Abstract
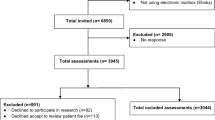
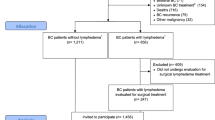
We sought to assess the association of breast cancer-related lymphedema (BCRL) with the ability to perform upper extremity activities of daily living (ADL) in our patient population. 324 breast cancer patients who had received treatment for unilateral breast cancer at our institution between 2005 and 2014 were prospectively screened for lymphedema. Bilateral arm measurements were performed pre-operatively and during post-operative follow-up using a Perometer. Patients completed an extensive quality of life (QOL) questionnaire at the time of each study assessment. Lymphedema was defined as a relative volume change (RVC) of ≥10% from the patient’s pre-operative baseline measurement. Linear regression models were used to evaluate the relationship between post-operative arm function score (as a continuous variable) and RVC, demographic, clinical, and QOL factors. By multivariate analysis, greater fear of lymphedema (p < 0.0001), more pain (p < 0.0001), body mass index >25 (p = 0.0015), mastectomy (p = 0.0001), and having an axillary node dissection (p = 0.0045) were all associated with lower functional scores. Higher emotional well-being score (p < 0.0001) and adjuvant chemotherapy (p = 0.0005) were associated with higher post-operative functional score. Neither low-level volume changes (5–10 % RVC) nor BCRL (RVC ≥10 %) were associated with ability to perform upper extremity ADL as measured by self-report (p = 0.99, p = 0.79). This prospective study demonstrates that low-level changes in arm volume (RVC 5–10 %) as well as clinically significant BCRL (RVC ≥10 %) did not impact the self-reported ability to use the affected extremity for ADL. These findings may help to inform clinicians and patients on the importance of prospective screening for lymphedema and QOL which enables early detection and intervention.
Similar content being viewed by others
References
Lane K, Worsley D, McKenzie D (2005) Exercise and the lymphatic system: implications for breast-cancer survivors. Sports Med 35(6):461–471
Kilbreath SL, Refshauge KM, Ward LC, Kastanias K, Yee J, Koelmeyer LA et al (2013) Factors affecting the preoperative and postoperative extracellular fluid in the arm on the side of breast cancer: a cohort study. Lymphat Res Biol 11(2):66–71
Johansson K, Hayes S, Speck RM, Schmitz KH (2013) Water-based exercise for patients with chronic arm lymphedema: a randomized controlled pilot trial. Am J Phys Med Rehabil 92(4):312–319
Bernas M, Askew R, Cormier JN. Curr Breast Cancer. 2010; 2:53
Cormier JN, Xing Y, Zaniletti I, Askew RL, Stewart BR, Armer JM (2009) Minimal limb volume change has a significant impact on breast cancer survivors. Lymphology 42(4):161–175
Armer JM, Stewart BR (2010) Post-breast cancer lymphedema: incidence increases from 12 to 30 to 60 months. Lymphology 43(3):118–127
DiSipio T, Rye S, Newman B, Hayes S (2013) Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol 14(6):500–515
Khan MA, Srinivasan K, Mohan A, Hardwicke J, Rayatt S (2010) Breast reconstruction and lymphedema. Plast Reconstr Surg 126(3):1118–1119 author reply 119-20
Gartner R, Jensen MB, Kronborg L, Ewertz M, Kehlet H, Kroman N (2010) Self-reported arm-lymphedema and functional impairment after breast cancer treatment–a nationwide study of prevalence and associated factors. Breast 19(6):506–515
Chachaj A, Malyszczak K, Pyszel K, Lukas J, Tarkowski R, Pudelko M et al (2010) Physical and psychological impairments of women with upper limb lymphedema following breast cancer treatment. Psychooncology 19(3):299–305
Hayes SC, Janda M, Cornish B, Battistutta D, Newman B (2008) Lymphedema after breast cancer: incidence, risk factors, and effect on upper body function. J Clin Oncol 26(21):3536–3542
Pinto M, Gimigliano F, Tatangelo F, Megna M, Izzo F, Gimigliano R et al (2013) Upper limb function and quality of life in breast cancer related lymphedema: a cross-sectional study. Eur J Phys Rehabil Med 49(5):665–673
Burckhardt M, Belzner M, Berg A, Fleischer S (2014) Living with breast cancer-related lymphedema: a synthesis of qualitative research. Oncol Nurs Forum 41(4):E220–E237
Shigaki CL, Madsen R, Wanchai A, Stewart BR, Armer JM (2013) Upper extremity lymphedema: presence and effect on functioning five years after breast cancer treatment. Rehabil Psychol 58(4):342–349
Harrington S, Padua D, Battaglini C, Michener LA (2013) Upper extremity strength and range of motion and their relationship to function in breast cancer survivors. Physiother Theory Pract 29(7):513–520
Hack TF, Kwan WB, Thomas-Maclean RL, Towers A, Miedema B, Tilley A et al (2010) Predictors of arm morbidity following breast cancer surgery. Psychooncology 19(11):1205–1212
Helms G, Kuhn T, Moser L, Remmel E, Kreienberg R (2009) Shoulder-arm morbidity in patients with sentinel node biopsy and complete axillary dissection–data from a prospective randomised trial. Eur J Surg Oncol 35(7):696–701
Aerts PD, De Vries J, Van der Steeg AF, Roukema JA (2011) The relationship between morbidity after axillary surgery and long-term quality of life in breast cancer patients: the role of anxiety. Eur J Surg Oncol 37(4):344–349
Kopec JA, Colangelo LH, Land SR, Julian TB, Brown AM, Anderson SJ et al (2013) Relationship between arm morbidity and patient-reported outcomes following surgery in women with node-negative NSABP protocol B-32. J Support Oncol 11(1):22–30
Levy EW, Pfalzer LA, Danoff J, Springer BA, McGarvey C, Shieh CY et al (2012) Predictors of functional shoulder recovery at 1 and 12 months after breast cancer surgery. Breast Cancer Res Treat 134(1):315–324
Dawes DJ, Meterissian S, Goldberg M, Mayo NE (2008) Impact of lymphoedema on arm function and health-related quality of life in women following breast cancer surgery. J Rehabil Med 40(8):651–658
Sagen A, Kaaresen R, Sandvik L, Thune I, Risberg MA (2014) Upper limb physical function and adverse effects after breast cancer surgery: a prospective 2.5-year follow-up study and preoperative measures. Arch Phys Med Rehabil 95(5):875–881
Timperi AW, Ergas IJ, Rehkopf DH, Roh JM, Kwan ML, Kushi LH (2013) Employment status and quality of life in recently diagnosed breast cancer survivors. Psychooncology 22(6):1411–1420
Ancukiewicz M, Russell TA, Otoole J, Specht M, Singer M, Kelada A et al (2011) Standardized method for quantification of developing lymphedema in patients treated for breast cancer. Int J Radiat Oncol Biol Phys 79(5):1436–1443
Ancukiewicz M, Miller CL, Skolny MN, O’Toole J, Warren LE, Jammallo LS et al (2012) Comparison of relative versus absolute arm size change as criteria for quantifying breast cancer-related lymphedema: the flaws in current studies and need for universal methodology. Breast Cancer Res Treat 135(1):145–152
Specht MC, Miller CL, Russell TA, Horick N, Skolny MN, O’Toole JA et al (2013) Defining a threshold for intervention in breast cancer-related lymphedema: what level of arm volume increase predicts progression? Breast Cancer Res Treat 140(3):485–494
Armer JM, Stewart BR (2005) A comparison of four diagnostic criteria for lymphedema in a post-breast cancer population. Lymphat Res Biol 3(4):208–217
Stout Gergich NL, Pfalzer LA, McGarvey C, Springer B, Gerber LH, Soballe P (2008) Preoperative assessment enables the early diagnosis and successful treatment of lymphedema. Cancer 112(12):2809–2819
Armer JM, Radina ME, Porock D, Culbertson SD (2003) Predicting breast cancer-related lymphedema using self-reported symptoms. Nurs Res 52(6):370–379
DE Beaton, Katz JN, Fossel AH, Wright JG, Tarasuk V, Bombardier C (2001) Measuring the whole or the parts? validity, reliability, and responsiveness of the disabilities of the arm, shoulder and hand outcome measure in different regions of the upper extremity. J Hand Ther 14((2):128–146
Lee TS, Kilbreath SL, Sullivan G, Refshauge KM, Beith JM (2007) The development of an arm activity survey for breast cancer survivors using the protection motivation theory. BMC Cancer 8(7):75
Coster S, Poole K, Fallowfield LJ (2001) The validation of a quality of life scale to assess the impact of arm morbidity in breast cancer patients post-operatively. Breast Cancer Res Treat 68(3):273–282
American Physical Therapists Association. Functional training in self-care and in domestic, education, work, community, social, and civic life. In: Guide to Physical Therapist Practice 2014 ed.; 2014
Czerniec SA, Ward LC, Refshauge KM, Beith J, Lee MJ, York S et al (2010) Assessment of breast cancer-related arm lymphedema–comparison of physical measurement methods and self-report. Cancer Invest 28(1):54–62
Hayes S, Cornish B, Newman B (2005) Comparison of methods to diagnose lymphoedema among breast cancer survivors: 6-month follow-up. Breast Cancer Res Treat 89(3):221–226
McLaughlin SA, Wright MJ, Morris KT, Giron GL, Sampson MR, Brockway JP et al (2008) Prevalence of lymphedema in women with breast cancer 5 years after sentinel lymph node biopsy or axillary dissection: objective measurements. J Clin Oncol 26(32):5213–5219
Hayes S, Di Sipio T, Rye S, Lopez JA, Saunders C, Pyke C et al (2011) Prevalence and prognostic significance of secondary lymphedema following breast cancer. Lymphat Res Biol 9(3):135–141
Sagen A, Karesen R, Risberg MA (2009) Physical activity for the affected limb and arm lymphedema after breast cancer surgery. A prospective, randomized controlled trial with two years follow-up. Acta Oncol 48(8):1102–1110
Harrington S, Michener LA, Kendig T, Miale S, George SZ (2014) Patient-reported upper extremity outcome measures used in breast cancer survivors: a systematic review. Arch Phys Med Rehabil 95(1):153–162
Hayes SC, Rye S, Disipio T, Yates P, Bashford J, Pyke C et al (2013) Exercise for health: a randomized, controlled trial evaluating the impact of a pragmatic, translational exercise intervention on the quality of life, function and treatment-related side effects following breast cancer. Breast Cancer Res Treat 137(1):175–186
Quinlan E, Thomas-MacLean R, Hack T, Kwan W, Miedema B, Tatemichi S et al (2009) The impact of breast cancer among Canadian women: disability and productivity. Work 34(3):285–296
Lauridsen MC, Overgaard M, Overgaard J, Hessov IB, Cristiansen P (2008) Shoulder disability and late symptoms following surgery for early breast cancer. Acta Oncol 47(4):569–575
Miedema B, Hamilton R, Tatemichi S, Thomas-Maclean R, Hack TF, Quinlan E et al (2011) Do breast cancer survivors’ post-surgery difficulties with recreational activities persist over time? J Cancer Surviv 5(4):405–412
Hayes SC, Rye S, Battistutta D, DiSipio T, Newman B (2010) Upper-body morbidity following breast cancer treatment is common, may persist longer-term and adversely influences quality of life. Health Qual Life Outcomes 8:92
Jammallo LS, Miller CL, Singer M, Horick NK, Skolny MN, Specht MC et al (2013) Impact of body mass index and weight fluctuation on lymphedema risk in patients treated for breast cancer. Breast Cancer Res Treat 142(1):59–67
McLaughlin SA, Bagaria S, Gibson T, Arnold M, Diehl N, Crook J et al (2013) Trends in risk reduction practices for the prevention of lymphedema in the first 12 months after breast cancer surgery. J Am Coll Surg 216((3):380–389 quiz 511-3
International classification of functioning, disability and health (ICF) [Internet].; 2001 []. Available from: http://www.who.int/classifications/icf/icf_more/en/?sid=Refworks%3ATreadwell%20Library%20at%20MGH&charset=utf-8&__char_set=utf8&genre=article&aulast=World%20Health%20Organization&date=2001&volume=2015&issue=1%2F30&atitle=International%20Classification%20of%20Functioning%2C%20Disability%20and%20Health%20(ICF)&au=World%20Health%20Organization%20&
Acknowledgments
The study described was supported by Award Number R01CA139118 (AGT), Award Number P50CA089393 (AGT) from the National Cancer Institute and the Adele McKinnon Research Fund for Breast Cancer-Related Lymphedema. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health.
Conflict of interest
The authors have no conflict of interests to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
O’Toole, J.A., Ferguson, C.M., Swaroop, M.N. et al. The impact of breast cancer-related lymphedema on the ability to perform upper extremity activities of daily living. Breast Cancer Res Treat 150, 381–388 (2015). https://doi.org/10.1007/s10549-015-3325-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-015-3325-3