Abstract
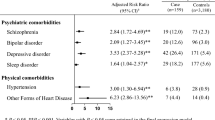
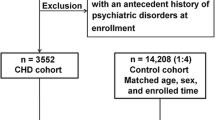
The objective of this study is to assess the prevalence and risk factors for attention-deficit hyperactivity disorder (ADHD) in a large cohort of patients with congenital heart disease (CHD). Patients (n = 695) with CHD who were aged 6–15 years and visited the outpatient clinics in our hospital from June 2015 to May 2017 were enrolled. Their medical records were collected, and the Chinese version of the Swanson, Nolan, and Pelham rating scale (SNAP-IVc) and a questionnaire about neuropsychiatric care-seeking behavior were completed by parents and counselors. Of the 695 patients, the overall prevalence of ADHD was 12.4%, including 3.2% for the combined subtype, 6.8% for the inattentive-predominant subtype, and 2.4% for the hyperactivity/impulsive-predominant subtype. Only the inattention-predominant subtype was significantly more prevalent than in the general population. The prevalence of the inattention-predominant subtype was highest in the patients with cyanotic CHD, high severity index, and in those who had received surgery or cardiopulmonary bypass. Multivariate regression analysis indicated that the risk factors for inattention-related symptoms included postoperative seizure and previous cardiopulmonary bypass (odds ratio: 3.22 and 3.82; P = 0.027 and < 0.001, respectively). Only 58.7% of the patients with probable ADHD ever sought neuropsychiatric care, and only 27% regularly attended neuropsychiatric clinics. The inattention-predominant subtype of ADHD was more prevalent in our CHD patients, especially in those with cyanotic CHD, higher disease severity index, and in those who had undergone a surgical intervention. The percentage of patients receiving regular neuropsychiatric clinic follow-up was low.

Similar content being viewed by others
References
Wu MH, Chen HC, Lu CW, Wang JK, Huang SC, Huang SK (2010) Prevalence of congenital heart disease at live birth in taiwan. J Pediatrics 156(5):782–785
Naef N, Liamlahi R, Beck I, Bernet V, Dave H, Knirsch W, Latal B (2017) Neurodevelopmental profiles of children with congenital heart disease at school age. J Pediatr 188:75–81. https://doi.org/10.1016/j.jpeds.2017.05.073
Marino BS, Lipkin PH, Newburger JW, Peacock G, Gerdes M, Gaynor JW, Mussatto KA, Uzark K, Goldberg CS, Johnson WH Jr, Li J, Smith SE, Bellinger DC, Mahle WT, CoCDitYCoCN AHACHDC, Stroke C (2012) Neurodevelopmental outcomes in children with congenital heart disease: evaluation and management: a scientific statement from the American Heart Association. Circulation 126(9):1143–1172. https://doi.org/10.1161/CIR.0b013e318265ee8a
Subcommittee on Attention-Deficit/Hyperactivity D, Steering Committee on Quality I, Management, Wolraich M, Brown L, Brown RT, DuPaul G, Earls M, Feldman HM, Ganiats TG, Kaplanek B, Meyer B, Perrin J, Pierce K, Reiff M, Stein MT, Visser S (2011) ADHD: clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics 128(5):1007–1022. https://doi.org/10.1542/peds.2011-2654
DeMaso DR, Calderon J, Taylor GA, Holland JE, Stopp C, White MT, Bellinger DC, Rivkin MJ, Wypij D, Newburger JW (2017) Psychiatric disorders in adolescents with single ventricle congenital heart disease. Pediatrics 139:3. https://doi.org/10.1542/peds.2016-2241
Liu YC, Liu SK, Shang CY, Lin CH, Tu C, Gau SS (2006) Norm of the Chinese version of the Swanson, Nolan and Pelham, version IV Scale for ADHD. Taiwan J Psychiatry 20(4):290–304
Gau SS, Shang CY, Liu SK, Lin CH, Swanson JM, Liu YC, Tu CL (2008) Psychometric properties of the Chinese version of the Swanson, Nolan, and Pelham, version IV scale—parent form. Int J Methods Psychiatric Res 17(1):35–44. https://doi.org/10.1002/mpr.237
Swanson JM, Kraemer HC, Hinshaw SP, Arnold LE, Conners CK, Abikoff HB, Clevenger W, Davies M, Elliott GR, Greenhill LL, Hechtman L, Hoza B, Jensen PS, March JS, Newcorn JH, Owens EB, Pelham WE, Schiller E, Severe JB, Simpson S, Vitiello B, Wells K, Wigal T, Wu M (2001) Clinical relevance of the primary findings of the MTA: success rates based on severity of ADHD and ODD symptoms at the end of treatment. J Am Acad Child Adolesc Psychiatry 40(2):168–179
Chen YL, Chen SH, Gau SS (2015) ADHD and autistic traits, family function, parenting style, and social adjustment for Internet addiction among children and adolescents in Taiwan: a longitudinal study. Res Dev Disabil 39:20–31. https://doi.org/10.1016/j.ridd.2014.12.025
Tsai FJ, Liu ST, Lee CM, Lee WT, Fan PC, Lin WS, Chiu YN, Gau SS (2013) ADHD-related symptoms, emotional/behavioral problems, and physical conditions in Taiwanese children with epilepsy. J Formosan Med Assoc 112(7):396–405. https://doi.org/10.1016/j.jfma.2011.08.022
Miller MR, Forrest CB, Kan JS (2000) Parental preferences for primary and specialty care collaboration in the management of teenagers with congenital heart disease. Pediatrics 106(2):264–269
Moons P, Van Deyk K, De Geest S, Gewillig M, Budts W (2005) Is the severity of congenital heart disease associated with the quality of life and perceived health of adult patients? Heart 91(9):1193–1198. https://doi.org/10.1136/hrt.2004.042234
Elliott AC, Reisch JS (2006) Implementing a multiple comparison test for proportions in a 2xc crosstabulation in SAS®. In: Paper presented at the SAS Users Group International Conference
Olsen M, Sorensen HT, Hjortdal VE, Christensen TD, Pedersen L (2011) Congenital heart defects and developmental and other psychiatric disorders: a Danish nationwide cohort study. Circulation 124(16):1706–1712. https://doi.org/10.1161/CIRCULATIONAHA.110.002832
Mahle WT, Clancy RR, Moss EM, Gerdes M, Jobes DR, Wernovsky G (2000) Neurodevelopmental outcome and lifestyle assessment in school-aged and adolescent children with hypoplastic left heart syndrome. Pediatrics 105(5):1082–1089. https://doi.org/10.1542/peds.105.5.1082
Kirshbom PM, Flynn TB, Clancy RR, Ittenbach RF, Hartman DM, Paridon SM, Wernovsky G, Spray TL, Gaynor JW (2005) Late neurodevelopmental outcome after repair of total anomalous pulmonary venous connection. J Thorac Cardiovasc Surg 129(5):1091–1097. https://doi.org/10.1016/j.jtcvs.2004.08.013
Shillingford AJ, Glanzman MM, Ittenbach RF, Clancy RR, Gaynor JW, Wernovsky G (2008) Inattention, hyperactivity, and school performance in a population of school-age children with complex congenital heart disease. Pediatrics 121(4):e759–767. https://doi.org/10.1542/peds.2007-1066
Hansen E, Poole TA, Nguyen V, Lerner M, Wigal T, Shannon K, Wigal SB, Batra AS (2012) Prevalence of ADHD symptoms in patients with congenital heart disease. Pediatr Int 54(6):838–843. https://doi.org/10.1111/j.1442-200X.2012.03711.x
Hovels-Gurich HH, Konrad K, Skorzenski D, Herpertz-Dahlmann B, Messmer BJ, Seghaye MC (2007) Attentional dysfunction in children after corrective cardiac surgery in infancy. Ann Thorac Surg 83(4):1425–1430. https://doi.org/10.1016/j.athoracsur.2006.10.069
Aoki Y, Yoncheva YN, Chen B, Nath T, Sharp D, Lazar M, Velasco P, Milham MP, Di Martino A (2017) Association of white matter structure with autism spectrum disorder and attention-deficit/hyperactivity disorder. JAMA Psychiatry 74(11):1120–1128. https://doi.org/10.1001/jamapsychiatry.2017.2573
Aoki Y, Cortese S, Castellanos FX (2017) Diffusion tensor imaging studies of attention-deficit/hyperactivity disorder: meta-analyses and reflections on head motion. J Child Psychol Psychiatry. https://doi.org/10.1111/jcpp.12778
Batra AS, Alexander ME, Silka MJ (2012) Attention-deficit/hyperactivity disorder, stimulant therapy, and the patient with congenital heart disease: evidence and reason. Pediatr Cardiol 33(3):394–401. https://doi.org/10.1007/s00246-012-0162-6
Jafri S, Ehsan L, Abbas Q, Chand P, Haque UIA (2017) Frequency and outcome of acute neurologic complications after congenital heart disease surgery. J Pediatric Neurosci 12(4):328–331. https://doi.org/10.4103/JPN.JPN_87_17
Desnous B, Lenoir M, Doussau A, Marandyuk B, Beaulieu-Genest L, Poirier N, Carmant L, Birca A, Team Cm (2019) Epilepsy and seizures in children with congenital heart disease: A prospective study. Seizure 64:50–53. https://doi.org/10.1016/j.seizure.2018.11.011
Ghosh S, Philip J, Patel N, Munoz-Pareja J, Lopez-Colon D, Bleiweis M, Winesett SP (2020) Risk factors for seizure and epilepsy in children with congenital heart disease. J Child Neurol. https://doi.org/10.1177/0883073820904912
Mahle WT, Wernovsky G (2001) Long-term developmental outcome of children with complex congenital heart disease. Clin Perinatol 28(1):235–247
Cnota JF, Gupta R, Michelfelder EC, Ittenbach RF (2011) Congenital heart disease infant death rates decrease as gestational age advances from 34 to 40 weeks. J Pediatr 159(5):761–765. https://doi.org/10.1016/j.jpeds.2011.04.020
Shillingford AJ, Wernovsky G (2004) Academic performance and behavioral difficulties after neonatal and infant heart surgery. Pediatr Clin North Am 51(6):1625–1639. https://doi.org/10.1016/j.pcl.2004.07.007
Bellinger DC, Wypij D, Rivkin MJ, DeMaso DR, Robertson RL Jr, Dunbar-Masterson C, Rappaport LA, Wernovsky G, Jonas RA, Newburger JW (2011) Adolescents with d-transposition of the great arteries corrected with the arterial switch procedure: neuropsychological assessment and structural brain imaging. Circulation 124(12):1361–1369. https://doi.org/10.1161/CIRCULATIONAHA.111.026963
Newburger JW, Wypij D, Bellinger DC, du Plessis AJ, Kuban KCK, Rappaport LA, Almirall D, Wessel DL, Jonas RA, Wernovsky G (2003) Length of stay after infant heart surgery is related to cognitive outcome at age 8 years. J Pediatrics 143(1):67–73. https://doi.org/10.1016/s0022-3476(03)00183-5
Gothelf D, Gruber R, Presburger G, Dotan I, Brand-Gothelf A, Burg M, Inbar D, Steinberg T, Frisch A, Apter A, Weizman A (2003) Methylphenidate treatment for attention-deficit/hyperactivity disorder in children and adolescents with velocardiofacial syndrome: an open-label study. J Clin Psychiatry 64(10):1163–1169
Hamrick SEG, Gremmels DB, Keet CA, Leonard CH, Connell JK, Hawgood S, Piecuch RE (2003) Neurodevelopmental outcome of infants supported with extracorporeal membrane oxygenation after cardiac surgery. Pediatrics 111(6):e671–e675
Funding
Cardiac Children Foundation, Taiwan, CCFT-2015-02 and National Health Research Institutes, Taiwan, PH-106-SP-15.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wang, CC., Weng, WC., Chang, LY. et al. Increased prevalence of inattention-related symptoms in a large cohort of patients with congenital heart disease. Eur Child Adolesc Psychiatry 30, 647–655 (2021). https://doi.org/10.1007/s00787-020-01547-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-020-01547-y