating operative risk in colorectal cancer surgery: ASA and POSSUM-based predictive models. Surg Oncol 13:83–92
Teeuwen PH, Bremers AJ, Groenewoud JM, van Laarhoven CJ, Bleichrodt RP (2011) Predictive value of POSSUM and ACPGBI scoring in mortality and morbidity of colorectal resection: a case–control study. J Gastrointest Surg 15:294–303
Ferjani AM, Griffin D, Stallard N, Wong LS (2007) A newly devised scoring system for prediction of mortality in patients with colorectal cancer: a prospective study. Lancet Oncol 8:317–322
Fichera A (2005) How accurate is the Cleveland Clinic Foundation model in predicting operative risk in colorectal cancer patients? Nat Clin Pract Oncol 2:258–259
Schneider EB, Haider AH, Hyder O, Efron JE, Lidor AO, Pawlik TM (2013) Assessing short- and long-term outcomes among black vs white Medicare patients undergoing resection of colorectal cancer. Am J Surg 205:402–408
Bharathan B, Welfare M, Borowski DW et al (2011) Impact of deprivation on short- and long-term outcomes after colorectal cancer surgery. Br J Surg 98:854–865
Schootman M, Lian M, Pruitt SL et al (2014) Hospital and geographic variability in thirty-day all-cause mortality following colorectal cancer surgery. Health Serv Res 49:1145–1164
Smith JJ, Tekkis PP (2010) ACPGBI colorectal cancer model. Available at: www.riskprediction.org.uk/index-crc.php. Accessed 11 July 2013
Alvarez C, Clark C, Zhang S et al (2013) Predicting out of intensive care unit cardiopulmonary arrest or death using electronic medical record data. BMC Med Inform Decis Mak 13:28
Warren JL, Klabunde CN, Schrag D, Bach PB, Riley GF (2002) Overview of the SEER-Medicare data: content, research applications, and generalizability to the United States elderly population. Med Care 40(8 Suppl):IV-3–IV-18
Cooper GS, Virnig B, Klabunde CN, Schussler N, Freeman J, Warren JL (2002) Use of SEER-Medicare data for measuring cancer surgery. Med Care 40(8 Suppl):IV-43–IV-48
Archampong D, Borowski D, Wille-Jorgensen P, Iversen LH (2012) Workload and surgeon’s specialty for outcome after colorectal cancer surgery. Cochrane Database of Syst Rev 3:Cd005391
Chien LC, Schootman M, Pruitt SL (2013) The modifying effect of patient location on stage-specific survival following colorectal cancer using geosurvival models. Cancer Causes Control 24:473–484
Kolfschoten NE, Marang van de Mheen PJ, Gooiker GA et al (2011) Variation in case-mix between hospitals treating colorectal cancer patients in the Netherlands. Eur J Surg Oncol 37:956–963
Morris EJ, Taylor EF, Thomas JD et al (2011) Thirty-day postoperative mortality after colorectal cancer surgery in England. Gut 60:806–813
Klabunde CN, Potosky AL, Legler JM, Warren JL (2000) Development of a comorbidity index using physician claims data. J Clin Epidemiol 53:1258–1267
Royston P, Moons KG, Altman DG, Vergouwe Y (2009) Prognosis and prognostic research: developing a prognostic model. BMJ 338:b604
Steyerberg EW (2009) Clinical prediction models: a practical approach to development, validation, and updating. Springer, New York
Steyerberg EW, Neville BA, Koppert LB et al (2006) Surgical mortality in patients with esophageal cancer: development and validation of a simple risk score. J Clin Oncol 24:4277–4284
Hosmer DW, Hosmer T, Le Cessie S, Lemeshow S (1997) A comparison of goodness-of-fit tests for the logistic regression model. Stat Med 16:965–980
Harrell FE Jr, Lee KL, Mark DB (1996) Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med 15:361–387
Pencina MJ, D’Agostino RB, Pencina KM, Janssens AC, Greenland P (2012) Interpreting incremental value of markers added to risk prediction models. Am J Epidemiol 176:473–481
Smulders YM, Thijs A, Twisk JW (2008) New cardiovascular risk determinants do exist and are clinically useful. Eur Heart J 29:436–440
Dogrul AB, Kilic YA, Celebi AE et al (2010) External validation of Cleveland Clinic Foundation colorectal cancer model in a University Clinic in terms of predicting operative mortality. Tech Coloproctol 14:9–12
Tabak YP, Sun X, Johannes RS, Hyde L, Shorr AF, Lindenauer PK (2013) Development and validation of a mortality risk-adjustment model for patients hospitalized for exacerbations of chronic obstructive pulmonary disease. Med Care 51:597–605
Hosmer DW, Lemeshow S (1980) Goodness of fit tests for the multiple logistic regression model. Commun Stat Theory Methods 9:1043–1069
Dekker JW, Gooiker GA, van der Geest LG et al (2012) Use of different comorbidity scores for risk-adjustment in the evaluation of quality of colorectal cancer surgery: does it matter? Eur J Surg Oncol 38:1071–1078
Bann SD, Sarin S (2001) Comparative audit: the trouble with POSSUM. J R Soc Med 94:632–634
Ash AS, Fienberg SE, Louis TA, Normand SL, Stukel TA, Utts J (2011) Statistical issues on assessing hospital performance. The COPSS-CMS White Paper Committee
Acknowledgments
This work was supported by grants from the National Cancer Institute at the National Institutes of Health (Grant Number CA112159); and the Health Behavior, Communication, and Outreach Core; the Core is supported in part by the National Cancer Institute Cancer Center Support Grant (Grant Number P30 CA91842) to the Alvin J. Siteman Cancer Center at Washington University School of Medicine and Barnes-Jewish Hospital in St. Louis, Missouri. Dr. Davidson was supported in part through Grants HL-38180, DK-56260, and Digestive Disease Research Core Center DK-52574. We gratefully acknowledge James Struthers for his data management and programming services. We thank the Alvin J. Siteman Cancer Center at Barnes-Jewish Hospital and Washington University School of Medicine in St. Louis, Missouri, for the use of the Health Behavior, Communication, and Outreach Core. This study used the linked SEER-Medicare database. The interpretation and reporting of these data are the sole responsibility of the authors. The authors acknowledge the efforts of the Applied Research Program, NCI; the Office of Research, Development and Information, CMS; Information Management Services (IMS), Inc.; and the Surveillance, Epidemiology, and End Results (SEER) Program tumor registries in the creation of the SEER-Medicare database.
Conflict of interest
The authors state that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
de Vries, S., Jeffe, D.B., Davidson, N.O. et al. Postoperative 30-day mortality in patients undergoing surgery for colorectal cancer: development of a prognostic model using administrative claims data. Cancer Causes Control 25, 1503–1512 (2014). https://doi.org/10.1007/s10552-014-0451-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-014-0451-x