Abstract
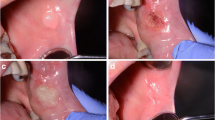
Use of the CO2 laser (λ = 10.6 μm, continuous wave, defocused) is an established procedure for the treatment of premalignant lesions. Through employment of the sp-mode as well as scanners, thermal laser effects can be reduced but, on the other hand, a lesser degree of destruction of dysplastic cells could lead to an increased recurrence rate. The purpose of this study was to prospectively evaluate the recurrence rates resulting from different methods of CO2 laser vaporization. From May 1995 to May, 2005, 145 patients with a total of 148 premalignant lesions of the oral mucosa were treated in a prospective clinical study. Sixty-two lesions in 62 patients were vaporized with the defocused CO2 laser (group 1). In a further 45 lesions (43 patients, group 2), a scanner was additionally employed. In the remaining 41 lesions (40 patients, group 3), vaporization was carried out in the sp-mode in which the scanner was also used. In September, 2005, recurrence rates in the three groups were evaluated. Use of the scanner in sp-mode resulted in the most irregular tissue vaporization. This can be accounted for by the irregular paths of the laser beam and the pulsed delivery of the laser energy. Statistically significant lowest recurrence rates were yielded by the defocused cw-technique followed by the cw-scanner and the sp-mode. These results indicate that for CO2 laser treatment of premalignant lesions of the oral mucosa, the best results can be achieved with the defocused technique. It may be assumed that other methods with lesser penetration of thermal effects (e.g. sp, scanner) do not reach the deeper-lying cells and, consequently, render higher rates of recurrence.

Similar content being viewed by others
References
Barnes L, Eveson JW, Reichart PA, Sidransky D (2005) Pathology and genetics: head and neck tumours. World Health Organization classification of tumours. IARC Press, Lyon
Lodi G, Sardella A, Bez Ch, Demarosi F, Carrassi A (2002) Systematic review of randomized trials for the treatment of oral leukoplakia. J Dent Educ 66:896–902
van der Meij EH, Mast H, van der Waal I (2007) The possible premalignant character of oral lichen planus and oral lichenoid lesions: a prospective five-year follow-up study of 192 patients. Oral Oncol 43:742–748
Sciubba JJ (1999) Improving detection of precancerous and cancerous oral lesions. Computer-assisted analysis of the oral brush biopsy. U.S. Collaborative OralCDx Study Group. J Am Dent Assoc 130:1445–1457
Deppe H, Hillemanns M, Hauck W (2004) Recurrence rates of premalignant lesions after CO2 laser resection. Med Laser Appl 19:55–60
Pindborg JJ, Jolst O, Renstrup G, Roed-Petersen B (1968) Studies in oral leukoplakia: a preliminary report on the period prevalence of malignant transformation in leukoplakia based on a follow up study of 248 patients. J Am Dent Assoc 76:767–771
Silverman S, Gorsky M, Lozada F (1984) Oral Leukoplakia and malignant transformation. A follow-up study of 257 patients. Cancer 53:563–568
Vedtofte P, Holmstrup P, Hjorting-Hansen E, Pindborg JJ (1987) Surgical treatment of premalignant lesions of the oral mucosa. Int J Oral Maxillofac Surg 16:656–664
Kaugars GE, Silverman S, Lovas JGL, Thompson JS, Brandt RB, Singh VN (1996) Use of antioxidant supplements in the treatment of human oral leukoplakia. Oral Surg Oral Med Oral Pathol 81:5–14
Silverman S, Renstrup G, Pindborg JJ (1963) Studies in oral leukoplakias III. Effects of vitamin A comparing clinical, histopathologic, cytologic, and hematologic responses. Acta Odontol Scand 21:271–292
Stich HF, Hornby AP, Mathew B, Sankaranarayanan R, Nair MK (1988) Response of oral leukoplakia to the administration of vitamin A. Cancer 40:93–101
Ribeiro AS, Ribeiro Salles P, da Silva TA, Mesquita RAA (2010) Review of the nonsurgical treatment of oral leukoplakia. Int J Dent. Epub 2010 Feb 23
Schmelzeisen R, Stauch G, Hessel S (1989) Effects of Nd:YAG laser and cryosurgery on the oral mucosa in rabbits. Int J Oral Maxillofac Surg 18:114–116
Horch HH, Gerlach KL (1982) CO2 laser treatment of oral dysplastic precancerous lesions. A preliminary report. Lasers Surg Med 2:179–185
Horch HH, Gerlach KL, Schaefer HE (1986) CO2 laser surgery of oral premalignant lesions. Int J Oral Maxillofac Surg 15:19–24
Roodenburg JL, Panders AK, Vermey A (1991) CO2-laser surgery of oral leukoplakia. Oral Surg Oral Med Oral Pathol 71:670–674
van der Hem PS, Nauta JM, van der Wal JE, Roodenburg JLN (2005) The results of CO2 laser surgery in patients with oral leukoplakia: a 25-year follow-up. Oral Oncol 41:31–37
Deppe H, Horch HH, Henke J, Donath K (2001) Peri-implant care of ailing implants with the carbon dioxide laser. Int J Oral Maxillofac Implants 16:659–667
Hohlweg-Majert B, Deppe H, Metzger MC, Schumm S, Hoefler H, Kesting MR, Holzle F, Wolff KD (2009) Sensitivity and specificity of oral brush biopsy. Cancer Investig 27:293–297
Mattsson U, Jontell M, Holmstrup P (2002) Oral lichen planus and malignant transformation: is a recall of patients justified? Crit Rev Oral Biol Med 13:390–396
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Deppe, H., Mücke, T., Hohlweg-Majert, B. et al. Different CO2 laser vaporization protocols for the therapy of oral precancerous lesions and precancerous conditions: a 10-year follow-up. Lasers Med Sci 27, 59–63 (2012). https://doi.org/10.1007/s10103-011-0910-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-011-0910-5