Abstract
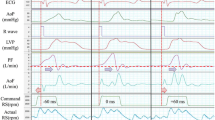
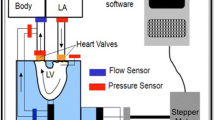
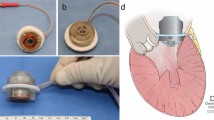
Mitral valve regurgitation (MVR) is common in patients receiving left ventricular assist device (LVAD) support, however the haemodynamic effect of MVR is not entirely clear. This study evaluated the haemodynamic effect of MVR with LVAD support and the influence of inflow cannulation site and LVAD speed modulation. Left atrial (LAC) and ventricular (LVC) cannulation was evaluated in a mock circulation loop with no, mild, moderate and severe MVR with constant speed and speed modulation (±600 RPM) modes. The use of an LVAD relieved pulmonary congestion during severe MVR, by reducing left atrial pressure from 20.5 to 10.8 (LAC) and 11.5 (LVC) mmHg. However, LAC resulted in decreased left ventricular stroke work (−0.08 J), ejection fraction (−7.9%) and higher MVR volume (+12.7 mL) and pump speed (+100 RPM) compared to LVC. This suggests that LVC, in addition to reducing MVR severity, also improves ventricular washout over LAC. LVAD speed modulation in synchrony with ventricular systole reduced MVR volume and increased ejection fraction with LAC and LVC, thus demonstrating the potential benefits of this mode, despite a reduction in cardiac output.



Similar content being viewed by others
References
Aaronson, K. D., H. Patel, and F. D. Pagani. Patient selection for left ventricular assist device therapy. Ann. Thorac. Surg. 75:S29–35, 2003.
Amacher, R., G. Ochsner, and M. Schmid Daners. Synchronized pulsatile speed control of turbodynamic left ventricular assist devices: review and prospects. Artif. Organs 38:867–875, 2014.
British Society of Echocardiography Education Committee. Echocardiography: Guidelines for valve quantification. edited by British Heart Foundation 2011.
Dranishnikov, N., A. Stepanenko, E. V. Potapov, M. Dandel, H. Siniawski, A. Mladenow, M. Hubler, O. Grauhan, Y. Weng, T. Krabatsch, R. Hetzer, and M. Kukucka. Simultaneous aortic valve replacement in left ventricular assist device recipients: single-center experience. Int. J. Artif. Organs 35:489–494, 2012.
Farrar, D. J., K. Bourque, C. P. Dague, C. J. Cotter, and V. L. Poirier. Design features, developmental status, and experimental results with the Heartmate III centrifugal left ventricular assist system with a magnetically levitated rotor. ASAIO J. 53:310–315, 2007.
Gregory, S. D., N. Greatrex, D. Timms, N. Gaddum, M. J. Pearcy, and J. F. Fraser. Simulation and enhancement of a cardiovascular device test rig. J. Simul. 4:34–41, 2010.
Gregory S. D., M. Stevens, D. Timms and M. Pearcy. Replication of the Frank-Starling response in a mock circulation loop. Conf Proc IEEE Eng Med Biol Soc 2011, pp. 6825–6828.
Gregory, S. D., M. C. Stevens, E. Wu, J. F. Fraser, and D. Timms. In vitro evaluation of aortic insufficiency with a rotary left ventricular assist device. Artif. Organs 37:802–809, 2013.
Ising, M. S., M. A. Sobieski, M. S. Slaughter, S. C. Koenig, and G. A. Giridharan. Feasibility of pump speed modulation for restoring vascular pulsatility with rotary blood pumps. ASAIO J. 61:526–532, 2015.
Jelenc, M., B. Jelenc, B. Vrtovec, and I. Knezevic. Mitral regurgitation and axial flow left ventricular assist device: a computer simulation study. ASAIO J. 59:405–409, 2013.
John, R., K. Liao, F. Kamdar, P. Eckman, A. Boyle, and M. Colvin-Adams. Effects on pre- and posttransplant pulmonary hemodynamics in patients with continuous-flow left ventricular assist devices. J. Thorac. Cardiovasc. Surg. 140:447–452, 2010.
John, R., Y. Naka, S. J. Park, C. Sai-Sudhakar, C. Salerno, K. S. Sundareswaran, D. J. Farrar, and C. A. Milano. Impact of concurrent surgical valve procedures in patients receiving continuous-flow devices. J. Thorac. Cardiovasc. Surg. 147:581–589, 2014; (discussion 589).
Kirklin, J. K., D. C. Naftel, F. D. Pagani, R. L. Kormos, L. W. Stevenson, E. D. Blume, M. A. Miller, J. Timothy Baldwin, and J. B. Young. Sixth INTERMACS annual report: A 10,000-patient database. J. Heart Lung Transplant. 33:555–564, 2014.
Kitada, S., T. S. Kato, S. S. Thomas, S. D. Conwell, C. Russo, M. R. Di Tullio, M. Farr, P. C. Schulze, N. Uriel, U. P. Jorde, H. Takayama, Y. Naka, S. Homma, and D. M. Mancini. Pre-operative echocardiographic features associated with persistent mitral regurgitation after left ventricular assist device implantation. J. Heart Lung Transplant. 32:897–904, 2013.
Koelling, T. M., K. D. Aaronson, R. J. Cody, D. S. Bach, and W. F. Armstrong. Prognostic significance of mitral regurgitation and tricuspid regurgitation in patients with left ventricular systolic dysfunction. Am. Heart J. 144:524–529, 2002.
Morgan, J. A., R. J. Brewer, H. W. Nemeh, R. Murthy, C. T. Williams, D. E. Lanfear, C. Tita, and G. Paone. Left ventricular reverse remodeling with a continuous flow left ventricular assist device measured by left ventricular end-diastolic dimensions and severity of mitral regurgitation. ASAIO J. 58:574–577, 2012.
Parikh, K. S., A. K. Mehrotra, M. J. Russo, R. M. Lang, A. Anderson, V. Jeevanandam, B. H. Freed, J. D. Paul, J. Karol, S. Nathan, and A. P. Shah. Percutaneous transcatheter aortic valve closure successfully treats left ventricular assist device-associated aortic insufficiency and improves cardiac hemodynamics. JACC: Cardiovasc. Interv. 6:84–89, 2013.
Pirbodaghi, T., S. Axiak, A. Weber, T. Gempp, and S. Vandenberghe. Pulsatile control of rotary blood pumps: does the modulation waveform matter? J. Thorac. Cardiovasc. Surg. 144:970–977, 2012.
Pirbodaghi, T., C. Cotter, and K. Bourque. Power consumption of rotary blood pumps: pulsatile versus constant-speed mode. Artif. Organs 38(12):1024–1028, 2014.
Pirbodaghi, T., A. Weber, S. Axiak, T. Carrel, and S. Vandenberghe. Asymmetric speed modulation of a rotary blood pump affects ventricular unloading. Eur. J. Cardiothorac. Surg. 43:383–388, 2013.
Robertson, J. O., D. C. Naftel, S. L. Myers, S. Prasad, G. D. Mertz, A. Itoh, F. D. Pagani, J. K. Kirklin, and S. C. Silvestry. Concomitant aortic valve procedures in patients undergoing implantation of continuous-flow left ventricular assist devices: an INTERMACS database analysis. J. Heart Lung Transplant. 34:797–805, 2014.
Russo, M. J., A. Merlo, E. M. Johnson, S. Akhter, S. McCarney, J. Steiman, A. Anderson, and V. Jeevanandam. Transapical approach for mitral valve repair during insertion of a left ventricular assist device. Sci. World J. 2013:925310, 2013.
Saeed, D., T. Kidambi, S. Shalli, B. Lapin, S. C. Malaisrie, R. Lee, W. G. Cotts, and E. C. McGee, Jr. Tricuspid valve repair with left ventricular assist device implantation: Is it warranted? J. Heart Lung Transplant. 30:530–535, 2011.
Salamonsen, R. F., D. G. Mason, and P. J. Ayre. Response of rotary blood pumps to changes in preload and afterload at a fixed speed setting are unphysiological when compared with the natural heart. Artif. Organs 35:E47–53, 2011.
Slaughter, M. S., F. D. Pagani, J. G. Rogers, L. W. Miller, B. Sun, S. D. Russel, R. C. Starling, L. Chen, A. J. Boyle, S. Chillcott, R. M. Adamson, M. S. Blood, M. T. Camacho, K. A. Idrissi, M. Petty, M. Sobieski, S. Wright, T. J. Myers, and D. J. Farrar. Clinical management of continuous-flow left ventricular assist devices in advanced heart failure. J. Heart Lung Transplant. 29:S1–S39, 2010.
Stanfield, J. R., and C. H. Selzman. Pressure sensitivity of axial-flow and centrifugal-flow left ventricular assist devices. Cardiovasc. Eng. Technol. 3:413–423, 2012.
Stepanenko, A., E. V. Potapov, Y. Weng, M. Pasic, T. Krabatsch, and R. Hetzer. Concomitant surgery during ventricular assist device implantation. Ann. Cardiothorac. Surg. 3:630–631, 2014.
Stevens M. C. Automatic Control of Dual LVADs as a BiVAD. PhD Thesis, University of Queensland, 2014.
Stulak, J. M., V. Tchantchaleishvili, N. A. Haglund, M. E. Davis, J. A. Schirger, J. A. Cowger, P. Shah, K. D. Aaronson, F. D. Pagani, and S. Maltais. Uncorrected pre-operative mitral valve regurgitation is not associated with adverse outcomes after continuous-flow left ventricular assist device implantation. J. Heart Lung Transplant. 34:718–723, 2015.
Taghavi, S., E. Hamad, L. Wilson, R. Clark, S. N. Jayarajan, N. Uriel, D. J. Goldstein, H. Takayama, Y. Naka, and A. A. Mangi. Mitral valve repair at the time of continuous-flow left ventricular assist device implantation confers meaningful decrement in pulmonary vascular resistance. ASAIO J. 59:469–473, 2013.
Timms, D., S. Gregory, N. Greatrex, M. J. Pearcy, J. F. Fraser, and U. Steinseifer. A compact mock circulation loop for the in vitro testing of cardiovascular devices. Artif. Organs 35:384–391, 2011.
Timms, D., S. Gregory, P. L. Hsu, B. Thomson, M. Pearcy, K. McNeil, J. Fraser, and U. Steinseifer. Atrial versus ventricular cannulation for a rotary ventricular assist device. Artif. Organs 34:714–720, 2010.
Tuzun, E., I. D. Gregoric, J. L. Conger, K. Golden, R. Jarvik, O. H. Frazier, and K. A. Kadipasaoglu. The effect of intermittent low speed mode upon aortic valve opening in calves supported with a Jarvik 2000 axial flow device. ASAIO J. 51:139–143, 2005.
Wang, T. S., A. F. Hernandez, G. M. Felker, C. A. Milano, J. G. Rogers, and C. B. Patel. Valvular heart disease in patients supported with left ventricular assist devices. Circ. Heart Fail. 7:215–222, 2014.
Westaby, S. Tricuspid regurgitation in left ventricular assist device patients. Eur. J. Cardio-Thorac. Surg. 41:217–218, 2012.
Acknowledgments
The authors would like to recognize the financial assistance provided by The Prince Charles Hospital Foundation (PRO2014-08), the National Health and Medical Research Council Centre for Research Excellence (APP1079421), The University of Queensland, Queensland University of Technology and Griffith University. John F. Fraser acknowledges his fellowship support from the Office of Health and Medical Research, Queensland Health.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Peter E. McHugh oversaw the review of this article.
Rights and permissions
About this article
Cite this article
Gregory, S.D., Stevens, M.C., Wu, E.L. et al. Mitral Valve Regurgitation with a Rotary Left Ventricular Assist Device: The Haemodynamic Effect of Inlet Cannulation Site and Speed Modulation. Ann Biomed Eng 44, 2674–2682 (2016). https://doi.org/10.1007/s10439-016-1579-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-016-1579-5