Abstract
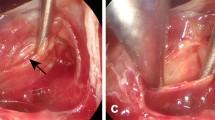
Although some investigators recommended surgical removal of the borders between pituitary adenoma and the surrounding normal pituitary gland, there is so far little documentation of how intensive dissection of the border zone affects the actual clinical remission rate of pituitary adenomas. We investigated the precise histological characteristics of the boundary, using surgical specimens from patients who underwent intensive resection of “microsurgical pseudocapsule” of growth hormone (GH)-secreting pituitary adenomas. Furthermore, we compared the remission rate of acromegaly between subjects with (Group 1) and without (Group 2) intensive resection of microsurgical pseudocapsule in order to correlate the histological complete resection and endocrinological remission. Histologically, most adenomas were in direct contact with normal pituitary gland that formed an increased fibrous component facing the adenoma, without a true histological pseudocapsule. It was impossible to dissect the tumor at exactly the tumor–normal pituitary interface for the whole extent of the pituitary adenoma during surgery, and complete removal of the tumor inevitably included a portion of normal tissue (microsurgical pseudocapsule). The biochemical remission rate was significantly higher in Group 1 than in Group 2 (90.0 vs 61.1%), and Group 1 showed no additional postoperative pituitary hypofunction. The present results suggested that intensive resection of the microsurgical pseudocapsule is essential to accomplish histological and endocrinological total resection of the GH-secreting pituitary adenomas for remission of acromegaly.




Similar content being viewed by others
References
Abe T, Lüdecke DK (1999) Recent primary transnasal surgical outcomes associated with intraoperative growth hormone measurement in acromegaly. Clin Endocrinol (Oxf) 50:27–35
Bergland R (1975) Pathological considerations in pituitary tumors. Prog Neurol Surg 6:62–94
Daita G, Yonemasu Y (1996) Dural invasion and proliferative potential of pituitary adenomas. Neurol Med Chir (Tokyo) 36:211–214
Farnoud M, Kujas M, Derome P, Racadot J, Peillon F, Li J (1994) Interactions between normal and tumoral tissues at the boundary of human anterior pituitary adenomas. An immunohistochemical study. Virchows Arch 424:75–82
Giustina A, Barkan A, Casanueva F, Cavagnini F, Frohman L, Ho K, Valdhuis J, Wass J, Von Werder K, Melmed S (2000) Criteria for cure of acromegaly: a consensus statement. J Clin Endocrinol Metab 85:526–529
Hardy J (1975) Transsphenoidal microsurgical removal of pituitary microadenoma. Prog Neurol Surg 6:200–216
Hashimoto N, Handa H, Yamagami T (1986) Transsphenoidal extracapsular approach to pituitary tumors. J Neurosurg 64:16–20
Heilman CB, Shucart WA, Rebeiz EE (1997) Endoscopic sphenoidotomy approach to the sella. Neurosurgery 41:602–607
Jho H-D, Carrau RL (1997) Endoscopic endonasal transsphenoidal surgery: experience with 50 patients. J Neurosurg 87:44–51
Kawamata T, Iseki H, Ishizaki R, Hori T (2002) Minimally invasive endoscope-assisted endonasal transsphenoidal microsurgery for pituitary tumors: experience with 215 cases comparing with sublabial transsphenoidal approach. Neurol Res 24:259–265
Kawamata T, Iseki H, Shibasaki T, Hori T (2002) Endoscopic augmented reality navigation system for endonasal transsphenoidal surgery to treat pituitary tumors: technical note. Neurosurgery 50:1393–1397
Kawamata T, Kamikawa S, Iseki H, Hori T (2002) Flexible endoscope-assisted endonasal transsphenoidal surgery for pituitary tumors. Minim Invasive Neurosurg 45:208–210
Knosp E, Steiner E, Kitz K, Matula C (1993) Pituitary adenomas with invasion of the cavernous sinus space: a magnetic resonance imaging classification compared with surgical findings. Neurosurgery 33:1992–1998
Koren I, Hadar T, Rappaport ZH, Yaniv E (1999) Endoscopic transnasal transsphenoidal microsurgery versus the sublabial approach for the treatment of pituitary tumors: endonasal complications. Laryngoscope 109:1838–1840
Kreutzer J, Vance M, Lopes M, Laws EJ (2001) Surgical management of GH-secreting pituitary adenomas: an outcome study using modern remission criteria. J Clin Endocrinol Metab 86:4072–4077
Landolt A, Shibata T, Kleihues P (1987) Growth rate of human pituitary adenomas. J Neurosurg 67:803–806
Meij B, Lopes M, Ellegala D, Alden T, Laws EJ (2002) The long-term significance of microscopic dural invasion in 354 patients with pituitary adenomas treated with transsphenoidal surgery. J Neurosurg 96:195–208
Rodziewicz GS, Kelley RT, Kellman RM, Smith MV (1996) Transnasal endoscopic surgery of the pituitary gland: technical note. Neurosurgery 39:189–193
Sautner D, Saeger W (1991) Invasiveness of pituitary adenomas. Pathol Res Pract 187:632–636
Scheithauer B, Kovacs K, Laws EJ, Randall R (1986) Pathology of invasive pituitary tumors with special reference to functional classification. J Neurosurg 65:733–744
Selman W, Laws EJ, Scheithauer B, Carpenter S (1986) The occurrence of dural invasion in pituitary adenomas. J Neurosurg 64:402–407
Shimon I, Cohen Z, Ram Z, Hadani M (2001) Transsphenoidal surgery for acromegaly: endocrinological follow-up of 98 patients. Neurosurgery 48:1239–1245
Teramoto A, Sano K, Osamura R, Watanabe K (1979) Immunohistochemical observations of the pituitary adenomas with the use of enzyme-labelled antibody method—on the residual pituitary gland and “capsule” of the adenoma. Neurol Med Chir (Tokyo) 19:895–902
Teramoto A, Takakura K, Fukushima T (1982) The clinico-pathological study on the boundary of pituitary adenomas. No To Shinkei 34:887–894
Wrightson P (1978) Conservative removal of small pituitary tumors: is it justified by the pathological findings? J Neurol Neurosurg Psychiatry 41:283–289
Zada G, Kelly D, Cohan P, Wang C, Swerdloff R (2003) Endonasal transsphenoidal approach for pituitary adenomas and other sellar lesions: an assessment of efficacy, safety, and patient impressions. J Neurosurg 98:350–358
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kawamata, T., Kubo, O. & Hori, T. Surgical removal of growth hormone-secreting pituitary adenomas with intensive microsurgical pseudocapsule resection results in complete remission of acromegaly. Neurosurg Rev 28, 201–208 (2005). https://doi.org/10.1007/s10143-005-0384-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-005-0384-7